Relationship between the ratio of triglyceride high density lipoprotein cholesterol and the risk of hypertension and diabetes in the elder people
-
摘要: 目的 探讨老年人群中甘油三酯高密度脂蛋白胆固醇比值(TG/HDL-C)与高血压及糖尿病患病风险的关系。方法 从三明市基础公共卫生系统中选取参与2023年健康体检的263 859例年龄60岁及以上人群,按照TG/HDL-C基线水平的五分位数将人群分为5组,采用回归分析研究TG/HDL-C与高血压和糖尿病患病风险的关联性。结果 高血压患病率为47.6%,糖尿病患病率为15.1%,高血压和糖尿病共病患病率为10.5%,女性比例为52.7%。TG/HDL-C升高与高血压、糖尿病及高血压和糖尿病共病患病风险增加密切相关。TG/HDL-C最高五分位数组具有较高的高血压、糖尿病及高血压和糖尿病共病患病风险。结论 在老年人群中,TG/HDL-C升高与高血压及糖尿病患病率增加密切相关,控制TG/HDL-C可能对高血压糖尿病的防治具有重要意义。
-
关键词:
- 老年人 /
- 甘油三酯高密度脂蛋白胆固醇比值 /
- 高血压 /
- 糖尿病
Abstract: Objective To explore the relationship between triglyceride high density lipoprotein cholesterol ratio(TG/HDL-C) and the risk of hypertension and diabetes in the elderly.Methods The 263 859 people aged 60 years and above who participated in the physical examination in 2023 were selected from the basic public health system of Sanming City, and were divided into five groups according to the quintile of TG/HDL-C baseline level. Regression analysis was used to study the correlation between TG/HDL-C and the risk of hypertension and diabetes.Results In this study, the prevalence of hypertension was 47.6%, the prevalence of diabetes was 15.1%, the prevalence of hypertension and diabetes was 10.5%, and the proportion of women was 52.7%. The increase of TG/HDL-C is closely related to hypertension, diabetes and the increased risk of hypertension and diabetes comorbidity. TG/HDL-C highest quintile array has a higher risk of hypertension, diabetes, hypertension and diabetes comorbidity.Conclusion In the elderly, the increase of TG/HDL-C is closely related to the increase of the prevalence of hypertension and diabetes. The control of TG/HDL-C may be of great significance for the prevention and treatment of hypertension and diabetes. -

-
表 1 受试者基线临床特征
Table 1. Baseline characteristics of the study population
例(%), X±S 临床特征 TG/HDL-C P 最低五分位数组 第二五分位数组 第三五分位数组 第四五分位数组 最高五分位数组 例数 52 774(20.0) 52 764(20.0) 52 772(20.0) 52 776(20.0) 52 773(20.0) 女性 25 903(49.1) 27 211(51.6) 28 296(53.6) 28 761(54.5) 28 810(54.6) < 0.001 年龄/岁 74.1±6.87 74.0±7.02 73.6±7.02 73.2±6.97 72.3±6.86 < 0.001 腰围/cm 77.4±8.74 80.3±8.98 82.4±8.99 84.2±8.95 86.0±8.67 < 0.001 BMI/(kg/m2) 21.8±3.05 22.7±3.22 23.4±3.26 24.1±3.25 24.7±3.14 < 0.001 收缩压/mmHg 135.5±18.8 136.8±18.8 137.4±18.2 138.4±18.3 139.5±18.2 < 0.001 舒张压/mmHg 78.5±10.3 79.3±10.3 79.9±10.2 80.5±10.2 81.5±10.2 < 0.001 心率/(次/min) 70.0±12.1 71.0±12.1 71.7±12.0 72.1±11.8 73.2±11.8 < 0.001 目前吸烟 10 995(20.8) 10 220(19.4) 9 778(18.5) 9 450(17.9) 9 473(18.0) < 0.001 高血压病 19 453(36.9) 22 575(42.8) 25 362(48.1) 27 663(52.4) 30 550(57.9) < 0.001 糖尿病 4 499(8.53) 6 083(11.5) 7 684(14.6) 9 409(17.8) 12 245(23.2) < 0.001 血糖/(mmol/L) 5.45±1.46 5.61±1.58 5.77±1.76 5.99±1.99 6.39±2.47 < 0.001 总胆固醇/(mmol/L) 4.97±1.12 5.05±1.16 5.12±1.19 5.21±1.21 5.28±1.24 < 0.001 TG/(mmol/L) 0.73±0.21 1.04±0.23 1.35±0.30 1.78±0.40 3.19±1.47 < 0.001 HDL-C/(mmol/L) 1.99±0.77 1.63±0.35 1.47±0.31 1.32±0.27 1.15±0.27 < 0.001 表 2 高血压和(或)糖尿病与TG/HDL-C比值的关系
Table 2. Relationship between hypertension and/or diabetes and TG/HDL-C
模型 未校正模型 校正模型 OR(95%CI) P值 OR(95%CI) P值 高血压 1.28(1.27~1.29) < 0.001 1.10(1.09~1.11) < 0.001 糖尿病 1.33(1.32~1.34) < 0.001 1.09(1.07~1.10) < 0.001 高血压合并糖尿病 1.35(1.33~1.36) < 0.001 1.13(1.12~1.14) < 0.001 注:校正模型中的校正因素为性别、年龄、BMI、收缩压、心率、吸烟、血糖及所属县级。 表 3 高血压和(或)糖尿病与TG/HDL-C不同分组之间的关系
Table 3. Relationship between hypertension and/or diabetes and quintiles of TG/HDL-C
模型 高血压 糖尿病 高血压合并糖尿病 OR(95%CI) P OR(95%CI) P OR(95%CI) P 最低五分位数组 参考 参考 参考 第二五分位数组 1.07(1.04~1.10) < 0.001 1.14(1.09~1.19) < 0.001 1.19(1.13~1.25) < 0.001 第三五分位数组 1.17(1.14~1.20) < 0.001 1.26(1.20~1.32) < 0.001 1.36(1.30~1.44) < 0.001 第四五分位数组 1.25(1.21~1.28) < 0.001 1.36(1.30~1.42) < 0.001 1.54(1.47~1.62) < 0.001 最高五分位数组 1.40(1.36~1.44) < 0.001 1.47(1.41~1.54) < 0.001 1.74(1.66~1.83) < 0.001 注:校正模型中的校正因素为性别、年龄、BMI、收缩压、心率、吸烟、血糖及所属县级。 表 4 其他因素与高血压和(或)糖尿病的关系
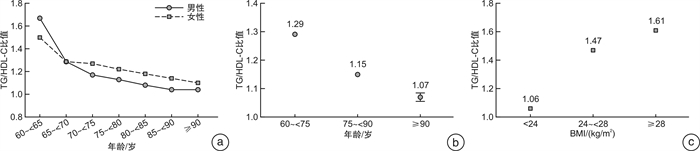
Table 4. The relationship of hypertension and/or diabetes with other risk factors
模型 高血压(125 603例) 糖尿病(39 920例) 高血压合并糖尿病(27 578例) OR(95%CI) P OR(95%CI) P OR(95%CI) P 性别 男性 1.09(1.08~1.11) < 0.001 1.08(1.06~1.09) < 0.001 1.12(1.10~1.14) < 0.001 女性 1.10(1.09~1.11) < 0.001 1.08(1.06~1.10) < 0.001 1.12(1.11~1.14) < 0.001 年龄 < 75岁 1.09(1.08~1.10) < 0.001 1.09(1.07~1.10) < 0.001 1.11(1.10~1.13) < 0.001 75~90岁 1.10(1.08~1.12) < 0.001 1.14(1.12~1.17) < 0.001 1.15(1.13~1.17) < 0.001 ≥90岁 1.06(0.98~1.15) 0.13 1.11(0.98~1.26) 0.091 1.09(0.96~1.24) < 0.001 BMI < 24 kg/m2 1.11(1.10~1.13) < 0.001 1.12(1.10~1.14) < 0.001 1.17(1.15~1.19) < 0.001 24~28 kg/m2 1.08(1.06~1.09) < 0.001 1.05(1.03~1.06) < 0.001 1.09(1.07~1.11) < 0.001 ≥28 kg/m2 1.06(1.04~1.09) < 0.001 1.02(0.99~1.05) 0.22 1.04(1.01~1.08) 0.005 吸烟 否 1.10(1.09~1.11) < 0.001 1.08(1.07~1.09) < 0.001 1.12(1.11~1.14) < 0.001 过去 1.10(1.05~1.16) < 0.001 1.09(1.02~1.16) 0.007 1.12(1.05~1.20) < 0.001 现在 1.11(1.09~1.13) < 0.001 1.09(1.06~1.12) < 0.001 1.13(1.10~1.17) < 0.001 注:校正模型中的校正因素为性别、年龄、BMI、收缩压、心率、吸烟、血糖及所属县级。年龄中位数为72岁,BMI中位数为23.2 kg/m2。 -
[1] 张啸飞, 胡大一, 丁荣晶, 等. 中国心脑血管疾病死亡现况及流行趋势[J]. 中华心血管病杂志, 2012, 40(3): 179-187.
[2] Mahmood SS, Levy D, Vasan RS, et al. The Framingham heart study and the epidemiology of cardiovascular disease: a historical perspective[J]. Lancet, 2014, 383(9921): 999-1008. doi: 10.1016/S0140-6736(13)61752-3
[3] 尹岭, 李亚鹏, 陈景元. 我国心脑血管疾病综合防控研究进展[J]. 中国临床保健杂志, 2019, 22(3): 289-292.
[4] Zhou MG, Wang HD, Zhu J, et al. Cause-specific mortality for 240 causes in China during 1990-2013: a systematic subnational analysis for the global burden of disease study 2013[J]. Lancet, 2016, 387(10015): 251-272. doi: 10.1016/S0140-6736(15)00551-6
[5] 马丽媛, 王增武, 樊静, 等. 《中国心血管健康与疾病报告2021》概要[J]. 中国介入心脏病学杂志, 2022, 30(7): 481-496.
[6] Hu G, Tuomilehto J, Borodulin K, et al. The joint associations of occupational, commuting, and leisure-time physical activity, and the Framingham risk score on the 10-year risk of coronary heart disease[J]. Eur Heart J, 2007, 28(4): 492-498. doi: 10.1093/eurheartj/ehl475
[7] 吕霞霞, 李福辉. 高血压相关危险因素及其与代谢综合征的相关性分析[J]. 现代预防医学, 2016, 43(5): 857-859, 890.
[8] 郭志荣, 胡晓抒, 武鸣, 等. 血脂与高血压关系的前瞻性研究[J]. 中华流行病学杂志, 2009, 30(6): 554-558.
[9] Laaksonen DE, Niskanen L, Nyyssönen K, et al. Dyslipidaemia as a predictor of hypertension in middle-aged men[J]. Eur Heart J, 2008, 29(20): 2561-2568. doi: 10.1093/eurheartj/ehn061
[10] Salazar MR, Carbajal HA, Espeche WG, et al. Relation among the plasma triglyceride/high-density lipoprotein cholesterol concentration ratio, insulin resistance, and associated cardio-metabolic risk factors in men and women[J]. Am J Cardiol, 2012, 109(12): 1749-1753. doi: 10.1016/j.amjcard.2012.02.016
[11] Lu Y, Zhang HB, Lu JP, et al. Prevalence of dyslipidemia and availability of lipid-lowering medications among primary health care settings in China[J]. JAMA Netw Open, 2021, 4(9): e2127573. doi: 10.1001/jamanetworkopen.2021.27573
[12] Zhang M, Deng Q, Wang L, et al. Prevalence of dyslipidemia and achievement of low-density lipoprotein cholesterol targets in Chinese adults: A nationally representative survey of 163, 641 adults[J]. Int J Cardiol, 2018, 260(12): 196-203.
[13] Opoku S, Gan Y, Fu W, et al. Prevalence and risk factors for dyslipidemia among adults in rural and urban China: findings from the China National Stroke Screening and prevention project(CNSSPP)[J]. BMC Public Health, 2019, 19(1): 1500. doi: 10.1186/s12889-019-7827-5
[14] 张梦妮, 李茂婷, 职心乐, 等. 1990—2019年中国动脉粥样硬化心血管病疾病负担变化及其危险因素分析[J]. 中华流行病学杂志, 2021, 42(10): 1797-1803.
[15] Hou QT, Yu C, Li SY, et al. Characteristics of lipid profiles and lipid control in patients with diabetes in a tertiary hospital in Southwest China: an observational study based on electronic medical records[J]. Lipids Health Dis, 2019, 18(1): 13. doi: 10.1186/s12944-018-0945-8
[16] 孙宁玲. 《中国高血压防治指南(2018年修订版)》的重要修改及点评[J]. 中华心血管病杂志(网络版), 2019, 2(1): 1-5.
[17] 中华医学会糖尿病学分会. 中国2型糖尿病防治指南(2020版)[J]. 中华内分泌代谢杂志, 2021, 37(4): 311-398.
[18] Khan K, Quazi S, Bankar NJ, et al. A cross-sectional observational study to assess the efficacy of triglyceride to high-density lipoprotein ratio as a marker of insulin resistance in subjects of central rural India[J]. Cureus, 2024, 16(4): e58612.
[19] Martínez-Marroquín Y, Meaney A, Samaniego-Méndez V, et al. The TG/HDL-c lipid ratio as a cardiovascular risk marker in a Mexican urban middle-class population: do we need a risk score tailored for mexicans?[J]. J Clin Med, 2023, 12(18): 6005. doi: 10.3390/jcm12186005
[20] 李风祥, 单迎光, 郜旌红, 等. TG/HDL-C比值与冠状动脉微循环疾病的相关性研究[J]. 临床心血管病杂志, 2021, 37(11): 1036-1039. https://lcxxg.whuhzzs.com/article/doi/10.13201/j.issn.1001-1439.2021.11.013
[21] 汤百惠, 苏建男, 林先和. TyG指数联合甘油三酯/高密度脂蛋白胆固醇比值对NSTE-ACS患者冠状动脉病变严重程度的预测价值[J]. 医学信息, 2023, 36(17): 88-92, 97.
[22] 汪红平, 王超凡, 高洁, 等. 甘油三酯葡萄糖乘积指数及甘油三酯高密度脂蛋白胆固醇比值对初发急性心肌梗死患者近期预后的影响[J]. 中国糖尿病杂志, 2022, 30(11): 835-842.
[23] Zhou ZJ, Liu Q, Zheng M, et al. Comparative study on the predictive value of TG/HDL-C, TyG and TyG-BMI indices for 5-year mortality in critically ill patients with chronic heart failure: a retrospective study[J]. Cardiovasc Diabetol, 2024, 23(1): 213. doi: 10.1186/s12933-024-02308-w
[24] Zhang FM, Zhang YY, Guo ZG, et al. The association of triglyceride and glucose index, and triglyceride to high-density lipoprotein cholesterol ratio with prehypertension and hypertension in normoglycemic subjects: a large cross-sectional population study[J]. J Clin Hypertens, 2021, 23(7): 1405-1412. doi: 10.1111/jch.14305
[25] Chen YX, Chang ZG, Liu YJ, et al. Triglyceride to high-density lipoprotein cholesterol ratio and cardiovascular events in the general population: a systematic review and meta-analysis of cohort studies[J]. Nutr Metab Cardiovasc Dis, 2022, 32(2): 318-329. doi: 10.1016/j.numecd.2021.11.005
[26] Ide T, Shimano H, Yahagi N, et al. SREBPs suppress IRS-2-mediated insulin signalling in the liver[J]. Nat Cell Biol, 2004, 6(4): 351-357. doi: 10.1038/ncb1111
[27] He S, Wang S, Chen XP, et al. Higher ratio of triglyceride to high-density lipoprotein cholesterol may predispose to diabetes mellitus: 15-year prospective study in a general population[J]. Metabolism, 2012, 61(1): 30-36. doi: 10.1016/j.metabol.2011.05.007
[28] Vergeer M, Brunham LR, Koetsveld J, et al. Carriers of loss-of-function mutations in ABCA1 display pancreatic beta-cell dysfunction[J]. Diabetes Care, 2010, 33(4): 869-874. doi: 10.2337/dc09-1562
[29] Janssen JAMJL. Hyperinsulinemia and its pivotal role in aging, obesity, type 2 diabetes, cardiovascular disease and cancer[J]. Int J Mol Sci, 2021, 22(15): 7797. doi: 10.3390/ijms22157797
[30] Hill MA, Yang Y, Zhang LP, et al. Insulin resistance, cardiovascular stiffening and cardiovascular disease[J]. Metabolism, 2021, 119: 154766. doi: 10.1016/j.metabol.2021.154766
-





 下载:
下载: