Early predictive value of plasma neutrophil gelatinase-associated lipocalin levels for acute kidney injury in patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention
-
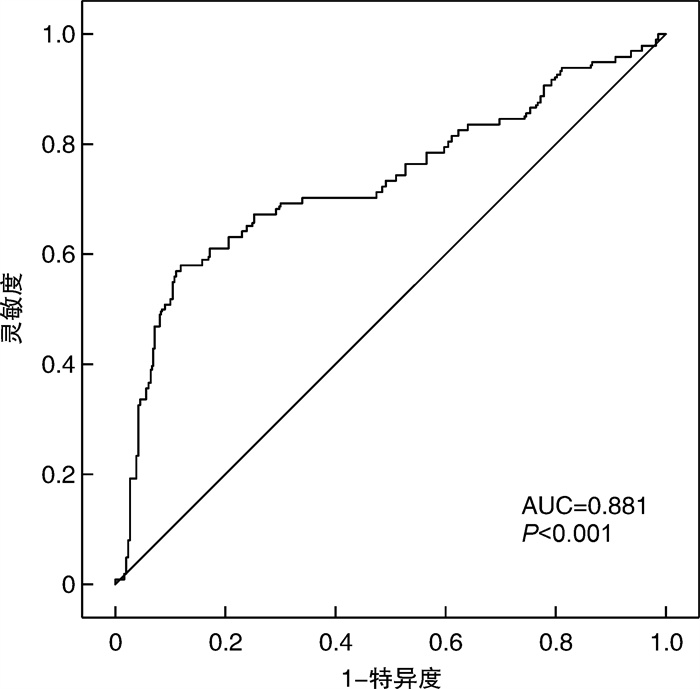
摘要: 目的 探讨血浆中性粒细胞明胶酶相关脂质运载蛋白(NGAL)水平对ST段抬高型心肌梗死(STEMI)患者接受直接经皮冠状动脉介入术(PCI)中急性肾损伤(AKI)的早期预测价值。 方法 连续纳入2017年10月—2019年5月在南京医科大学附属南京医院接受直接PCI治疗的450例STEMI患者。PCI前(0 h)和PCI后24 h测量血浆NGAL水平。AKI根据术后血清肌酐水平升高KDIGO标准定义。应用受试者工作特征曲线(ROC)确定血浆NGAL水平预测AKI的截断值、灵敏度和特异度。 结果 总体AKI发生率为14.2%。和没有发生AKI的患者相比,AKI患者0 h时[(89.6±33.9) ng/mL vs (139.5±38.4) ng/mL,P<0.001]和24 h时[(93.7±35.2) ng/mL vs (167.2±45.3) ng/mL,P<0.001]NGAL水平明显升高。Logistic回归显示,NGAL水平0 h(OR=1.056,95%CI:1.012~1.324,P=0.006)和术后24 h(OR=1.132,95%CI:1.043~1.419,P=0.03)与发生AKI独立相关。ROC曲线显示,NGAL 0 h为124.9 ng/mL时,预测AKI的灵敏度为87.5%,特异度为89.5%(AUC=0.881,95%CI:0.801~0.961,P<0.001)。 结论 NGAL水平升高提示肾小管损伤,与接受直接PCI的STEMI患者发生AKI独立相关。
-
关键词:
- 中性粒细胞明胶酶相关脂质运载蛋白 /
- 急性肾损伤 /
- ST段抬高型心肌梗死 /
- 经皮冠状动脉介入
Abstract: Objective To investigate the early predictive value of plasma neutrophil gelatinase-associated lipocalin(NGAL) levels for acute kidney injury(AKI) in patients with ST-segment elevation myocardial infarction(STEMI) undergoing primary percutaneous coronary intervention(PCI). Methods A total of 450 consecutive patients with STEMI undergoing primary PCI at the Department of Cardiology, Nanjing First Hospital, were enrolled between October 2017 and May 2019. Plasma NGAL levels were measured prior to PCI(0 h) and 24 h afterward. AKI was defined according to the KDIGO criteria, which is based on serum creatinine increase. Receiver-operating characteristic(ROC) methods were used to identify the cut-off value, sensitivity, and specificity of plasma NGAL levels for predicting AKI. Results The overall AKI incidence was 14.2%. NGAL levels were significantly higher in patients with AKI compared to those without AKI, at both 0 h[(89.6±33.9) ng/mL vs(139.5±38.4) ng/mL, P < 0.001]and 24 h[(93.7±35.2) ng/mL vs(167.2±45.3) ng/mL, P < 0.001]. Logistic regression analysis showed that NGAL levels were independently associated with AKI at 0 h(OR=1.056, 95%CI: 1.012-1.324, P=0.006) and 24 h(OR=1.132, 95%CI: 1.043-1.419, P=0.03). ROC curve analysis revealed the cut-off value of NGAL predicted AKI was determined as 124.9 ng/mL with a sensitivity of 87.5% and a specificity of 89.5%(AUC=0.881, 95%CI: 0.801-0.961, P < 0.001). Conclusion Elevated NGAL levels suggest renal tubular damage, and are independently associated with AKI in STEMI patients undergoing primary PCI. -

-
表 1 患者临床基线特征
Table 1. Baseline clinical characteristics
例(%), X±S 项目 无AKI组(386例) AKI组(64例) P 年龄/岁 64.8±12.7 78.6±10.5 0.010 男性 305(79.0) 48(75.0) 0.470 糖尿病 109(28.2) 16(25.0) 0.590 高脂血症 197(51.0) 34(53.1) 0.760 冠心病家族史 96(24.9) 14(21.9) 0.610 吸烟史 185(47.9) 25(39.1) 0.190 高血压 172(44.6) 54(84.5) <0.001 eGFR/(mL/min/1.73 m2) 92.4±20.3 61.5±13.9 <0.001 心肌梗死史 93(24.1) 14(21.9) 0.700 病变支数 0.120 单支 175(45.3) 21(32.8) 两支 97(25.1) 17(26.6) 3支 114(29.6) 26(40.6) 左心室射血分数/% 48.7±11.2 44.5±9.8 0.210 对比剂用量/mL 126.9±38.4 131.7±42.3 0.650 表 2 患者实验室检查指标
Table 2. Laboratory indicators
X±S, M(P25, P75) 项目 无AKI组
(386例)AKI组
(64例)P NGAL/(ng/mL) 0 h 89.6±33.9 139.5±38.4 <0.001 24 h 93.7±35.2 167.2±45.3 <0.001 hs-CRP峰值/(ng/mL) 7.53
(2.80,12.04)5.39
(2.52,11.30)<0.001 肌钙蛋白I/(ng/mL) 30.4±8.9 54.8±11.5 0.020 血红蛋白浓度/(g/L) 14.7±3.9 14.2±3.5 0.780 白细胞计数/(×1012/L) 12.8±4.3 13.7±4.1 0.420 表 3 AKI发生的独立危险因素
Table 3. Independent risk factors for AKI occurrence
项目 模型1 模型2 OR 95%CI P OR 95%CI P 年龄 1.051 0.935~1.223 0.410 1.083 0.964~1.189 0.220 高血压 16.137 2.543~32.148 0.080 12.527 2.145~29.816 0.130 肌钙蛋白I 1.216 0.957~1.562 0.230 1.147 0.973~1.428 0.260 基线eGFR 0.962 1.013~1.387 0.008 0.853 1.015~1.248 0.001 hs-CRP峰值 1.025 0.983~1.424 0.007 1.037 0.971~1.352 0.230 NGAL 0 h 1.056 1.012~1.324 0.006 24 h 1.132 1.043~1.419 0.030 -
[1] Itach T, Banai A, Paran Y, et al. Acute Kidney Injury Recovery Patterns in ST-Segment Elevation Myocardial Infarction Patients[J]. J Clin Med, 2022, 11(8): 2169. doi: 10.3390/jcm11082169
[2] Ye J, Liu C, Deng Z, et al. Risk factors associated with contrast-associated acute kidney injury in ST-segment elevation myocardial infarction patients: a systematic review and meta-analysis[J]. BMJ Open, 2023, 13(6): e070561. doi: 10.1136/bmjopen-2022-070561
[3] Yoon SY, Kim JS, Jeong KH, et al. Acute Kidney Injury: Biomarker-Guided Diagnosis and Management[J]. Medicina(Kaunas), 2022, 58(3): 340.
[4] Balakrishna A, Walco J, Billings FT, et al. Perioperative Acute Kidney Injury: Implications, Approach, Prevention[J]. Adv Anesth, 2023, 41(1): 205-224. doi: 10.1016/j.aan.2023.06.005
[5] Menon S, Symons JM, Selewski DT. Acute Kidney Injury[J]. Pediatr Rev, 2023, 44(5): 265-279. doi: 10.1542/pir.2021-005438
[6] 李秀珍, 谭晓, 高逸冰, 等. 血清中性粒细胞明胶酶相关脂质运载蛋白对对比剂肾病的早期预测价值[J]. 中华老年多器官疾病杂志, 2019, 18(3): 210-213.
[7] Luo P, Ao W, Xiang D, et al. Values of serum neutrophil gelatinase-associated lipocalin and cystatin C after percutaneous coronary intervention for early diagnosis of contrast-induced nephropathy[J]. Afr Health Sci, 2023, 23(3): 593-598.
[8] Thygesen K, Alpert JS, Jaffe AS, et al. Fourth Universal Definition of Myocardial Infarction(2018)[J]. J Am Coll Cardiol, 2018, 72(18): 2231-2264. doi: 10.1016/j.jacc.2018.08.1038
[9] Kidney Disease: Improving Global Outcomes(KDIGO)CKD Work Group. KDIGO 2024 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease[J]. Kidney Int, 2024, 105(4S): S117-S314.
[10] Jha V, Al-Ghamdi SMG, Li G, et al. Global Economic Burden Associated with Chronic Kidney Disease: A Pragmatic Review of Medical Costs for the Inside CKD Research Programme[J]. Adv Ther, 2023, 40(10): 4405-4420. doi: 10.1007/s12325-023-02608-9
[11] Margolis G, Gal-Oz A, Letourneau-Shesaf S, et al. Acute kidney injury based on the KDIGO criteria among ST elevation myocardial infarction patients treated by primary percutaneous intervention[J]. J Nephrol, 2018, 31(3): 423-428. doi: 10.1007/s40620-017-0461-3
[12] Stanski NL, Rodrigues CE, Strader M, et al. Precision management of acute kidney injury in the intensive care unit: current state of the art[J]. Int Care Med, 2023, 49(9): 1049-1061. doi: 10.1007/s00134-023-07171-z
[13] Yang Z, Gong H, Kan F, et al. Association between the triglyceride glucose(TyG)index and the risk of acute kidney injury in critically ill patients with heart failure: analysis of the MIMIC-IV database[J]. Cardiovasc Diabetol, 2023, 22(1): 232. doi: 10.1186/s12933-023-01971-9
[14] Rossiter A, La A, Koyner JL, et al. New biomarkers in acute kidney injury[J]. Crit Rev Clin Lab Sci, 2024, 61(1): 23-44. doi: 10.1080/10408363.2023.2242481
[15] Villa G, Samoni S, Muzzi M, et al. Doppler-Derived Renal Functional Reserve in the Prediction of Postoperative Acute Kidney Injury in Patients Undergoing Robotic Surgery[J]. Anesth Analg, 2024, 139(1): 211-219.
[16] Ma Y, Shen X, Yong Z, et al. Comparison of glomerular filtration rate estimating equations in older adults: A systematic review and meta-analysis[J]. Arch Gerontol Geriatr, 2023, 114: 105107. doi: 10.1016/j.archger.2023.105107
[17] Nurkoç SG, Ünlü S, Şen B, et al. Neutrophil Gelatinase-Associated Lipocalin Level Can Predict Early Organ Damage in Primary Hypertensive Patients: A Pilot Study[J]. Anatol J Cardiol, 2023, 27(8): 513-518.
[18] Xu C, Lin S, Mao L, et al. Neutrophil gelatinase-associated lipocalin as predictor of acute kidney injury requiring renal replacement therapy: A systematic review and meta-analysis[J]. Front Med, 2022, 9: 859318. doi: 10.3389/fmed.2022.859318
[19] Rozenfeld KL, Zahler D, Shtark M, et al. Elevated neutrophil gelatinase-associated lipocalin levels before contrast media administration among ST-segment elevation myocardial infarction patients treated with primary percutaneous coronary intervention[J]. Coron Artery Dis, 2020, 31(2): 118-123. doi: 10.1097/MCA.0000000000000762
[20] Nguyen LS, Spagnoli V, Kerneis M, et al. Evaluation of neutrophil gelatinase-associated lipocalin and cystatin C as biomarkers of acute kidney injury after ST-segment elevation myocardial infarction treated by percutaneous coronary intervention[J]. Arch Cardiovasc Dis, 2019, 112(3): 180-186. doi: 10.1016/j.acvd.2018.11.006
[21] Tecson KM, Erhardtsen E, Eriksen PM, et al. Optimal cut points of plasma and urine neutrophil gelatinase-associated lipocalin for the prediction of acute kidney injury among critically ill adults: retrospective determination and clinical validation of a prospective multicentre study[J]. BMJ Open, 2017, 7(7): e016028. doi: 10.1136/bmjopen-2017-016028
[22] Tan J, Zhang YH, Si J, et al. Incidence, predictors and prognosis of acute kidney injury in acute ST-segment elevation myocardial infarction patients undergoing emergent coronary angiography/primary percutaneous coronary intervention[J]. J Geriatr Cardiol, 2023, 20(2): 139-149. doi: 10.26599/1671-5411.2023.02.004
[23] Zahler D, Rozenfeld KL, Merdler I, et al. Contrast Volume to Glomerular Filtration Ratio and Acute Kidney Injury among ST-Segment Elevation Myocardial Infarction Patients Treated with Primary Percutaneous Coronary Intervention[J]. Cardiorenal Med, 2020, 10(2): 108-115. doi: 10.1159/000504534
[24] de Geus HR, Ronco C, Haase M, et al. The cardiac surgery-associated neutrophil gelatinase-associated lipocalin(CSA-NGAL)score: A potential tool to monitor acute tubular damage[J]. J Thorac Cardiovasc Surg, 2016, 151(6): 1476-1481. doi: 10.1016/j.jtcvs.2016.01.037
[25] Wang W, Xie Y, Huang X, et al. The value of N-terminal pro-brain natriuretic peptide and hs-CRP in predicting acute kidney injury after acute myocardial infarction[J]. Am J Transl Res, 2022, 14(8): 5501-5510.
[26] Watanabe M, Aonuma K, Murohara T, et al. Prevention of Contrast-Induced Nephropathy After Cardiovascular Catheterization and Intervention With High-Dose Strong Statin Therapy in Japan-The PREVENT CINC-J Study[J]. Circ J, 2022, 86(9): 1455-1463. doi: 10.1253/circj.CJ-21-0869
[27] Hammami R, Masmoudi O, Jdidi J, et al. Impact of atorvastatin reload on the prevention of contrast-induced nephropathy in patients on chronic statin therapy: A prospective randomized trial[J]. PloS One, 2023, 18(5): e0270000. doi: 10.1371/journal.pone.0270000
[28] Giacobbe F, Giannino G, Annone U, et al. Impact of statin adherence and interruption within 6 months after ST-segment elevation myocardial infarction(STEMI): Results from the real-world regional registry FAST-STEMI[J]. Int J Cardiol, 2024, 405: 131933. doi: 10.1016/j.ijcard.2024.131933
-




 下载:
下载: