Risk factors and prediction model for delayed extubation of extracorporeal membrane oxygenation in fulminant myocarditis
-
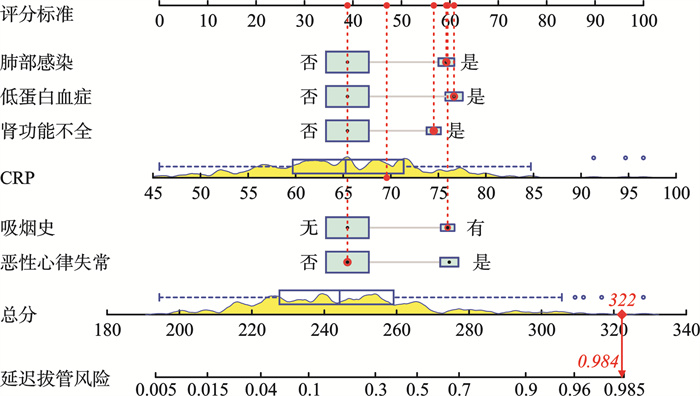
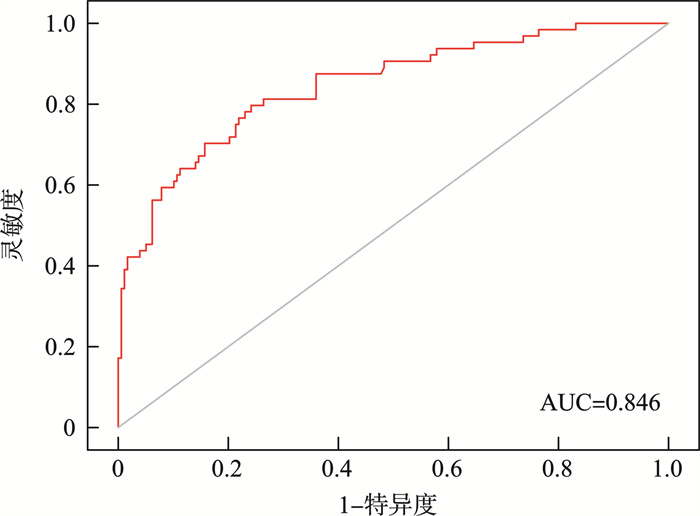
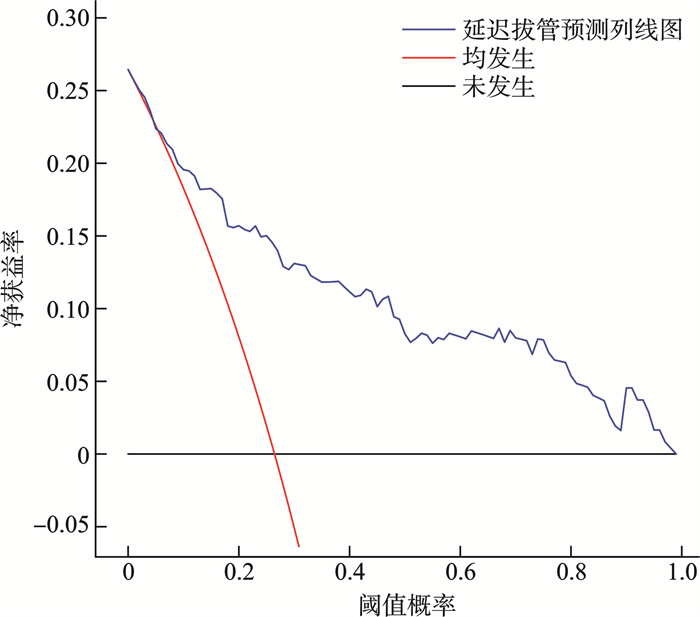
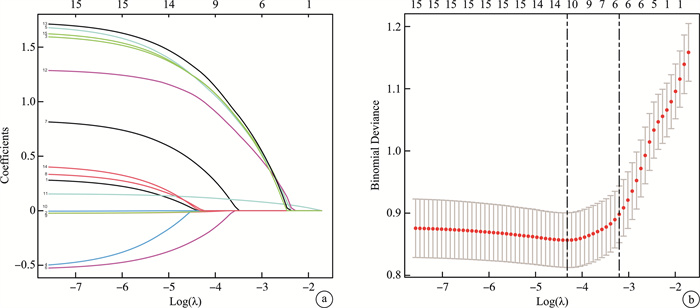
摘要: 目的 探讨暴发性心肌炎体外膜肺氧合延迟拔管的危险因素,并建立其列线图预测模型。 方法 选取2020年1月—2023年11月江苏省人民医院体外生命支持中心及分中心收治的242例暴发性心肌炎接受体外膜肺氧合的患者作为研究对象,根据体外膜肺氧合延迟拔管的发生情况将其分为延迟拔管组(64例)和早期拔管组(178例)。收集两组患者的性别、年龄、恶性心律失常、饮酒史、吸烟史、其他支持治疗、糖尿病、高血压、白细胞计数(WBC)、血小板计数(PLT)、C反应蛋白(CRP)、肾功能不全、低蛋白血症、睡眠质量及肺部感染等资料。采用LASSO和logistic回归分析筛选延迟拔管的预测因素,采用R软件建立延迟拔管的列线图预测模型,并对模型进行验证。 结果 两组性别、年龄、饮酒史、其他支持治疗、糖尿病、高血压、WBC、PLT及睡眠质量等资料均差异无统计学意义;延迟拔管组恶性心律失常、吸烟、肾功能不全、低蛋白血症及肺部感染发生率及CRP水平均显著高于早期拔管组(均P<0.05)。Logistic回归分析显示,恶性心律失常(OR=4.672,95%CI:1.834~11.901,P=0.001)、吸烟史(OR=4.561,95%CI:1.409~14.765,P=0.011)、CRP(OR=1.155,95%CI:1.098~1.215,P<0.001)、肾功能不全(OR=3.695,95%CI:1.178~11.586,P=0.025)、低蛋白血症(OR=5.018,95%CI:1.896~13.285,P=0.001)及肺部感染(OR=4.467,95%CI:1.675~11.910,P=0.003)是延迟拔管的危险因素。基于上述危险因素建立列线图模型,预测延迟拔管的ROC曲线下面积为0.846(95%CI:0.789~0.904);校正曲线的实际值与预测值基本吻合;决策曲线显示阈值概率为1%~100%时,列线图预测延迟拔管的净获益值较高。 结论 恶性心律失常、吸烟史、CRP、肾功能不全、低蛋白血症及肺部感染是暴发性心肌炎患者体外膜肺氧合延迟拔管的危险因素,基于此建立的列线图模型预测延迟拔管的准确性和临床实用性良好。Abstract: Objective To investigate the risk factors of delayed extracorporeal membrane oxygenation(ECMO) extubation in fulminant myocarditis, and to establish a nomogram model for predicting delayed extubation. Methods Two-hundred and forty-two patients with fulminant myocarditis who received ECMO and were admitted to the Extracorporeal Life Support Center and its sub centers of Jiangsu Provincial People's Hospital from January 2020 to November 2023 were selected as the study subjects. Patients were divided into the delayed extubation group(n=64) and the early extubation group(n=178) according to the occurrence of delayed ECMO extubation. Data of gender, age, malignant arrhythmia, drinking history, smoking history, other supportive treatment, diabetes, hypertension, white blood cell count(WBC), platelet count(PLT), C-reactive protein(CRP), renal dysfunction, hypoproteinemia, sleep quality, and pulmonary infection were collected. LASSO and logistic regression analysis were used to screen the risk factors of delayed extubation. R software was used to establish a nomogram model for predicting delayed extubation. The model was validated. Results There were no statistically significant differences in gender, age, drinking history, other supportive treatment, diabetes, hypertension, WBC, PLT, sleep quality, and lung infection between the two groups. The incidence of malignant arrhythmia, smoking history, renal dysfunction, hypoalbuminemia, pulmonary infection, and CRP levels in the delayed extubation group were significantly higher than those in the early extubation group(all P < 0.05). Logistic regression analysis showed that malignant arrhythmia(OR=4.672, 95%CI: 1.834-11.901, P=0.001), smoking history(OR=4.561, 95%CI: 1.409-14.765, P=0.011), CRP(OR=1.155, 95%CI: 1.098-1.215, P < 0.001), renal dysfunction(OR=3.695, 95%CI: 1.178-11.586, P=0.025), hypoalbuminemia(OR=5.018, 95%CI: 1.896-13.285, P=0.001), and pulmonary infection(OR=4.467, 95%CI: 1.675-11.910, P=0.003) were risk factors for delayed extubation. A nomogram model was established based on the above risk factors, the area under the ROC curve for predicting delayed extubation was 0.846(95%CI: 0.789-0.904). The actual value of the calibration curve was basically consistent with the predicted value; When the decision curve shows a threshold probability of 1% to 100%, the model predicted a higher net benefit value for delayed extubation. Conclusion The study identified malignant arrhythmia, smoking history, CRP, renal dysfunction, hypoalbuminemia, and pulmonary infection as risk factors for delayed ECMO extubation in patients with fulminant myocarditis. The nomogram model established based on these factors has good accuracy and clinical practicality in predicting delayed extubation.
-

-
表 1 患者一般资料
Table 1. General data
例(%), X±S 项目 早期拔管组(178例) 延迟拔管组(64例) t/χ2 P 男/女/例 91/87 36/28 0.496 0.481 年龄/岁 50.28±8.16 49.64±7.13 0.556 0.579 恶性心律失常 19(10.67) 18(28.13) 11.069 0.001 饮酒史 16(8.99) 7(10.94) 0.208 0.648 吸烟史 10(5.62) 13(20.31) 11.818 0.001 其他支持治疗 0.236 0.889 临时起搏器 24(13.48) 8(12.50) IABP 20(11.24) 6(9.38) 机械通气 134(75.28) 50(78.13) 糖尿病 24(13.48) 11(17.19) 0.522 0.470 高血压 20(11.24) 9(14.06) 0.357 0.550 WBC/(×109/L) 13.08±2.41 12.84±2.36 0.687 0.493 PLT/(×109/L) 118.34±14.51 116.89±12.83 0.706 0.481 CRP/(mg/L) 63.32±7.53 71.36±9.12 6.828 <0.001 肾功能不全 10(5.62) 14(21.88) 13.926 <0.001 低蛋白血症 19(10.67) 16(25.00) 7.809 0.005 睡眠质量 0.359 0.549 差 15(8.43) 7(10.94) 良好 163(91.57) 57(89.06) 肺部感染 14(7.87) 15(23.44) 10.823 0.001 表 2 Logistic回归分析结果
Table 2. Results of logistic regression analysis
因素 β SE Wald OR 95%CI P 恶性心律失常 1.542 0.477 10.441 4.672 1.834~11.901 0.001 吸烟史 1.518 0.599 6.412 4.561 1.409~14.765 0.011 CRP 0.144 0.026 30.841 1.155 1.098~1.215 <0.001 肾功能不全 1.307 0.583 5.025 3.695 1.178~11.586 0.025 低蛋白血症 1.613 0.497 10.546 5.018 1.896~13.285 0.001 肺部感染 1.497 0.500 8.948 4.467 1.675~11.910 0.003 常数 -11.807 1.853 40.591 -
[1] Menachery SM, Hang Y, Pritchard L, et al. Immune Checkpoint Inhibitor Rechallenge in a Patient With Previous Fulminant Myocarditis[J]. Am J Cardiol, 2023, 199(7): 33-36.
[2] 杨昕宇, 吴倩芸, 吴奕霖, 等. 暴发性心肌炎短期死亡的危险因素及其列线图预测模型的建立及验证: 回顾性分析[J]. 临床心血管病杂志, 2023, 39(3): 225-230. https://lcxxg.whuhzzs.com/article/doi/10.13201/j.issn.1001-1439.2023.03.013
[3] Kociol RD, Cooper LT, Fang JC, et al. Recognition and Initial Management of Fulminant Myocarditis: A Scientific Statement From the American Heart Association[J]. Circulation, 2020, 141(6): e69-e92.
[4] Kobayashi H, Shiohama T, Nakashima M, et al. Fulminant myocarditis following recurrent generalized erythrokeratoderma in a child with a heterozygous GJA1 variant[J]. Am J Med Genet A, 2020, 182(8): 1933-1938. doi: 10.1002/ajmg.a.61626
[5] Catapano D, Tontodonato M, D'Elia S, et al. Fulminant Myocarditis Unmasking Adult-Onset Still's Disease and Desmoplakin Truncation[J]. Circ Cardiovasc Imaging, 2023, 16(8): e015001.
[6] Kawamura T, Toda K, Yoshioka D, et al. Less Invasive Left Ventricular Unloading With Impella May Improve the Clinical Outcomes of Fulminant Myocarditis[J]. ASAIO J, 2023, 69(6): 561-568. doi: 10.1097/MAT.0000000000001907
[7] Zeng C, Song Y, Tang W, et al. Follow-up assessment of myocardial calcification secondary to fulminant myocarditis with computed tomography[J]. J Cardiovasc Comput Tomogr, 2023, 17(1): e1-e3. doi: 10.1016/j.jcct.2022.06.138
[8] Durocher D, El-Hajjaji I, Gilani SO, et al. Bidirectional Ventricular Tachycardia in a Patient with Fulminant Myocarditis Secondary to Cardiac Sarcoid Mimicking Giant Cell Myocarditis[J]. CJC Open, 2021, 3(12): 1509-1512. doi: 10.1016/j.cjco.2021.07.007
[9] Reid TD, Kratzke IM, Dayal D, et al. The role of extracorporeal membrane oxygenation in adult liver transplant patients: A qualitative systematic review of literature[J]. Artif Organs, 2022, 46(4): 578-596. doi: 10.1111/aor.14120
[10] Wu J, Zhang H, Gao Y, et al. Nursing effect of ECMO combined with CRRT in the treatment of fulminant myocarditis: A protocol of randomized controlled trial[J]. Medicine(Baltimore), 2021, 100(3): e24085.
[11] 中华医学会心血管病学分会精准医学学组, 中华心血管病杂志编辑委员会, 成人暴发性心肌炎工作组. 成人暴发性心肌炎诊断与治疗中国专家共识[J]. 中华心血管病杂志, 2017, 45(9): 742-752.
[12] Turgeon PY, Massot M, Beaupré F, et al. Effect of Acute Immunosuppression on Left Ventricular Recovery and Mortality in Fulminant Viral Myocarditis: A Case Series and Review of Literature-Science Direct[J]. CJC Open, 2021, 3(3): 292-302. doi: 10.1016/j.cjco.2020.10.017
[13] Li H, Zhu H, Yang Z, et al. Tissue Characterization by Mapping and Strain Cardiac MRI to Evaluate Myocardial Inflammation in Fulminant Myocarditis[J]. J Magn Reson Imaging, 2020, 52(3): 930-938. doi: 10.1002/jmri.27094
[14] Pettit KA, Selewski DT, Askenazi DJ, et al. Synergistic association of fluid overload and acute kidney injury on outcomes in pediatric cardiac ECMO: a retrospective analysis of the KIDMO database[J]. Pediatr Nephrol, 2023, 38(4): 1343-1353. doi: 10.1007/s00467-022-05708-w
[15] 施霞, 岑福兰, 苏志敏, 等. 体外膜肺氧合在新型冠状病毒肺炎危重型合并暴发性心肌炎患者中的应用[J]. 中华实验和临床病毒学杂志, 2022, 36(4): 448-454.
[16] 钟玉婷, 田克钧, 郭锐, 等. 麻醉诱导前泵注右美托咪定对室性心律失常患者围术期左心室功能、血流动力学的影响[J]. 中国现代医学杂志, 2022, 32(22): 75-79.
[17] 王海霞, 仇焕容, 苏凯, 等. 病态肥胖患者胃减容术后延迟拔管的危险因素分析[J]. 临床麻醉学杂志, 2022, 38(8): 833-836.
[18] 王绍玮, 曾西, 李庆福, 等. 影响持续植物状态合并气管切开患者拔管的相关因素分析[J]. 中华物理医学与康复杂志, 2022, 44(10): 907-911.
[19] 刘卓然, 黎靖, 周宇, 等. 基于HALP评分的列线图模型对肝细胞癌患者肝切除术后预后的预测价值[J]. 临床肝胆病杂志, 2023, 39(7): 1600-1608.
[20] 孙明波, 何光辉, 宁贤远. 上尿路结石微创术后复发的列线图预测模型的建立及预防指导[J]. 皖南医学院学报, 2023, 42(4): 343-346.
-




 下载:
下载: