Risk factors of delayed surgery for acute type A aortic dissection in out-of-hospital referrals
-
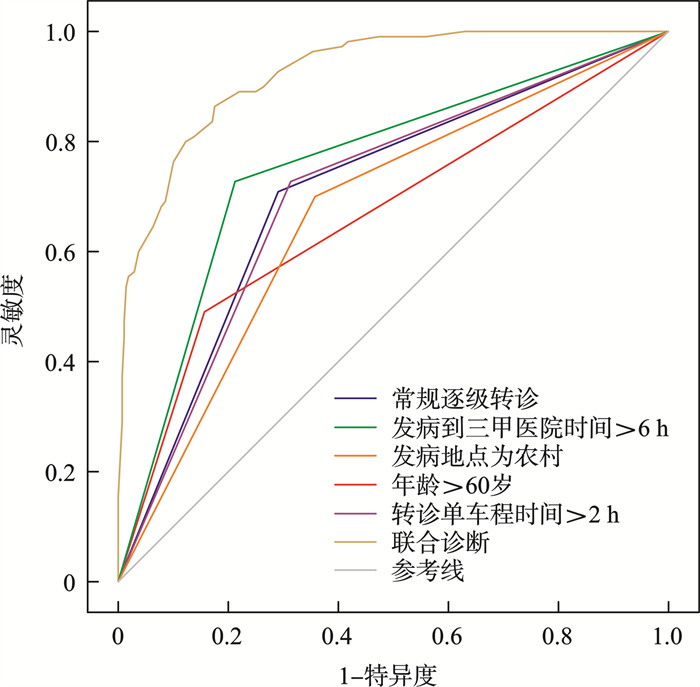
摘要: 目的 探讨院外转诊急性A型主动脉夹层(ATAAD)患者手术延迟的危险因素,并探讨解决手术延迟的方法。 方法 回顾性分析2019年4月—2023年5月外院转诊的378例ATAAD患者的临床资料。根据发病至手术时间是否大于12 h,将患者分为延迟组(110例)和及时组(268例)。比较两组患者病史资料、发病及就诊信息,采用logistic回归分析筛选手术延迟的独立危险因素,并采用受试者工作特征曲线(ROC)对危险因素的预测效能进行判断。 结果 及时组和延时组患者年龄、发病症状、发病地点、发病时间、发病至三甲医院时间、转诊单车程时间、转诊模式相比较均差异有统计学意义(均P<0.05)。Logistic回归分析显示,发病地点为农村(OR=4.66,95%CI:1.99~10.90,P<0.001)、发病到三甲医院时间>6 h(OR=8.65,95%CI:3.80~19.69,P<0.001)、转诊单车程时间>2 h(OR=11.65,95%CI:4.64~29.23,P<0.001)、年龄>60岁(OR=4.88,95%CI:2.01~11.83,P<0.001)、常规逐级转诊(OR=11.35,95%CI:4.53~28.45,P<0.001)是ATAAD患者手术延迟的独立危险因素。ROC分析显示,各危险因素联合预测手术延时的AUC为0.926(95%CI:0.893~0.958,P<0.05),预测灵敏度为89.5%,特异度为78.4%。 结论 ATAAD患者年龄>60岁、发病地点为农村、发病至三甲医院时间>6 h、转诊单车程时间>2 h、常规逐级转诊是手术延迟的独立危险因素。
-
关键词:
- A型主动脉夹层,急性 /
- 手术延迟 /
- 危险因素 /
- 转诊模式
Abstract: Objective To analyze the risk factors for surgical delay in patients with acute type A aortic dissection (ATAAD) referred out of hospital and to identify strategies to minimize surgical delays. Methods Clinical data of 378 cases with ATAAD who were referred to other hospitals from April 2019 to May 2023 were retrospectively analyzed. All patients were divided into the delayed group (n=110) and the timely group (n=268) according to whether the time from onset to operation was longer than 12 h. The preoperative data and referral information of the two groups were compared. Logistic regression analysis was used to identified risk factors for surgical delay, and receiver operating characteristic (ROC) curves were used to evaluate the predictive values of risk factors. Results Patients' age, onset symptoms, onset location, onset time, onset time to Grade-Ⅲ hospital, referral travel time, and referral mode between the two groups were statistically significant(all P < 0.05). Logistic regression analysis showed that the location of onset in rural areas(OR=4.66, 95%CI: 1.99-10.90, P < 0.001), time>6 hours from onset to Grade-Ⅲ hospital(OR=8.65, 95%CI: 3.80-19.69, P < 0.001), single driving time>2 hours for referral(OR=11.65, 95%CI: 4.64-29.23, P < 0.001), age of onset>60 years old(OR=4.88, 95%CI: 2.01-11.83, P < 0.001), and routine progressive referral(OR=11.35, 95%CI: 4.53-28.45, P < 0.001) were independent risk factors for surgical delay in ATAAD patients. ROC analysis showed that the area under the curves of joint risk factors for predicting surgical delay was 0.926(95%CI: 0.893-0.958, P < 0.05), the sensitivity was 89.5%, the specificity was 78.4%. Conclusion Patients' age of onset>60 years old, location of onset in rural areas, time>6 hours from onset to Grade Ⅲ hospital, single driving time>2 hours for referral, and routine progressive referral are independent risk factors for delayed ATAAD surgery.-
Key words:
- type A aortic dissection, acute /
- surgical delay /
- risk factor /
- referral model
-

-
表 1 一般临床资料
Table 1. Clinical data
例(%), X±S 项目 及时组(268例) 延时组(110例) t/χ2 P 男/女/例 233/35 93/17 0.377 0.539 年龄/岁 47.1±11.9 55.2±9.2 6.396 <0.001 发病地点为农村 96(35.8) 77(70.0) 35.342 <0.001 发病时间 周末白天 36(13.4) 17(15.5) 1.259 0.209 晚9点到早6点发病 78(29.1) 49(44.5) 5.179 0.023 社会因素 10(3.7) 8(7.2) 2.157 0.142 中专及以上 84(31.3) 26(23.6) 2.245 0.134 BMI/(kg/m2) 27.1±2.8 26.6±3.2 1.511 0.132 高血压病史 220(82.1) 94(85.5) 0.628 0.428 高血脂病史 158(58.9) 69(62.7) 0.463 0.496 糖尿病病史 30(11.2) 12(10.9) 0.006 0.936 冠心病病史 25(9.3) 17(11.8) 0.535 0.465 吸烟史 163(60.8) 70(63.6) 0.261 0.609 饮酒史 168(62.7) 74(67.3) 1.141 0.285 发病时撕裂样疼痛 214(79.9) 76(69.1) 5.056 0.025 表 2 院前情况
Table 2. Pre-hospital data
例(%), X±S 项目 及时组(268例) 延时组(110例) t/χ2 P 转诊模式 59.641 <0.001 常规逐级转诊 75(27.9) 78(70.9) 点对点转诊 193(72.1) 32(29.1) 发病到三甲医院就诊时间/h 5.2±3.6 8.2±4.5 6.824 <0.001 转诊单车程时间/h 1.8±0.9 2.2±1.3 3.423 <0.001 表 3 多因素logistic回归分析结果
Table 3. Multiple logistic regression analysis results
危险因素 β SE Wals OR(95%CI) P 发病地点为农村 1.54 0.43 3.55 4.66(1.99~10.90) <0.001 发病到三甲医院时间>6 h 2.16 0.42 5.14 8.65(3.80~19.69) <0.001 转诊单车程时间>2 h 2.46 0.47 5.23 11.65(4.64~29.23) <0.001 年龄>60岁 1.58 0.45 3.51 4.88(2.01~11.83) <0.001 常规逐级转诊 2.43 0.47 5.18 11.35(4.53~28.45) <0.001 表 4 ROC曲线分析结果
Table 4. ROC analysis results
危险因素 SE AUC(95%CI) P 常规逐级转诊 0.031 0.707(0.645~0.768) <0.001 发病到三甲医院时间>6 h 0.029 0.769(0.711~0.827) <0.001 发病地点为农村 0.031 0.675(0.614~0.737) <0.001 年龄>60岁 0.032 0.646(0.582~0.709) 0.010 转诊单车程时间>2 h 0.030 0.716(0.656~0.776) <0.001 联合 0.016 0.926(0.893~0.958) <0.001 -
[1] Carrel T, Sundt TM, Kodolitsch YV, et al. Acute aortic dissection[J]. 2023, 401(10378): 773-788.
[2] 蔡治祥, 颜涛, 罗林, 等. 预置包裹法对凝血功能异常的A型主动脉夹层手术的止血效果分析[J]. 临床心血管病杂志, 2023, 39(6): 438-443. https://lcxxg.whuhzzs.com/article/doi/10.13201/j.issn.1001-1439.2023.06.007
[3] Teurneau-Hermansson K, Ede J, Larsson M, et al. Mortality after non-surgically treated acute type A aortic dissection is higher than previously reported[J]. Eur J Cardiothorac Surg, 2024, 65(2): ezae039. doi: 10.1093/ejcts/ezae039
[4] Zhang Q, Peng L, Hu J, et al. Low temperature and temperature decline increase acute aortic dissection risk and burden: A nationwide case crossover analysis at hourly level among 40, 270 patients[J]. Lancet Reg Health West Pac, 2022, 28: 100562.
[5] 孙立忠, 李建荣. 我国Stanford A型主动脉夹层诊疗进展与挑战[J]. 中华外科杂志, 2017, 55(4): 241-244.
[6] Yin J, Liu F, Wang J, et al. Aortic dissection: global epidemiology[J]. Cardiol Plus, 2022, 7(4): 151-161. doi: 10.1097/CP9.0000000000000028
[7] 赵锐, 吴进林, 丘俊涛, 等. 主动脉夹层多中心注册数据库概况[J]. 中华外科杂志, 2020, 58(8): 604-607.
[8] Zhao R, Qiu J, Dai L, et al. Current Surgical Management of Acute Type A Aortic Dissection in China: A Multicenter Registry Study[J]. JACC Asia, 2022, 2(7): 869-878. doi: 10.1016/j.jacasi.2022.08.009
[9] Yoshino H, Akutsu K, Takahashi T, et al. P5607 Clinical characteristics and treatment strategy for acute aortic dissection in Tokyo Acute Aortic Disease Super-Network System[J]. Eur Heart J, 2019, 40(Supplement_1): ehz746.0551. doi: 10.1093/eurheartj/ehz746.0551
[10] 郭津津, 秦历杰, 臧舒婷, 等. 急性心肌梗死患者院前延迟影响因素及干预措施研究进展[J]. 中华急诊医学杂志, 2020, 29(11): 1498-1502.
[11] 蒋敏, 王辉, 李培培, 等. 急性缺血性脑卒中患者院前延迟现状及影响因素分析[J]. 成都医学院学报, 2024, 19(1): 146-152.
[12] 方瑜, 胡涛, 严丽, 等. 我国急性主动脉夹层院前救治延迟现况及原因[J]. 医学与社会, 2022, 35(9): 138-144.
[13] 王葵, 蒋芳, 王显悦, 等. 急性主动脉夹层确诊时间延长的危险因素分析[J]. 血管与腔内血管外科杂志, 2024, 10(1): 56-59, 75.
[14] Toh S, Yew DCM, Choong JJ, et al. Acute type A aortic dissection in-hours versus out-of-hours: A systematic review and meta-analysis[J]. J Card Surg, 2020, 35(12): 3432-3439. doi: 10.1111/jocs.15070
[15] Banceu CM, Banceu DM, Kauvar DS, et al. Acute Aortic Syndromes from Diagnosis to Treatment-A Comprehensive Review[J]. J Clin Med, 2024, 13(5): 1231. doi: 10.3390/jcm13051231
[16] Vaja R, Talukder S, Norkunas M, et al. Impact of a streamlined rotational system for the management of acute aortic syndrome: sharing is caring[J]. Eur J Cardiothorac Surg, 2019, 55(5): 984-989. doi: 10.1093/ejcts/ezy386
[17] Harris KM, Strauss CE, Duval S, et al. Multidisciplinary standardized care for acute aortic dissection: design and initial outcomes of a regional care model[J]. Circ Cardiovasc Qual Outcomes, 2010, 3(4): 424-430. doi: 10.1161/CIRCOUTCOMES.109.920140
[18] Czerny M, Schmidli J, Bertoglio L, et al. Clinical Cases Referring to Diagnosis and Management of Patients With Thoracic Aortic Pathologies Involving the Aortic Arch: A Companion Document of the 2018 European Association for Cardio-Thoracic Surgery(EACTS)and the European Society for Vascular Surgery(ESVS)Expert Consensus Document Addressing Current Options and Recommendations for the Treatment of Thoracic Aortic Pathologies Involving the Aortic Arch[J]. Eur J Vasc Endovasc Surg, 2019, 57(3): 452-460. doi: 10.1016/j.ejvs.2018.12.011
[19] Andersen ND, Ganapathi AM, Hanna JM, et al. Outcomes of acute type a dissection repair before and after implementation of a multidisciplinary thoracic aortic surgery program[J]. J Am Coll Cardiol, 2014, 63(17): 1796-1803. doi: 10.1016/j.jacc.2013.10.085
[20] Vendramin I, Lechiancole A, Piani D, et al. Influence of a regional network combined with a systematic multidisciplinary approach on the outcomes of patients with acute type A aortic dissection[J]. Int J Cardiol, 2023, 391: 131278. doi: 10.1016/j.ijcard.2023.131278
[21] 中华人民共和国国家卫生健康委员会. 2021年我国卫生健康事业发展统计公报[J]. 中国实用乡村医生杂志, 2022, 29(9): 1-11.
[22] 中国心胸血管麻醉学会心血管麻醉分会. Stanford A型主动脉夹层外科手术麻醉中国专家临床路径管理共识(2017)[J]. 临床麻醉学杂志, 2018(10): 1009-1013.
[23] 危重症患者院际转运专家共识组, 国家急诊专业质控中心. 危重症患者院际转运专家共识[J]. 中华急诊医学杂志, 2022, 31(1): 17-23.
-




 下载:
下载: