Analysis of hemostatic effect of preset wrapping technique on Type A aortic dissection with abnormal coagulation
-
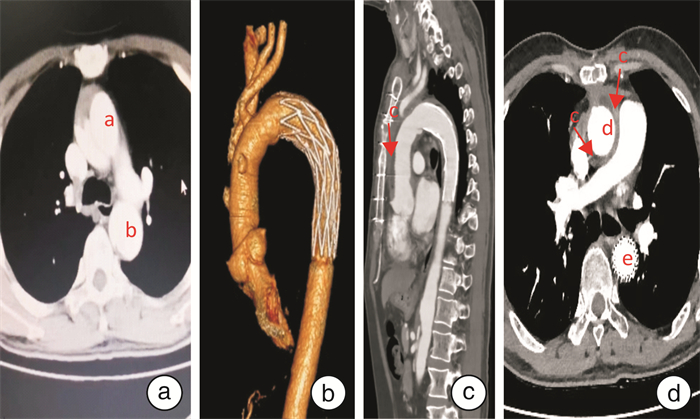
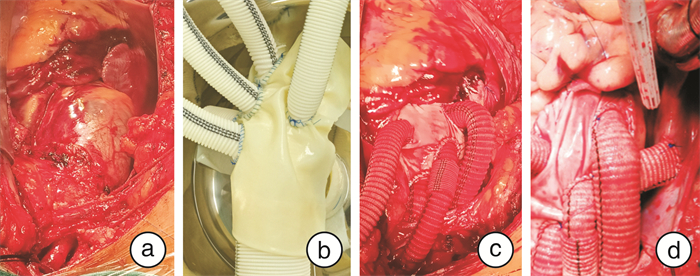
摘要: 目的 探讨采用预置牛心包包裹-右心分流法对伴凝血功能异常的A型主动脉夹层(AAD)手术的止血效果及早期疗效。方法 回顾性分析2018年1月—2022年9月于南部战区总医院心脏外科中心行全弓置换手术的患者399例,术前伴凝血功能异常AAD患者78例,根据术前是否采用预置牛心包包裹法止血进行分组,其中预置包裹组23例,对照组55例。全组内科凝血异常治疗策略参考美国2017 EACTS/EACTA(成人心脏手术患者血液管理指南)对症治疗,预置组均采用预置牛心包包裹-右心分流法止血,对照组止血先尝试主动脉人工血管“裸奔”,必要时加牛心包或自体心包补片包裹分流止血。比较分析两组患者术前一般资料及凝血异常指标情况、手术情况、输血量及凝血药物使用情况及术后早期恢复情况。结果 全组AAD伴凝血功能异常患者均完成外科手术操作。①术前情况:两组患者年龄、发病时间、高血压例数、肝功能异常情况及凝血相关异常指标无明显差异;②术中情况:两组行Bentall术(带主动脉瓣人工血管升主动脉替换术)、心脏停搏时间无明显统计学差异,与对照组相比,预置组体外循环时间[(291.5±56.8) min vs (223.7±45.3) min,P < 0.001]、手术时间较短[(495.5±81.3) min vs (380.6±65.8) min,P < 0.001];③输血量及凝血药物使用情况:与对照组相比,预置组输注血液制品(浓缩红细胞、新鲜冰冻血浆和血小板)及使用凝血相关药物(凝血酶原复合物、纤维蛋白原和重组人凝血七因子较少)(P < 0.05);④术后恢复情况:与对照组比较,预置组患者术后24 h纵隔引流量较少、ICU留滞时间较短(P < 0.05),院内死亡例数、机械通气时间、再次开胸止血、纵隔感染例数、床旁血滤治疗例数减少,但无统计学差异(P>0.05)。结论 预置牛心包包裹止血法应用于伴凝血功能异常的AAD手术基本不增加主动脉阻壁时间,可减少体外循环辅助时间及手术时间,减少术后出血、输血及止血药物使用量,继而有助于患者术后早期恢复。Abstract: Objective To explore the hemostatic effect and early clinical effect of bovine pericardium wrapping-right atrial shunt for type A aortic dissection(AAD) with abnormal coagulation before operation.Methods A total of 399 AAD patients who underwent total arch replacement in the Cardiac Surgery Center of General Hospital of Southern Theater Command from January 2018 to September 2022 were retrospectively analyzed, and 78 patients with preoperative coagulation dysfunction were enrolled and divided into preset bovine pericardium wrapping group(n=23) and control group(n=55). All patients treatment strategy for internal coagulation abnormalities was based on the results of blood coagulation function, and by referring to the 2017 EACTS/EACTA(Guidelines for Blood Management of Adult Heart Surgery Patients) of the United States for symptomatic treatment, All patients in the preset group were treated with preset bovine pericardium wrapped and right heart shunt to prevent or decrease bleeding, while the control group was first tried to artificial aortic vessels "streak-running", and bovine pericardium or autologous pericardium patch was wrapped and shunt to prevent or decrease bleeding if necessary. The preoperative general data, abnormal coagulation indicators, surgical conditions, blood transfusion volume, coagulation drug use, and early postoperative recovery of the two groups were compared and analyzed.Results All AAD patients completed surgical procedures. ①Preoperative conditions: There was no significant difference between the two groups in age, onset time, number of hypertension cases, abnormal liver function and coagulation related abnormal indicators; ②Intraoperative conditions: There was no significant difference between the two groups in the proportion of Bentall operation and cardiac arrest time(P>0.05). Compared with the control group, preset pericardium group had shorter the time of cardiopulmonary bypass and operation(P < 0.001); ③Blood transfusion volume and use of coagulation drugs: compared with the control group, preset pericardium group received less blood products(concentrated red blood cells, fresh frozen plasma and platelets) and coagulation related drugs(prothrombin complex, fibrinogen, and recombinant activated factor Ⅶ)(P < 0.05); ④Postoperative recovery: Compared with the control group, the patients in the preset pericardium group had less 24 hours postoperative mediastinal drainage volume(P < 0.05), shorter ICU retention time, higher hospital deaths(P < 0.05), and mechanical ventilation time, hospital death, re-thoracotomy for bleeding, mediastinal infection, bedside hemofiltration treatment were reduced in the preset group, but there was no statistically significant difference(P>0.05).Conclusion The application of the hemostatic method of preset pericardium wrapping in the operation of type A aortic dissection with abnormal coagulation function does not increase the operation time, and can reduce the auxiliary time of cardiopulmonary bypass and the operation time, reduce the postoperative bleeding, blood transfusion and the use of hemostatic drugs, and thus contribute to the early recovery of patients after operation. However, future large sample sized studies are warranted to thoroughly examine the clinical efficacy of this preset wrapping technique.
-

-
表 1 术前一般临床资料
Table 1. Preoperative clinical data
例(%), X±S 项目 预置组(23例) 对照组(55例) t/χ2 P 男/女/例 20/3 47/8 0.030 0.862 年龄/岁 49.1±11.9 48.5±12.7 0.194 0.847 BMI/(kg/m2) 27.3±2.7 26.6±3.4 0.877 0.383 发病时间/h 19.5±10.9 17.6±9.4 0.776 0.440 高血压病史 19(82.6) 47(85.5) 0.101 0.751 肝功能异常 18(78.3) 44(80.0) 0.030 0.862 表 2 两组患者术前凝血异常情况
Table 2. Abnormalities of blood coagulation before operation in two groups
例(%) 项目 预置组(23例) 对照组(55例) t/χ2 P ASA 5(21.7) 13(23.6) 0.033 0.856 DAPT 6(26.1) 14(25.5) 0.003 0.953 VKA 4(17.4) 7(12.7) 0.291 0.589 NOAC 1(4.3) 2(3.6) 0.222 0.881 Fib < 1.5 g/L 6(26.1) 16(29.1) 0.788 0.072 PLT < 50×109/L 4(17.4) 9(16.4) 0.912 0.012 注:ASA:阿司匹林;DAPT:双联抗血小板;VKA:维生素拮抗剂-华法林;NOAC:新型口服抗凝药物;Fib:纤维蛋白原;PLT:血小板计数。 表 3 两组患者术前凝血异常指标
Table 3. Indicators of abnormal blood coagulation before operation in two groups
例(%) 项目 预置组(23例) 对照组(55例) t/χ2 P Fib/(g/L) 2.8±0.7 2.6±0.8 1.043 0.300 INR 1.4±0.8 1.3±0.9 0.462 0.646 MA值 51.1±10.8 53.3±11.7 0.774 0.441 PLT/(×109/L) 125.7±98.2 130.5±93.2 0.204 0.839 K时间/min 2.8±1.1 3.1±0.9 1.256 0.213 注:INR:国际标准化比值;MA值:最大血凝块硬度。 表 4 手术相关临床数据
Table 4. Intraoperative clinical data
例(%), X±S 项目 预置组(23例) 对照组(55例) t/χ2 P 手术时间/min 380.6±65.8 495.5±81.3 7.356 0.000 体外循环时间/min 223.7±45.3 291.5±56.8 5.082 0.000 心脏停搏时间/min 109.6±38.5 106.8±36.3 0.305 0.761 Bentall术 6(26.1) 13(23.6) 0.053 0.818 表 5 输血量及凝血药物使用情况
Table 5. Data of blood products and coagulants
X±S 项目 预置组(23例) 对照组(55例) t/χ2 P PRBC/mL 488.4±390.1 815.3±739.9 2.001 0.049 FFP/mL 416.5±299.1 746.1±703.4 2.161 0.034 PLT/U 0.8±0.4 1.1±0.6 2.198 0.031 PCC/KIU 18.3±5.2 22.8±9.1 2.219 0.029 rFⅦa/KIU 18.7±8.9 35.1±11.5 6.109 0.000 Fib/g 1.9±1.1 3.2±1.9 3.066 0.003 表 6 术后恢复相关指标
Table 6. Postoperative recovery related clinical data
例(%), X±S 项目 预置组(23例) 对照组(55例) t/χ2 P 术后24h引流量/mL 610±299 1 180±458 5.488 0.000 再次开胸止血 2(8.7) 8(14.6) 0.497 0.481 ICU时间/h 105.3±39.4 129.5±43.9 2.286 0.025 血滤治疗 5(21.7) 14(25.5) 0.122 0.727 机械通气时间/h 31.4±32.5 43.2±38.1 1.299 0.198 纵隔感染 5(21.7) 9(16.4) 0.318 0.573 院内死亡 2(8.7) 7(12.8) 0.258 0.611 -
[1] 邹坤, 魏大闯, 李文华, 等. 手术救治ECMO辅助下的急性Stanford A型主动脉夹层致心源性休克伴主动脉缩窄患者1例[J]. 临床心血管病杂志, 2022, 38(11): 926-928. https://lcxxg.whuhzzs.com/article/doi/10.13201/j.issn.1001-1439.2022.11.015
[2] Lin CY, Wu MY, Tseng CN, et al. Delayed sternal closure for intractable bleeding after acute type A aortic dissection repair: outcomes and risk factors analyses[J]. J Cardiothoracic Surgery, 2022, 17(1): 184. doi: 10.1186/s13019-022-01946-z
[3] Zindovic I, Sjögren J, Bjursten H, et al. The coagulopathy of acute type a aortic dissection: a prospective, observational study[J]. J Cardiothoracic Vascular Anesthesia, 2019, 33(10): 2746-2754. doi: 10.1053/j.jvca.2019.02.013
[4] Li M, Xu S, Yan Y, et al. Association of biomarkers related to preoperative inflammatory and coagulation with postoperative in-hospital deaths in patients with type A acute aortic dissection[J]. Scientific Reports, 2021, 11(1): 18775. doi: 10.1038/s41598-021-98298-w
[5] Bhaskar B, Dulhunty J, Mullany DV, et al. Impact of blood product transfusion on short and long-term survival after cardiac surgery: more evidence[J]. Annals Thoracic Surgery, 2012, 94(2): 460-467. doi: 10.1016/j.athoracsur.2012.04.005
[6] 李书闻, 杨彦伟, 卢家凯, 等. 急性Stanford A型主动脉夹层术后凝血功能障碍危险因素分析[J]. 中国胸心血管外科临床杂志, 2018, 25(8): 670-675. https://www.cnki.com.cn/Article/CJFDTOTAL-ZXYX201808006.htm
[7] 史泽鹏, 何学志, 庄熙晶, 等. 扩大外膜内翻并翻转吻合与主动脉包裹后右房分流技术处理A2型夹层根部的近期疗效对比[J]. 临床心血管病杂志, 2022, 38(3): 210-215. doi: 10.13201/j.issn.1001-1439.2022.03.010 https://lcxxg.whuhzzs.com/article/doi/10.13201/j.issn.1001-1439.2022.03.010
[8] Chen LW, Wu XJ, Dai XF. Transverse Pericardial Sinus Closure in Acute Type A Aortic Dissection Operation[J]. Annals Thoracic Surgery, 2017, 104(4): e351-e353. doi: 10.1016/j.athoracsur.2017.06.035
[9] 刘胜中, 黄克力, 谭今. 右心房分流术在主动脉根部手术中的临床应用[J]. 四川医学, 2013, 34(4): 452-454. doi: 10.3969/j.issn.1004-0501.2013.04.009
[10] 蔡治祥, 张卫达, 车强, 等. 伴凝血功能异常的A型主动脉夹层手术及治疗策略[J]. 临床心血管病杂志, 2019, 35(5): 463-467. doi: 10.13201/j.issn.1001-1439.2019.05.017
[11] Boer C, Meesters MI, Milojevic M, et al. 2017 EACTS/EACTA Guidelines on patient blood management for adult cardiac surgery[J]. J Cardiothoracic Vascular Anesthesia, 2018, 32(1): 88-120. doi: 10.1053/j.jvca.2017.06.026
[12] Guan X, Li J, Gong M, et al. The hemostatic disturbance in patients with acute aortic dissection: A prospective observational study[J]. Medicine, 2016, 95(36): e4710. doi: 10.1097/MD.0000000000004710
[13] Boldyrev SY, Barbukhatty KO, Porhanov VA. Surgical Treatment of Acute Type A Aortic Dissection with 18-Litre Bleeding[J]. Aorta(Stamford, Conn), 2021, 9(1): 30-32. http://www.thieme-connect.com/products/ejournals/abstract/10.1055/s-0041-1722897
[14] 孙立忠, 李建荣. 我国Stanford A型主动脉夹层诊疗进展与挑战[J]. 中华外科杂志, 2017, 55(4): 241-244. https://www.cnki.com.cn/Article/CJFDTOTAL-ZOGU201906014.htm
[15] Guan XL, Wang XL, Liu YY, et al. Changes in the hemostatic system of patients with acute aortic dissection undergoing aortic arch surgery[J]. Annals Thoracic Surgery, 2016, 101(3): 945-951. doi: 10.1016/j.athoracsur.2015.08.047
[16] Galea J, Manché A. Methodsof hemorrhage control from the aorta after repair of a dissected aortic aneurysm[J]. Annals Thoracic Surgery, 2017, 103(3): e299-e300. doi: 10.1016/j.athoracsur.2016.08.105
[17] LIU Y, HAN L, LI J, et al. Consumption coagulopathy in acute aortic dissection: principles of management[J]. J Cardiothoracic Surgery, 2017, 12(1): 50. doi: 10.1186/s13019-017-0613-5
[18] Kao CL, Chang JP. Perigraft-to-right atrial shunt for aortic root hemostasis[J]. Texas Heart Institute journal, 2003, 30(3): 205-207. http://europepmc.org/articles/PMC197318/pdf/20030900s00008p205.pdf
[19] 喻雪飞, 董柱, 张本, 等. 急性Stanford A型主动脉夹层术后感染的危险因素分析及预防策略[J]. 临床心血管病杂志, 2021, 37(8): 758-763. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXB202108017.htm
[20] 李冬海, 曹玉珏, 贺立新, 等. 心脏术后切口感染累及心外牛心包补片患者的治疗[J]. 感染、炎症、修复, 2014, 15(2): 112-113. https://www.cnki.com.cn/Article/CJFDTOTAL-GRYX201402020.htm
[21] Kelly YP, Waikar SS, Mendu ML. When to stop renal replacement therapy in anticipation of renal recovery in AKI: The need for consensus guidelines[J]. Seminars Dialysis, 2019, 32(3): 205-209. http://doc.paperpass.com/foreign/rgArti2019136640734.html
[22] Lin ZH, Zuo L. When to initiate renal replacement therapy: The trend of dialysis initiation[J]. World J Nephrology, 2015, 4(5): 521-527. http://www.pubmedcentral.nih.gov/picrender.fcgi?artid=PMC4635372&blobtype=pdf
[23] 陈志远, 李庆国. 国际主动脉夹层注册数据库的研究进展[J]. 东南国防医药, 2021, 23(3): 287-292. https://www.cnki.com.cn/Article/CJFDTOTAL-DNGY202103014.htm
[24] 罗明尧, 舒畅, 陈冬, 等. 以主动脉夹层和腹主动脉瘤为例谈中国主动脉疾病诊疗研究现状[J]. 临床外科杂志, 2021, 29(12): 1196-1199. https://www.cnki.com.cn/Article/CJFDTOTAL-LCWK202112031.htm
-




 下载:
下载: