A comparison of the short-term efficacy of the extended adventitial inversion with graft eversion anastomosis and aortic wall wrapping graft with right atrial shunt anastomosis in root remodeling of A2-type aortic dissection
-
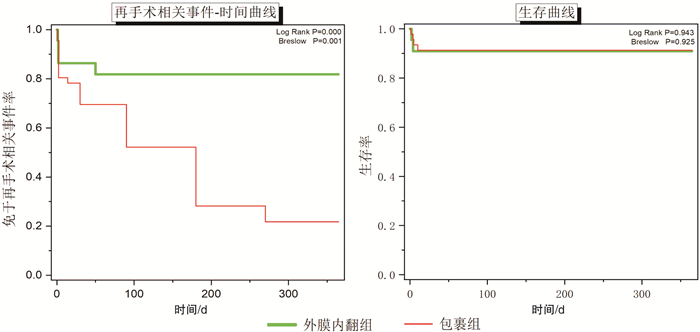
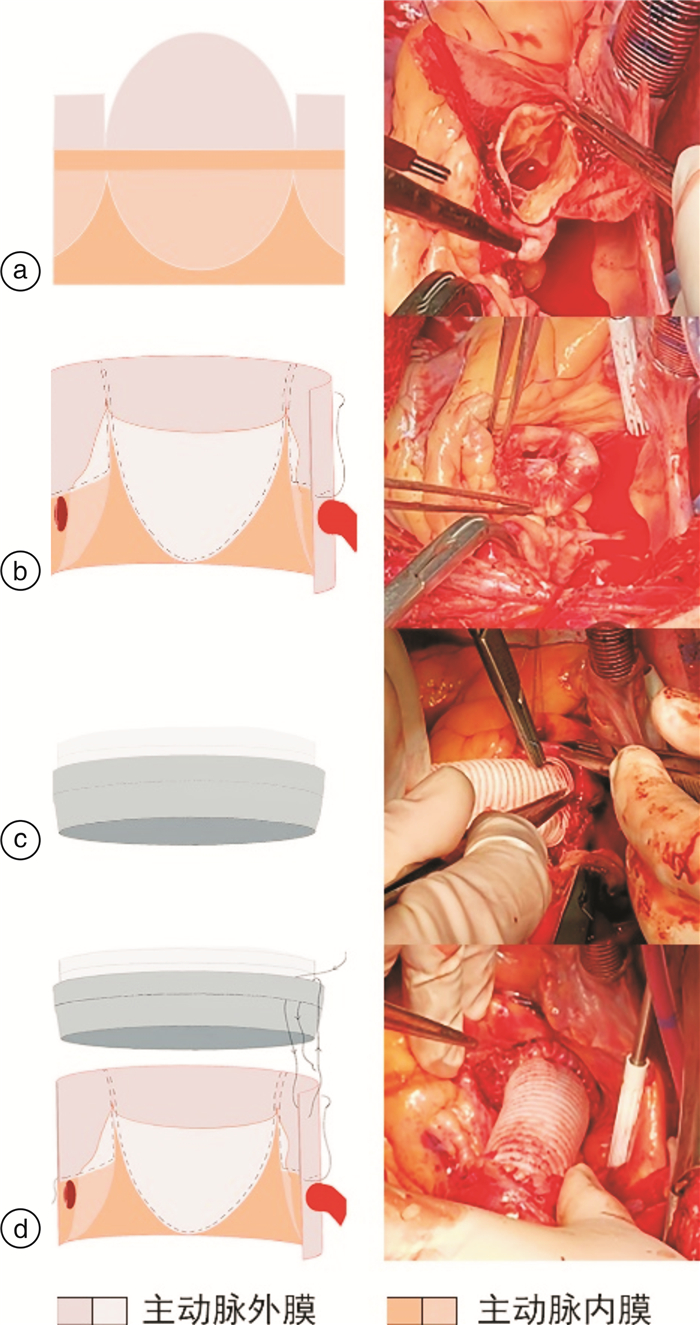
摘要: 目的 对比扩大外膜内翻并翻转吻合与主动脉包裹后右房分流两种手术方式的围术期差异,评价其术后及近期疗效,为手术处理策略提供新选择。方法 回顾性分析2017年2月—2020年3月我中心行手术治疗的68例急性A2型主动脉夹层患者。其中外膜内翻组22例应用扩大外膜内翻并翻转吻合技术;包裹组46例应用主动脉包裹后右房分流技术。比较两组患者术前、术中及术后近期随访结果,评价其疗效及安全性。结果 外膜内翻组手术总时长、停机至关皮时间较包裹组明显缩短(P < 0.05)。对比术后2周内及术后12个月心脏超声可见包裹组窦管交界直径明显扩张(P < 0.05)。随访节点内外膜内翻组技术可有效闭合夹层假腔,降低吻合口漏风险,同时其复位主动脉瓣膜的效果维持情况优于包裹组技术(P < 0.05),两组之间再手术相关事件发生情况存在明显差异(P < 0.05)。结论 外膜内翻并翻转吻合技术处理A2型主动脉夹层较主动脉包裹后右房分流技术明显缩短了手术时间并可预防窦管交界的近期扩张,应用其处理主动脉根部安全且可靠,近期手术疗效维持更佳。Abstract: Objective We compared the perioperative differences between extended adventitial inversion with graft eversion anastomosis technique and aortic wall wrapping graft with right atrial shunt anastomosis technique to evaluate postoperative and short-term efficacy and provide a new surgical method.Methods The 68 patients with acute A2 aortic dissection were analyzed retrospectively, who underwent surgery in our center from February 2017 to March 2020. Of them, 22 cases were treated with extended adventitial inversion with graft eversion anastomosis(eAiGe); 46 cases were treated with aortic wall wrapping graft with right atrial shunt anastomosis(AwAs). Some concerned results from pre-operation, intra-operation and short-term follow-ups of two groups were compared to evaluate the efficacy and safety.Results The total time of surgery and extracorporeal circulation halt to suture skin were significantly shorter in eAiGe group(P < 0.05). For postoperative 2 weeks and 12 months the diameter of the sinotubular junction(STJ) was significantly dilated in AwAs group(P < 0.05). The eAiGe was effective in closing the false lumen, reducing the risk of anastomotic leakage, and maintaining the effect of the resetting aortic valvar follow-up time(P < 0.05). The difference between two groups of the occurrence of reoperation-related events was significant(P < 0.05).Conclusion The eAiGe significantly reduces operative time and prevents the dilatation of STJ, which was more safer and reliable in the remodeling of the aortic root and maintained better in short-term in A2 aortic dissection.
-
Key words:
- anastomosis technique /
- aortic dissection /
- aortic root /
- efficacy
-

-
表 1 患者一般情况
Table 1. General information of patients
例(%), X±S 项目 外膜内翻组(22例) 包裹组(46例) 统计值 P 男性 16(72.7) 28(60.9) 0.92 0.338 年龄/岁 54.36±14.64 57.00±12.32 0.78 0.439 高血压 20(90.9) 38(82.6) * 0.481 糖尿病 3(13.6) 8(17.4) * 1.000 吸烟史 5(22.7) 12(26.1) 0.09 0.765 规律饮酒史 3(13.6) 8(17.4) * 1.000 手术方式 5.04 0.081 升主动脉置换 9(40.9) 21(45.7) 升主动脉置换+半弓置换/成型 1(4.5) 12(26.1) 升主动脉置换+主动脉弓置换+远端支架置入术 10(45.5) 13(28.3) 术前瓣膜反流(轻度/中度) 8(36.4)/14(63.6) 24(52.2)/22(47.8) 1.49 0.222 主动脉窦受累情况 2.49 0.287 单纯无冠窦 6(27.3) 21(45.7) 无冠窦+右冠窦 15(68.2) 22(47.8) 无冠窦+左冠窦+右冠窦 1(4.5) 3(6.5) 主动脉瓣膜交界受累情况 0.52 0.772 右、无交界撕脱 17(77.3) 37(80.4) 左、无交界撕脱 0(0) 1(2.2) 右、无+左、无交界撕脱 3(13.6) 8(17.4) 冠脉开口受累情况 * 1.000 Neri A 3(13.6) 4(8.7) Neri B 2(9.1) 5(10.9) Neri C 0(0) 0(0) 术前超声情况 ASD/mm 35.75±4.03 36.50±4.33 0.74 0.458 STJD/mm 37.18±4.24 40.13±6.69 1.61 0.107 AVAD/mm 24.09±1.97 25.33±2.76 1.89 0.059 LVD/mm 49.73±2.47 49.00±4.09 0.96 0.339 RAD/mm 31.41±10.91 28.89±7.33 0.36 0.722 LVEF/% 50.18±10.59 48.37±7.72 0.27 0.787 注:*为Fisher精确检验;Neri分型[4]:A:冠脉开口正常;B:冠脉开口血肿;C:冠脉开口局部离断。 表 2 手术时间
Table 2. Surgery time
min, X±S 手术相关时间 外膜内翻组(22例) 包裹组(46例) 统计值 P 心肌阻断时间 83.23±24.46 87.04±29.66 0.35 0.723 停循环时间 9.22±9.75 11.13±16.65 0.33 0.738 手术总时长(切皮至关皮) 354.27±74.10 392.52±83.83 1.98 0.047 开皮至停机时间 287.49±70.50 314.02±67.02 1.93 0.054 停机至关皮时间 66.78±9.49 78.50±16.76 3.09 0.002 表 3 术后及随访心脏结构
Table 3. Post-operative and follow-up cardiac structure
X±S 超声结构指标 外膜内翻组(20例) 包裹组(42例) 术后2周内 随访节点 统计值 P 术后2周内 随访节点 统计值 P ASD/mm 34.90±5.06 35.15±4.92 0.82 0.414 37.83±4.57 37.79±4.52 1.00 0.317 AVAD/mm 24.05±2.14 24.10±2.07 0.26 0.796 25.26±2.73 25.95±3.60 1.89 0.058 STJD/mm 37.30±4.19 34.90±5.34 1.95 0.052 40.67±7.08 42.35±6.48 2.47 0.014 LVD/mm 47.85±3.03 47.50±2.93 1.13 0.259 48.24±3.61 46.11±5.91 0.74 0.463 RAD/mm 29.65±10.59 29.10±9.74 1.49 0.137 31.50±10.04 34.23±9.74 1.90 0.058 LVEF/% 48.50±9.02 47.75±7.97 1.00 0.317 48.38±6.90 48.62±6.48 0.58 0.564 表 4 再手术相关事件
Table 4. Re-operation related events
例(%) 随访节点评估内容 外膜内翻组(20例) 包裹组(42例) 统计值 P 主动脉根部夹层假腔复现 0(0) 19(45.2) 13.05 0.000 主动脉根部吻合口漏 0(0) 9(21.4) * 0.047 中等量以上心包积液 1(5.0) 4(9.5) * 1.000 纵隔感染或感染性心内膜炎 1(5.0) 2(4.8) * 1.000 主动脉瓣膜反流情况 术后2周内有反流 4(20.0) 7(16.7) * 0.735 随访节点内反流进展 2(10.0) 15(35.7) 4.50 0.034 注:*为Fisher精确检验 -
[1] Ullery BW, Suh GY, Hirotsu K, et al. Geometric deformations of the thoracic aorta and supra-aortic arch branch vessels following thoracic endovascular aortic repair[J]. Vasc Endovascular Surg, 2018, 52(3): 173-180. doi: 10.1177/1538574417753452
[2] Caffarelli AD, Fann JI, Salerno CT, et al. Cardiac allograft aortic dissection: successful repair using a composite valve graft and modified-Cabrol coronary reconstruction[J]. J Card Surg, 2005, 20(5): 450-452. doi: 10.1111/j.1540-8191.2005.200467.x
[3] Nicholas TK, Eugene HB, Donald BD, et al. Kirklin/Barrat-Boyes Cardiac Surgery[M]. 3rd ed. Philvdelphia: Churchill Livingstone, 2003: 1820-1834.
[4] Xue Y, Zhou Q, Pan J, et al. Root reconstruction for proximal repair in acute type A aortic dissection[J]. J Thorac Dis, 2019, 11(11): 4708-4716. doi: 10.21037/jtd.2019.10.62
[5] Howard DP, Banerjee A, Fairhead JF, et al. Population-based study of incidence and outcome of acute aortic dissection and premorbid risk factor control: 10-year results from the Oxford Vascular Study[J]. Circulation, 2013, 127(20): 2031-2037. doi: 10.1161/CIRCULATIONAHA.112.000483
[6] 冯鑫, 夏良涛, 魏翔, 等. ABO血型与主动脉夹层的相关性: 单中心1448例回顾性队列研究[J]. 临床心血管病杂志, 2021, 37(2): 146-150. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXB202102012.htm
[7] Korotcova L, Kumar S, Agematsu K, et al. Prolonged white matter inflammation after cardiopulmonary bypass and circulatory arrest in a juvenile porcine model[J]. Ann Thorac Surg, 2015, 100(3): 1030-1037. doi: 10.1016/j.athoracsur.2015.04.017
[8] 金祺, 李呈龙, 樊凡, 等. 急性A型主动脉夹层患者围术期血小板动态变化与预后相关性分析[J]. 心肺血管病杂志, 2020, 39(2): 173-177. https://www.cnki.com.cn/Article/CJFDTOTAL-XFXZ202002019.htm
[9] 孙立忠, 刘宁宁, 常谦, 等. 主动脉夹层的细化分型及其应用[J]. 中华外科杂志, 2005, 43(18): 1171-1176. doi: 10.3760/j:issn:0529-5815.2005.18.002
[10] Tasca G, Jaworek M, Lucherini F, et al. Leaflet kinematics after the Yacoub and Florida-sleeve operations: results of an in vitro study[J]. Eur J Cardiothorac Surg, 2021, 59(3): 674-679. doi: 10.1093/ejcts/ezaa370
[11] Floten HS, Ravichandran PS, Furnary AP, et al. Adventitial inversion technique in repair of aortic dissection[J]. Ann Thorac Surg, 1995, 59(3): 771-772. doi: 10.1016/0003-4975(94)01018-8
[12] Qiu J, Wu J, Xie E, et al. Surgical management and outcomes of the aortic root in acute type A aortic dissection[J]. Ann Thorac Surg, 2020, 110(1): 136-143. doi: 10.1016/j.athoracsur.2019.10.014
[13] Tamura N, Komiya T, Sakaguchi G, et al. 'Turn-up' anastomotic technique for acute aortic dissection[J]. Eur J Cardiothorac Surg, 2007, 31(3): 548-549. doi: 10.1016/j.ejcts.2006.11.059
[14] Kazui T, Washiyama N, Muhammad BA, et al. Total arch replacement using aortic arch branched grafts with the aid of antegrade selective cerebral perfusion[J]. Ann Thorac Surg, 2000, 70(1): 3-8;discussion 8-9. doi: 10.1016/S0003-4975(00)01535-6
[15] 周子凡, 王龙飞, 王珺, 等. DavidⅠ与Bentall术治疗主动脉根部病变[J]. 中华胸心血管外科杂志, 2019, 10(7): 414-416. doi: 10.3760/cma.j.issn.1001-4497.2019.07.007
[16] 陈彧, 马维国, 李建荣, 等. Bentall术后Stanford A型主动脉夹层手术治疗[J]. 中华胸心血管外科杂志, 2018, 9(6): 344-349. doi: 10.3760/cma.j.issn.1001-4497.2018.06.005
[17] Moreira R, Jacinto T, Neves P, et al. Predictors of acute kidney injury in the postoperative period of cardiac surgery associated with cardiopulmonary bypass[J]. Rev Port Cir Cardiotorac Vasc, 2017, 24(3-4): 154.
[18] Kirsch M, Soustelle C, Houël R, et al. Risk factor analysis for proximal and distal reoperations after surgery for acute type A aortic dissection[J]. J Thorac Cardiovasc Surg, 2002, 123(2): 318-325. doi: 10.1067/mtc.2002.119702
-




 下载:
下载: