The predictive value of platelet aggregation level in predicting short-term adverse cardiovascular events in patients with acute coronary syndrome
-
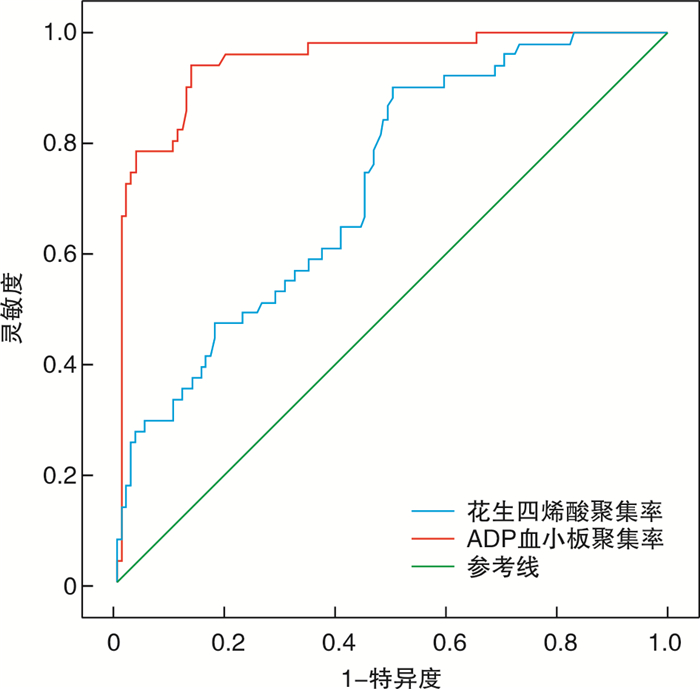
摘要: 目的 探讨血小板聚集率对急性冠状动脉综合征(ACS)患者短期发生心血管不良事件的预测价值。方法 选取自2018年12月—2021年4月就诊于河北省人民医院的ACS患者169例。根据是否发生主要不良心血管事件(MACE)分为未发生事件组(A组,118例)和发生事件组(B组,51例),比较两组基本资料及血小板聚集水平。结果 花生四烯酸聚集率A组为(15.37±13.06)%,B组为(31.26±23.90)%,两组差异有统计学意义(P < 0.001)。ADP血小板聚集率A组为(29.32±12.05)%,B组为(55.74±11.42)%,两组差异有统计学意义(P < 0.001)。ROC曲线显示,花生四烯酸聚集率预测ACS短期发生MACE事件的截点、曲线下面积、灵敏度、特异度分别为12.45%、0.724、90.2%、50.0%,ADP血小板聚集率预测ACS短期发生MACE事件的截点、曲线下面积、灵敏度、特异度分别为41.25%、0.949、94.1%、86.4%。结论 血小板聚集水平对ACS患者短期内发生心血管不良事件有一定的预测价值。Abstract: Objective To investigate the predictive value of platelet aggregation on short-term adverse cardiovascular events in patients with acute coronary syndrome.Methods A total of 169 patients with acute coronary syndrome were selected as the study subjects in Hebei General Hospital from December 2018 to April 2021. According to the occurrence of MACE events, the patients were divided into group A(n=118) and group B(n=51), and the clinical data and platelet aggregation levels of the two groups were compared.Results The average arachidonic acid aggregation rate and ADP platelet aggregation rate in group A were (15.37±13.06)% and (29.32±12.05)%, respectively. The mean arachidonic acid aggregation rate was (31.26±23.90)%, and the mean ADP platelet aggregation rate was (55.74±11.42)% in group B, with statistical difference between the two groups(P < 0.001). ROC curve analysis showed that the cut-off point, area under curve, sensitivity and specificity of arachidonic acid aggregation rate for predicting short-term MACE events in patients with acute coronary syndrome were 12.45%, 0.724, 90.2%, and 50.0% respectively. The cut-off point, area under curve, sensitivity and specificity of ADP platelet aggregation rate for predicting short-term MACE events in patients with acute coronary syndrome were 41.25%, 0.949, 94.1%, and 86.4% respectively.Conclusion Platelet aggregation level has certain predictive value for short-term adverse cardiovascular events in patients with acute coronary syndrome.
-

-
表 1 两组患者临床基线特征比较
Table 1. Baseline clinical characteristics
例(%), X±S 指标 A组(118例) B组(51例) P值 男性 97(82.2) 32(62.7) 0.006 年龄/岁 60.30±9.50 65.33±9.32 0.008 BMI/(kg·m-2) 25.61±3.47 26.00±2.94 0.497 心肌梗死 18(15.3) 10(19.6) 0.485 冠脉介入 21(17.8) 16(31.4) 0.050 冠脉移植 2(1.7) 1(2.0) 0.905 溶栓 4(3.4) 1(2.0) 0.993 冠心病 54(45.8) 28(54.9) 0.275 外周血管疾病 13(11) 15(29.4) 0.003 脑梗死或TIA 11(9.3) 7(13.7) 0.394 心律失常 12(10.2) 6(11.8) 0.758 慢性肾病 0(0) 4(2.7) 0.011 高血压 76(64.4) 36(70.6) 0.435 1级 13(11.0) 3(5.9) 2级 22(18.6) 6(11.8) 3级 41(34.7) 27(52.9) 糖尿病 33(28.0) 13(25.5) 0.740 吸烟 47(39.8) 14(27.5) 0.124 高脂血症 12(10.2) 11(21.6) 0.047 家族史 35(29.7) 12(23.5) 0.414 心脏超声 LVEF/% 59.05±8.29 58.31±10.90 0.974 LVEDD/mm 47.75±4.28 48.88±5.54 0.363 LVESD/mm 32.64±5.04 33.33±6.82 0.926 诊断 0.098 STEMI 43(36.4) 10(20.0) NSTEMI 10(8.5) 5(10.0) UA 65(55.1) 35(70.0) 注:TIA:短暂性脑缺血发作;LVEF:左室射血分数;LVEDD:左室舒张末内径;LVESD:左室收缩末内径;STEMI:ST段抬高型心肌梗死;NSTEMI:非ST段抬高型心肌梗死;UA:不稳定型心绞痛。 -
[1] 张楠, 陆莹. 中性粒细胞/淋巴细胞比值与急性冠脉综合征相关性的研究进展[J]. 中国急救医学, 2021, 41(3): 265-269. doi: 10.3969/j.issn.1002-1949.2021.03.016
[2] 王鸽, 赵冠棋, 严研, 等. 幽门螺杆菌感染影响急性冠脉综合征抗栓治疗出血并发症的研究进展[J]. 中华医学杂志, 2021, 101(9): 675-678. doi: 10.3760/cma.j.cn112137-20200608-01800
[3] 陈奇, 刘洋, 衡紫微, 等. 氯吡格雷及替格瑞洛对老年急性冠脉综合征患者的疗效与安全性探讨[J]. 中国循证心血管医学杂志, 2021, 13(3): 337-341. doi: 10.3969/j.issn.1674-4055.2021.03.19
[4] 刘江萍, 木胡牙提. 急性冠脉综合征流行病学及危险因素的研究进展[J]. 国际心血管病杂志, 2019, 46(1): 1-3, 7. doi: 10.3969/j.issn.1673-6583.2019.01.001
[5] 邓新立, 刘渊, 蔡力力, 等. 老年表观健康人群血小板聚集功能检验结果调查与分析[J]. 中华检验医学杂志, 2021, 44(1): 45-49. doi: 10.3760/cma.j.cn114452-20201005-00758
[6] Siller-Matula JM, Francesconi M, Dechant C, et al. Personalized antiplatelet treatment after percutaneous coronary intervention: the MADONNA study[J]. Int J Cardiol, 2013, 167(5): 2018-23. doi: 10.1016/j.ijcard.2012.05.040
[7] 杨家明, 赵肸, 张金盈, 等. 不同抗血小板治疗方案对急性冠状动脉综合征合并基线血小板中度减少患者预后的影响[J]. 临床心血管病杂志, 2021, 37(1): 21-27. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXB202101005.htm
[8] 聂珂, 赵嫦娇. 双联强化抗血小板对急性冠脉综合征合并糖尿病患者的血小板活性及预后影响[J]. 标记免疫分析与临床, 2019, 26(3): 380-384, 388. https://www.cnki.com.cn/Article/CJFDTOTAL-BJMY201903007.htm
[9] Kim BK, Hong SJ, Cho YH, et al. Effect of ticagrelor monotherapy vs ticagrelor with aspirin on major bleeding and cardiovascular events in patients with acute coronary syndrome: The TICO Randomized Clinical Trial[J]. JAMA, 2020, 323(23): 2407-2416. doi: 10.1001/jama.2020.7580
[10] Madsen EH, Saw J, Kristensen SR, et al. Long-term aspirin and clopidogrel response evaluated by light transmission aggregometry, VerifyNow, and thrombelastography in patients undergoing percutaneous coronary intervention[J]. Clin Chem, 2010, 56(5): 839-847. doi: 10.1373/clinchem.2009.137471
[11] 中国老年保健医学研究会检验医学分会. 光学比浊法检测血小板聚集标准化专家共识[J]. 中华检验医学杂志, 2021, 44(6): 472-479. doi: 10.3760/cma.j.cn114452-20210208-00098
[12] 李世军, 司全金. 2017年欧洲心脏病学会外周动脉疾病诊断与治疗指南解读[J]. 中华老年心脑血管病杂志, 2018, 20(6): 669-672. doi: 10.3969/j.issn.1009-0126.2018.06.030
[13] 张宇琼, 史旭波. 急性冠脉综合征的血脂管理现状[J]. 现代中西医结合杂志, 2018, 27(33): 3758-3762. https://www.cnki.com.cn/Article/CJFDTOTAL-XDJH201833036.htm
[14] Oh M, Kim H, Shin EW, et al. Comparison of high-dose rosuvastatin versus low-dose rosuvastatin plus ezetimibe on carotid atherosclerotic plaque inflammation in patients with acute coronary syndrome[J]. J Cardiovasc Transl Res, 2020, 13(6): 900-907. doi: 10.1007/s12265-020-10009-4
[15] 李军胜, 刘岐涛. 早期强化他汀类药物治疗急性冠脉综合征的降脂原理及心肌保护作用[J]. 海峡药学, 2016, 28(4): 179-180. doi: 10.3969/j.issn.1006-3765.2016.04.089
[16] 王金艳, 张庆华, 亢瑞娜, 等. 急性冠脉综合征患者接受PC I治疗后中断他汀对预后的影响[J]. 重庆医学, 2014, (22): 2938-2940. doi: 10.3969/j.issn.1671-8348.2014.22.041
[17] 程光辉, 谢芳, 黄尾平, 等. 强化辛伐他汀对急性冠脉综合征合并慢性肾功能不全患者肾功能的影响[J]. 内科急危重症杂志, 2020, 26(1): 25-28. https://www.cnki.com.cn/Article/CJFDTOTAL-NKJW202001008.htm
[18] Vyshlov EV, Tsoy EI, Sultanov VS, et al. Hypolipidemic and hepatoprotective effects of a polyprenol-containing drug in patients with acute coronary syndrome[J]. Bull Exp Biol Med, 2018, 165(3): 319-321. doi: 10.1007/s10517-018-4159-x
[19] Boklage SH, Malangone-Monaco E, Lopez-Gonzalez L, et al. Statin utilization patterns and outcomes for patients with acute coronary syndrome during and following inpatient admissions[J]. Cardiovasc Drugs Ther, 2018, 32(3): 273-280. doi: 10.1007/s10557-018-6800-3
[20] 李靖, 王乐丰, Li J, 等. 急性冠脉综合征抗栓治疗出血情况研究现状[J]. 国际心血管病杂志, 2009, 36(5): 270-273. doi: 10.3969/j.issn.1673-6583.2009.05.005
[21] Sharma R, Kumar P, Prashanth SP, et al. Dual antiplatelet therapy in coronary artery disease[J]. Cardiol Ther, 2020, 9(2): 349-361. doi: 10.1007/s40119-020-00197-0
[22] 王添艳, 孙增先. 新型ADP-P2Y12受体拮抗剂研究进展[J]. 浙江医学, 2020, 42(2): 192-197. https://www.cnki.com.cn/Article/CJFDTOTAL-ZJYE202002028.htm
[23] 尹毓瑶, 张新鑫, 潘一龙, 等. 比较替格瑞洛和氯吡格雷治疗急性冠脉综合征合并糖尿病不同随访时间疗效和安全性的Meta分析[J]. 安徽医药, 2021, 25(10): 1909-1915. doi: 10.3969/j.issn.1009-6469.2021.10.001
[24] Bonello L, Laine M, Kipson N, et al. Ticagrelor increases adenosine plasma concentration in patients with an acute coronary syndrome[J]. J Am Coll Cardiol, 2014, 63(9): 872-877. doi: 10.1016/j.jacc.2013.09.067
[25] 中国医师协会心血管内科医师分会血栓防治专业委员会, 中华医学会心血管病学分会介入学组, 中华心血管病杂志编辑委员会. 替格瑞洛临床应用中国专家共识[J]. 中华心血管病杂志, 2016, 44(2): 112-120. https://www.cnki.com.cn/Article/CJFDTOTAL-JYGZ201605002.htm
[26] Ellithi M, Baye J, Wilke RA. CYP2C19 genotype-guided antiplatelet therapy: promises and pitfalls[J]. Pharmacogenomics, 2020, 21(12): 889-897.
-




 下载:
下载: