Correlation analysis of Lp(a), ApoB, sd LDL-C and cardiovascular outcomes in patients with coronary heart disease
-
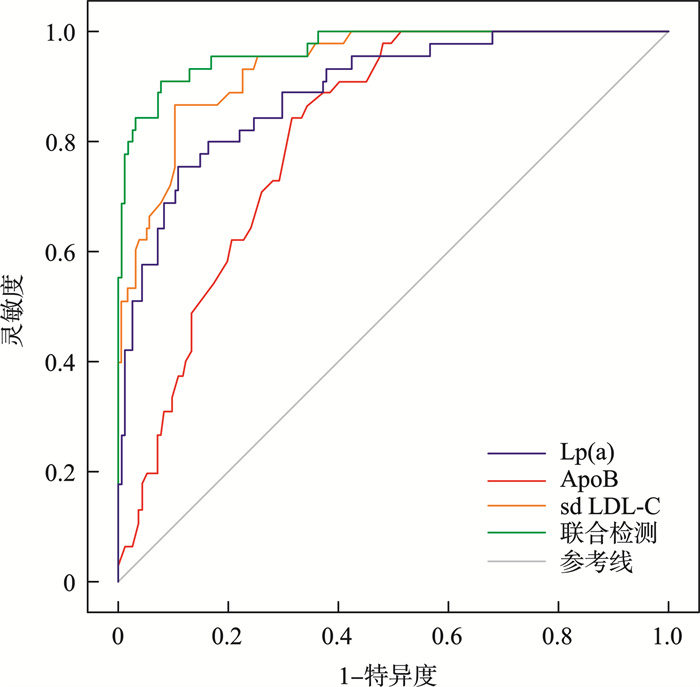
摘要: 目的 探讨血清脂蛋白a[Lp(a)]、载脂蛋白B(ApoB)、小而密低密度脂蛋白胆固醇(sd LDL-C)与冠心病患者心血管事件结局的相关性。方法 纳入2021年1月—2024年1月本院诊治的198例冠心病患者,根据是否发生主要不良心血管事件(MACE)分为MACE组(45例)、非MACE组(153例)。对比两组临床资料、血清Lp(a)、ApoB及sd LDL-C水平,logistic回归分析影响MACE发生的危险因素。ROC曲线分析血清Lp(a)、ApoB、sd LDL-C及联合检测预测冠心病患者发生MACE的效能。结果 Logistic回归分析显示吸烟、饮酒、高水平Lp(a)、ApoB及sd LDL-C均为影响冠心病患者发生MACE的独立危险因素(OR=1.072、1.425、1.549、1.398、1.266,均P<0.05)。ROC曲线显示,Lp(a)(AUC=0.892,95%CI 0.840~0.931)、ApoB(AUC=0.811,95%CI 0.750~0.863)、sd LDL-C(AUC=0.937,95%CI 0.893~0.966)及联合检测(AUC=0.969,95%CI 0.934~0.988)预测冠心病患者发生MACE具有一定价值。结论 血清Lp(a)、ApoB、sd LDL-C水平均为影响冠心病患者发生MACE的独立危险因素,且上述指标能预测冠心病患者MACE的发生,联合预测价值更高。
-
关键词:
- 冠心病 /
- 主要不良心血管事件 /
- 脂蛋白a /
- 载脂蛋白B /
- 小而密低密度脂蛋白胆固醇
Abstract: Objective To investigate the correlation between serum lipoprotein a[Lp(a)], apolipoprotein B(ApoB), small and dense low-density lipoprotein cholesterol(sd LDL-C) and major adverse cardiovascular events(MACE) in patients with coronary heart disease.Methods A total of 198 patients with coronary heart disease were enrolled from January 2021 to January 2024 and divided into MACE group(45 cases) and non-MACE group(153 cases). The clinical data, serum Lp(a), ApoB and sd LDL-C levels of the two groups were compared, and the risk factors affecting the occurrence of MACE were analyzed by logistic regression. ROC curve was used to analyze the efficacy of serum Lp(a), ApoB, sd LDL-C and combined detection in predicting MACE in patients with coronary heart disease.Results Logistic regression analysis showed that smoking, drinking, high level of Lp(a), ApoB and sd LDL-C were independent risk factors for MACE in coronary heart disease patients(OR=1.072, 1.425, 1.549, 1.398, 1.266, all P<0.05). ROC curve showed that Lp(a)(AUC=0.892, 95%CI=0.840-0.931), ApoB(AUC=0.811, 95%CI=0.750-0.863), sd LDL-C(AUC=0.937, 95%CI=0.893-0.966) and combined test(AUC=0.969, 95%CI=0.934-0.988) have certain value in predicting the occurrence of MACE in patients with coronary heart disease.Conclusion Serum Lp(a), ApoB and sd LDL-C levels are all independent risk factors for the occurrence of MACE in patients with coronary heart disease, and the above indexes can predict the occurrence of MACE in patients with coronary heart disease, and the combined prediction value is higher. -

-
表 1 两组临床资料比较
Table 1. General data
例(%), X±S 临床资料 MACE组(45例) 非MACE组(153例) χ2/t P 性别 0.035 0.853 男性 24(53.33) 84(54.90) 女性 21(46.67) 69(45.10) 年龄/岁 56.88±10.69 57.24±9.88 -0.211 0.833 受教育水平 0.129 0.719 初中及以下 10(22.22) 38(24.84) 高中及以上 35(77.78) 115(75.16) 体重指数/(kg/m2) 22.16±2.58 22.49±2.04 -0.896 0.372 病程/年 3.26±1.49 3.45±1.28 -0.842 0.401 高血压 0.186 0.666 是 24(53.33) 76(49.67) 否 21(46.67) 77(50.33) 高血脂症 0.088 0.767 是 18(40.00) 65(42.48) 否 27(60.00) 88(57.52) 糖尿病 0.042 0.838 是 19(42.22) 62(40.52) 否 26(57.78) 91(59.48) 吸烟 8.508 0.004 是 18(40.00) 29(18.95) 否 27(60.00) 124(81.05) 饮酒 5.890 0.015 是 23(51.11) 48(31.37) 否 22(48.89) 105(68.63) 冠心病家族史 0.066 0.797 是 9(20.00) 28(18.30) 否 36(80.00) 125(81.70) Lp(a)/(mg/L) 189.63±32.59 139.56±25.69 10.779 <0.001 ApoB/(g/L) 1.18±0.16 0.91±0.25 6.838 <0.001 sd LDL-C/(mmol/L) 1.48±0.33 0.84±0.26 13.612 <0.001 表 2 变量赋值表
Table 2. Variable assignment
变量 因素 赋值 因变量 MACE 未发生=0,发生=1 自变量 吸烟 否=0,是=1 自变量 饮酒 否=0,是=1 自变量 Lp(a) 实际值 自变量 ApoB 实际值 自变量 sd LDL-C 实际值 表 3 MACE发生因素的logistic回归分析
Table 3. Logistic regression analysis of MACE occurrence factors
因素 β SE Wald χ2 P OR 95%CI 吸烟 0.070 0.023 9.138 0.003 1.072 1.025~1.121 饮酒 0.354 0.121 8.568 0.003 1.425 1.124~1.806 Lp(a) 0.438 0.159 7.575 0.006 1.549 1.134~2.115 ApoB 0.335 0.127 6.960 0.008 1.398 1.090~1.793 sd LDL-C 0.236 0.087 7.349 0.007 1.266 1.068~1.501 表 4 血清Lp(a)、ApoB、sd LDL-C及联合检测预测冠心病患者发生MACE的效能
Table 4. Efficacy of serum Lp(a), ApoB, sd LDL-C in predicting MACE in patients with CHD
指标 灵敏度/% 特异度/% AUC 95%CI 截断值 Youden指数 Lp(a) 75.56 88.89 0.892 0.840~0.931 167.64 mg/L 0.644 ApoB 84.44 67.97 0.811 0.750~0.863 1.04 g/L 0.524 sd LDL-C 86.67 89.54 0.937 0.893~0.966 1.19 mmol/L 0.762 联合检测 91.11 92.16 0.969 0.934~0.988 - 0.833 -
[1] Silventoinen K, Lahtinen H, Davey Smith G, et al. Height, social position and coronary heart disease incidence: the contribution of genetic and environmental factors[J]. J Epidemiol Community Health, 2023, 77(6): 384-390. doi: 10.1136/jech-2022-219907
[2] Jiesisibieke ZL, Panter J, Wang MY, et al. Mode of transport, genetic susceptibility, and incidence of coronary heart disease[J]. Int J Behav Nutr Phys Act, 2023, 20(1): 79. doi: 10.1186/s12966-023-01484-4
[3] Kelshiker MA, Seligman H, Howard JP, et al. Coronary flow reserve and cardiovascular outcomes: a systematic review and meta-analysis[J]. Eur Heart J, 2022, 43(16): 1582-1593. doi: 10.1093/eurheartj/ehab775
[4] Wang KL, Meah MN, Bularga A, et al. Computed tomography coronary angiography in non-ST-segment elevation myocardial infarction[J]. Br J Radiol, 2022, 95(1140): 20220346. doi: 10.1259/bjr.20220346
[5] 王安吉, 徐春雪, 薛永利. 冠状动脉CT血管造影对急性冠状动脉综合征的评价及影响因素分析[J]. 临床心血管病杂志, 2024, 40(8): 628-631. doi: 10.13201/j.issn.1001-1439.2024.08.005
[6] Snaebjarnarson AS, Helgadottir A, Arnadottir GA, et al. Complex effects of sequence variants on lipid levels and coronary artery disease[J]. Cell, 2023, 186(19): 4085-4099. e15. doi: 10.1016/j.cell.2023.08.012
[7] 王怡雯, 韩拓, 王丽霞, 等. 脂蛋白(a)与冠心病相关性的研究进展[J]. 临床心血管病杂志, 2022, 38(11): 860-863.
[8] Jung HW, Ra M, Bae HJ, et al. The LDL-C/Apo B predicts coronary atherosclerotic heart disease in non-diabetic patients without high LDL-C[J]. Medicine, 2023, 102(1): e32596. doi: 10.1097/MD.0000000000032596
[9] Fu C, Liu DB, Liu Q, et al. Revisiting an old relationship: the causal associations of the ApoB/ApoA1 ratio with cardiometabolic diseases and relative risk factors-a Mendelian randomization analysis[J]. Cardiovasc Diabetol, 2024, 23(1): 51. doi: 10.1186/s12933-024-02140-2
[10] Tsimikas S, Witztum JL. Oxidized phospholipids in cardiovascular disease[J]. Nat Rev Cardiol, 2024, 21: 170-191. doi: 10.1038/s41569-023-00937-4
[11] Gilliland TC, Liu YX, Mohebi R, et al. Lipoprotein(a), oxidized phospholipids, and coronary artery disease severity and outcomes[J]. J Am Coll Cardiol, 2023, 81(18): 1780-1792. doi: 10.1016/j.jacc.2023.02.050
[12] Rikhi R, Schaich CL, Hafzalla GW, et al. Small dense low-density lipoprotein cholesterol and coronary artery calcification in the Multi-Ethnic Study of Atherosclerosis[J]. Eur J Prev Cardiol, 2024, 31(8): 1048-1054. doi: 10.1093/eurjpc/zwae049
[13] 木那瓦尔·克热木, 迪拉热·阿迪, 魏娴, 等. 小而密低密度脂蛋白与心血管疾病相关性的研究进展[J]. 中国心血管杂志, 2023, 28(6): 583-587.
[14] 李立青, 陈春彦, 米运强, 等. sd-LDL、CHO、血脂水平与老年冠心病患者病情程度的关系[J]. 现代医药卫生, 2023, 39(20): 3490-3494. doi: 10.3969/j.issn.1009-5519.2023.20.016
[15] 中华医学会, 中华医学会杂志社, 中华医学会全科医学分会, 等. 冠心病心脏康复基层指南(2020年)[J]. 中华全科医师杂志, 2021, 20(2): 150-165.
[16] 张雯雯, 胡月, 黄秋霞. 多视角PAC心理弹性理论在冠心病经皮冠状动脉介入术治疗患者中的应用效果[J]. 中国健康心理学杂志, 2024, 32(6): 909-913.
[17] Starodubtseva I, Meshkova M, Zuikova A. Pathogenetic mechanisms of repeated adverse cardiovascular events development in patients with coronary heart disease: the role of chronic inflammation[J]. Folia Med, 2023, 65(6): 863-870. doi: 10.3897/folmed.65.e109433
[18] Zheng JN, Lu B. Current progress of studies of coronary CT for risk prediction of major adverse cardiovascular event(MACE)[J]. J Cardiovasc Imaging, 2021, 29(4): 301-315. doi: 10.4250/jcvi.2021.0016
[19] 彭菊琴, 廖江铨, 王瑞茵, 等. 血脂变异性与冠心病患者不良心血管事件的相关性[J]. 中国心血管杂志, 2022, 27(3): 252-257.
[20] 何蕊. 血小板聚集率、基质金属蛋白酶-9与老年冠心病患者心血管不良事件的相关性[J]. 医学理论与实践, 2024, 37(11): 1912-1914.
[21] Mao CY, Li DJ, Zhou E, et al. Nicotine exacerbates atherosclerosis through a macrophage-mediated endothelial injury pathway[J]. Aging, 2021, 13(5): 7627-7643. doi: 10.18632/aging.202660
[22] Boyaci F, Akcay M, Hatem E, et al. Assessment of arterial stiffness with cardio-ankle vascular index in patients with mitral annular calcification[J]. Eurasian J Med, 2021, 53(2): 90-95. doi: 10.5152/eurasianjmed.2021.19235
[23] Petermann-Rocha F, Deo S, Celis-Morales C, et al. An opportunity for prevention: associations between the life's essential 8 score and cardiovascular incidence using prospective data from UK biobank[J]. Curr Probl Cardiol, 2023, 48(4): 101540.
[24] Arora M, ElSayed A, Beger B, et al. The impact of alcohol consumption on cardiovascular health: myths and measures[J]. Glob Heart, 2022, 17(1): 45.
[25] Wong CX, Tu SJ, Marcus GM. Alcohol and arrhythmias[J]. JACC Clin Electrophysiol, 2023, 9(2): 266-279.
[26] Cruijsen E, de Ruiter AJ, Küpers LK, et al. Alcohol intake and long-term mortality risk after myocardial infarction in the Alpha Omega Cohort[J]. Am J Clin Nutr, 2022, 115(3): 633-642.
[27] Jang AY, Scherer PE, Kim JY, et al. Adiponectin and cardiometabolic trait and mortality: where do we go?[J]. Cardiovasc Res, 2022, 118(9): 2074-2084.
[28] Sarraju A, Nissen SE. Atherosclerotic plaque stabilization and regression: a review of clinical evidence[J]. Nat Rev Cardiol, 2024, 21(7): 487-497.
[29] Zhang J, Jia L, Yang Y, et al. Lipoprotein(a)and myocardial infarction: impact on long-term mortality[J]. Lipids Health Dis, 2023, 22(1): 70.
[30] Simons LA, Simons J. Lipoprotein(a)and the risk of recurrent coronary heart disease: the dubbo study[J]. Curr Med Res Opin, 2023, 39(7): 933-938.
[31] Hagström E, Steg PG, Szarek M, et al. Apolipoprotein B, residual cardiovascular risk after acute coronary syndrome, and effects of alirocumab[J]. Circulation, 2022, 146(9): 657-672.
[32] Yamaji T, Harada T, Kajikawa M, et al. Role of small dense low-density lipoprotein cholesterol in cardiovascular events in patients with coronary artery disease and type 2 diabetes mellitus receiving statin treatment[J]. J Atheroscler Thromb, 2024, 31(4): 478-500.
[33] Sourij C, Aziz F, Krappinger S, et al. Changes in lipoprotein(a)levels in people after ST elevation myocardial infarction-the STEMI-lipids study[J]. Int J Mol Sci, 2023, 24(21): 15531.
[34] 邓俊杰, 呼靖宣, 李兴华, 等. 小而密低密度脂蛋白胆固醇预测老年冠心病患者主要不良心血管事件的价值[J]. 实用临床医药杂志, 2022, 26(3): 34-38.
-

计量
- 文章访问数: 687
- 施引文献: 0



 下载:
下载: