The diagnostic value of D-dimer combined with neutrophil to high-density lipoprotein cholesterol ratio in aortic dissection
-
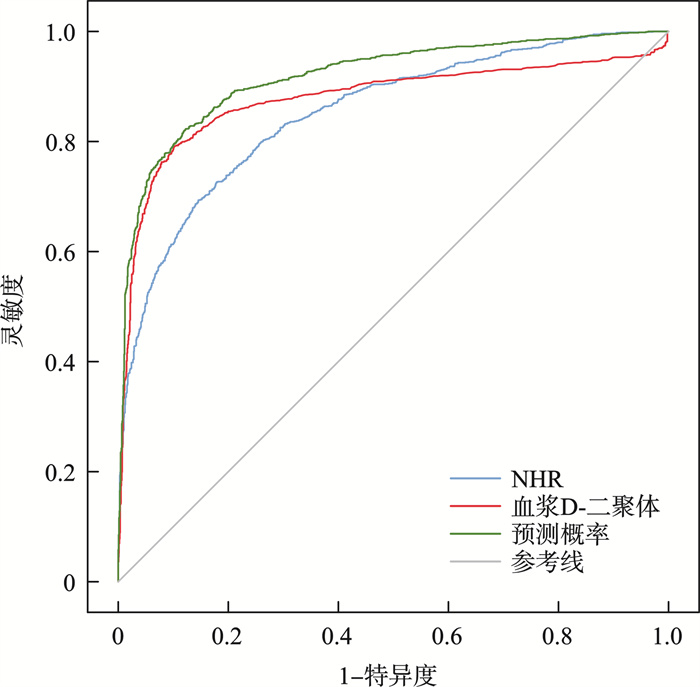
摘要: 目的 探讨D-二聚体联合外周血中中性粒细胞与高密度脂蛋白胆固醇比值(NHR)对主动脉夹层(AD)患者的诊断意义。方法 通过电子病历连续收集2012年4月—2023年5月就诊于新疆医科大学第一附属医院及新疆维吾尔自治区人民医院的1 509例AD患者和同一时期1 769例健康对照者的临床资料、入院时首次血常规、生化等数据,计算NHR。结果 ① 与对照组相比,AD组的收缩压和心率、白细胞总计数等水平显著升高,而血清血小板计数、总胆固醇和高密度脂蛋白水平显著降低(P<0.05);②AD组NHR明显高于对照组[7.74(5.07,11.76) vs 3.44(2.48,4.76),P<0.001];③单因素及多因素logistic回归分析显示,NHR是AD的独立危险因素;④根据受试者工作特征曲线分析,D-二聚体联合NHR诊断AD的曲线下面积为0.918,其灵敏度、特异度分别为82.3%、87.7%。结论 NHR是AD的危险因素,具有诊断价值。NHR联合D-二聚体诊断效能更高。
-
关键词:
- 主动脉夹层 /
- 中性粒细胞与高密度脂蛋白比值 /
- 生物标志物 /
- 受试者工作特征曲线
Abstract: Objective To investigate the predictive value of neutrophils to high density lipoprotein ratio(NHR) combined with D-dimer in the early diagnosis of aortic dissection(AD).Methods One thousand five hundred and nine patients and one thousand seven hundred and sixty-nine controls who visited the First Affiliated Hospital of Xinjiang Medical University and the People's Hospital of Xinjiang Uygur Autonomous Region from April 2012 to May 2023 were included in the study. We collected clinical data and calculated NHR in patients.Results ① Compared with the control group, the systolic blood pressure, heart rate, total white blood cell count levels in the AD group were significantly increased, while serum platelet count, total cholesterol, and HDL-C levels were significantly reduced(P<0.05); ②The levels of NHR in AD group were significantly higher than those in control group[7.74(5.07, 11.76) vs 3.44(2.48, 4.76), P<0.001]; ③Multivariate logistic regression demonstrated that NHR was an independent predictor of AD; ④According to receiver operating characteristic(ROC) analysis, the area under the curve(AUC) of D-dimer combined with NHR for diagnosing AD was 0.918, the sensitivity and specificity for AD diagnosis were 82.3% and 87.7%, respectively.Conclusion NHR is a risk factor in AD and has diagnostic value. The combination of NHR and D-dimer has higher diagnostic efficacy than single. -

-
表 1 基线资料、血液学指标及NHR比较
Table 1. General data
例(%), X±S, M(P25, P75) 变量 对照组(1 769例) AD组(1 509例) t/χ2/Z P 男 1397(79.00) 1204(79.80) 0.332 0.565 年龄/岁 55.12±10.31 54.91±11.78 0.529 0.597 吸烟史 806(45.56) 719(47.65) 1.423 0.233 高血压病史 1 010(50.80) 994(82.70) 26.403 <0.001 糖尿病史 334(18.89) 131(8.68) 67.177 <0.001 收缩压/mmHg 126.00(116.00,137.00) 140.00(123.50,159.00) -19.398 <0.001 舒张压/mmHg 78.97±11.63 81.49±15.06 -5.392 <0.001 心率/(次/min) 78.00(72.00,84.00) 79.00(73.00,89.00) -5.739 <0.001 葡萄糖/(mmol/L) 5.15(4.63,6.12) 6.20(5.17,7.49) -15.436 <0.001 白细胞(×109/L) 6.53(5.47,7.90) 9.06(6.32,12.69) -19.982 <0.001 红细胞/(×1012/L) 4.76(4.37,5.12) 4.40(4.00,4.78) -15.922 <0.001 血红蛋白/(g/L) 145.00(135.00,154.00) 134.00(121.00,144.00) -19.127 <0.001 血小板/(×109/L) 227.00(189.00,267.00) 194.00(151.00,242.50) -13.613 <0.001 甘油三酯/(mmol/L) 1.71(1.17,2.77) 1.28(0.94,1.77) -15.435 <0.001 总胆固醇/(mmol/L) 4.21(3.53,4.93) 3.75(3.11,4.38) -12.231 <0.001 HDL-C/(mmol/L) 1.07(0.89,1.30) 0.87(0.69,1.07) -18.764 <0.001 LDL-C/(mmol/L) 2.75(2.20,3.36) 2.35(1.83,2.88) -12.531 <0.001 D-二聚体/(mg/L) 73.00(43.50,130.50) 815.50(188.50,2 457.75) -9.227 <0.001 BNP/(pg/mL) 44.80(29.70,7.00) 155.50(69.98,492.25) -9.399 <0.001 NHR 3.44(2.48,4.76) 7.74(5.07,11.76) -32.610 <0.001 表 2 按心血管危险因素分层的NHR水平比较
Table 2. NHR in different stratification levels of cardiovascular risk factors
M(P25, P75) 变量 分层 对照组(1 769例) AD组(1 509例) t/χ2/Z P 性别 男 3.69(2.74,5.11) 8.28(5.47,12.27) -29.734 <0.001 女 2.57(1.77,3.47) 6.01(3.76,8.61) -14.689 <0.001 年龄 ≤60岁 3.67(2.72,5.09) 8.64(5.86,12.52) -27.883 <0.001 >60岁 3.02(2.10,4.08) 5.99(4.05,8.73) -16.666 <0.001 吸烟史 是 3.86(2.86,5.26) 8.57(5.71,12.72) -22.458 <0.001 否 3.08(2.22,4.32) 7.72(4.62,10.70) -23.862 <0.001 高血压病史 是 3.54(2.56,4.96) 7.77(5.19,11.79) -25.062 <0.001 否 3.27(2.37,4.55) 7.71(4.84,11.64) -20.450 <0.001 糖尿病病史 是 3.91(2.88,5.45) 6.15(4.86,8.42) -8.499 <0.001 否 3.32(2.39,4.59) 7.59(5.07,11.93) -31.087 <0.001 BMI ≤25 kg/m2 2.86(1.98,3.91) 6.37(4.01,10.36) -16.739 <0.001 >25 kg/m2 3.71(2.76,5.15) 7.50(4.86,11.47) -19.492 <0.001 表 3 AD患者NHR水平与其他数据的相关性
Table 3. Correlation between NHR levels and other data in AD patients
变量 相关系数 P 年龄 -0.134 <0.001 收缩压 0.132 <0.001 舒张压 0.059 0.001 心率 0.071 <0.001 身高 0.050 0.020 葡萄糖 0.171 <0.001 甘油三酯 -0.030 0.105 总胆固醇 -0.147 <0.001 白细胞计数 0.439 <0.001 血小板计数 -0.163 0.002 D-二聚体 0.139 <0.001 C-反应蛋白 0.114 0.006 N端-B型钠尿肽前体 0.064 0.035 表 4 单因素和多因素logistic回归分析
Table 4. Univariant and multivariate logistic regression
变量 单因素 多因素 OR(95%CI) P OR(95%CI) P 性别 1.051(0.887~1.246) 0.565 1.775(0.587~5.372) 0.310 吸烟史 1.087(0.948~1.248) 0.233 3.188(0.769~13.221) 0.110 高血压史 1.450(1.258~1.672) <0.001 3.364(1.221~9.264) 0.019 糖尿病史 0.414(0.334~0.514) <0.001 年龄 0.998(0.992~1.005) 0.597 0.940(0.895~0.988) 0.015 BMI 1.005(0.997~1.014) 0.237 0.889(0.782~1.011) 0.073 心率 1.020(1.014~1.026) <0.001 收缩压 1.037(1.033~1.041) <0.001 葡萄糖 1.174(1.134~1.215) <0.001 甘油三酯 0.641(0.596~0.689) <0.001 0.398(0.242~0.654) <0.001 白细胞 1.296(1.262~1.331) <0.001 0.600(0.448~0.805) 0.001 血小板 0.995(0.994~0.996) <0.001 D-二聚体 1.004(1.003~1.004) <0.001 1.005(1.001~1.008) 0.007 C-反应蛋白 1.108(1.052~1.166) <0.001 1.050(0.990~1.114) 0.107 NHR 1.610(1.549~1.673) <0.001 2.286(1.500~3.484) <0.001 表 5 NHR和D-二聚体对AD患者的诊断价值
Table 5. Diagnostic value of NHR and D-dimer in AD patients
变量 灵敏度/% 特异度/% AUC 95%CI P NHR 69.3 85.8 0.851 0.837~0.866 <0.001 D-二聚体 80.7 71.8 0.877 0.862~0.892 <0.001 NHR联合D-二聚体 82.3 87.7 0.918 0.907~0.928 <0.001 -
[1] 陈司奇, 魏翔, 陈太强. Stanford A型主动脉夹层患者孙氏手术后早期截瘫原因分析[J]. 临床心血管病杂志, 2024, 40(9): 725-730. doi: 10.13201/j.issn.1001-1439.2024.09.007
[2] Mele D, Rizzo M, Campana M, et al. Imaging in acute aortic syndrome: not just dissection[J]. 2020, 21(9): 656-68.
[3] 丁吕盛, 李旎, 朱林文, 等. 新型生物标志物用于主动脉夹层诊断及预后评估价值的研究进展[J]. 浙江医学, 2023, 45(13): 1446-1453.
[4] Han L, Dai L, Zhao YF, et al. CD40 L promotes development of acute aortic dissectionvia induction of inflammation and impairment of endothelial cell function[J]. Aging, 2018, 10(3): 371-385. doi: 10.18632/aging.101394
[5] Zeng T, Shi L, Ji Q, et al. Cytokines in aortic dissection[J]. Clin Chim Acta, 2018, 486: 177-182. doi: 10.1016/j.cca.2018.08.005
[6] Erbel R, Aboyans V, Boileau C, et al. 2014 ESC guidelines on the diagnosis and treatment of aortic diseases: document covering acute and chronic aortic diseases of the thoracic and abdominal aorta of the adult. the task force for the diagnosis and treatment of aortic diseases of the European society of cardiology(ESC)[J]. Eur Heart J, 2014, 35(41): 2873-2926. doi: 10.1093/eurheartj/ehu281
[7] Evangelista A, Isselbacher EM, Bossone E, et al. Insights from the international registry of acute aortic dissection: a 20-year experience of collaborative clinical research[J]. Circulation, 2018, 137(17): 1846-1860. doi: 10.1161/CIRCULATIONAHA.117.031264
[8] Keykhaei M, Ashraf H, Rashedi S, et al. Differences in the 2020 ESC versus 2015 ESC and 2014 ACC/AHA guidelines on the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation[J]. Curr Atheroscler Rep, 2021, 23(12): 77. doi: 10.1007/s11883-021-00976-7
[9] Costa F, Ariotti S, Valgimigli M, et al. Perspectives on the 2014 ESC/EACTS guidelines on myocardial revascularization: fifty years of revascularization: where are we and where are we heading?[J]. J Cardiovasc Transl Res, 2015, 8(4): 211-220. doi: 10.1007/s12265-015-9632-6
[10] Hu W, Zhang P, Su Q, et al. Peripheral leukocyte counts vary with lipid levels, age and sex in subjects from the healthy population[J]. Atherosclerosis, 2020, 308: 15-21. doi: 10.1016/j.atherosclerosis.2020.07.009
[11] Ren LX, Wu MW, Xiong J. Preliminary progress in the study of the relationship between COVID-19 infection and partial arterial or venous diseases[J]. Zhonghua Wai Ke Za Zhi, 2023, 61(12): 1119-1123.
[12] Kou T, Luo H, Yin L. Relationship between neutrophils to HDL-C ratio and severity of coronary stenosis[J]. BMC Cardiovasc Disord, 2021, 21(1): 127. doi: 10.1186/s12872-020-01771-z
[13] Huang JB, Chen YS, Ji HY, et al. Neutrophil to high-density lipoprotein ratio has a superior prognostic value in elderly patients with acute myocardial infarction: a comparison study[J]. Lipids Health Dis, 2020, 19(1): 59. doi: 10.1186/s12944-020-01238-2
[14] Yang YY, Jiao XL, Li LY, et al. Increased circulating angiopoietin-like protein 8 levels are associated with thoracic aortic dissection and higher inflammatory conditions[J]. Cardiovasc Drugs Ther, 2020, 34(1): 65-77. doi: 10.1007/s10557-019-06924-7
[15] 中华医学会外科学分会血管外科学组. Stanford B型主动脉夹层诊断和治疗中国专家共识(2022版)[J]. 中国血管外科杂志(电子版), 2022, 14(2): 119-130.
[16] Postnov A, Suslov A, Sobenin I, et al. Thoracic aortic aneurysm: blood pressure and inflammation as key factors in the development of aneurysm dissection[J]. Curr Pharm Des, 2021, 27(28): 3122-3127. doi: 10.2174/1381612827666210210142200
[17] Paghdar S, Khan TM, Patel NP, et al. Doxycycline therapy for abdominal aortic aneurysm: inhibitory effect on matrix metalloproteinases[J]. Cureus, 2021, 13(5): e14966.
[18] Prado AF, Batista RIM, Tanus-Santos JE, et al. Matrix metalloproteinases and arterial hypertension: role of oxidative stress and nitric oxide in vascular functional and structural alterations[J]. Biomolecules, 2021, 11(4): 585. doi: 10.3390/biom11040585
[19] Morello F, Piler P, Novak M, et al. Biomarkers for diagnosis and prognostic stratification of aortic dissection: challenges and perspectives[J]. Biomark Med, 2014, 8(7): 931-941. doi: 10.2217/bmm.14.38
[20] Bossone E, Czerny M, Lerakis S, et al. Imaging and biomarkers in acute aortic syndromes: diagnostic and prognostic implications[J]. Curr Probl Cardiol, 2021, 46(3): 100654.
[21] Tomida S, Aizawa K, Nishida N, et al. Indomethacin reduces rates of aortic dissection and rupture of the abdominal aorta by inhibiting monocyte/macrophage accumulation in a murine model[J]. Sci Rep, 2019, 9(1): 10751.
[22] Cifani N, Proietta M, Taurino M, et al. Monocyte subsets, stanford-a acute aortic dissection, and carotid artery stenosis: new evidences[J]. J Immunol Res, 2019, 2019: 9782594.
[23] Liu H, Li DZ, Jia Y, et al. Predictive value of white blood cells, neutrophils, platelets, platelet to lymphocyte and neutrophil to lymphocyte ratios in patients with acute aortic dissection[J]. Braz J Cardiovasc Surg, 2020, 35(6): 1031-1033.
[24] Liu X, Su X, Zeng H. Impact of admission serum total cholesterol level on in-hospital mortality in patients with acute aortic dissection[J]. Pak J Med Sci, 2016, 32(4): 939-943.
[25] Barter PJ, Puranik R, Rye KA. New insights into the role of HDL as an anti-inflammatory agent in the prevention of cardiovascular disease[J]. Curr Cardiol Rep, 2007, 9(6): 493-498.
[26] Barrett TJ, Distel E, Murphy AJ, et al. Apolipoprotein AI)promotes atherosclerosis regression in diabetic mice by suppressing myelopoiesis and plaque inflammation[J]. Circulation, 2019, 140(14): 1170-1184.
[27] Liu XT, He XW, Tan R, et al. High-density lipoprotein cholesterol and in-hospital mortality in patients with acute aortic dissection[J]. Huazhong Keji Daxue Xuebao Yixue Yingdewen Ban, 2016, 36(3): 364-367.
[28] Zhao LF, Jin H, Yang B, et al. Correlation between ABCA1 gene polymorphism and aopA-I and HDL-C in abdominal aortic aneurysm[J]. Med Sci Monit, 2016, 22: 172-176.
[29] Delbosc S, Rouer M, Alsac JM, et al. High-density lipoprotein therapy inhibits Porphyromonas gingivalis-induced abdominal aortic aneurysm progression[J]. Thromb Haemost, 2016, 115(4): 789-799.
[30] 董继斌. 高密度脂蛋白(HDL)抗动脉粥样硬化研究进展[J]. 复旦学报(医学版), 2012, 39(4): 414-417.
[31] Ronsein GE, Vaisar T. Inflammation, remodeling, and other factors affecting HDL cholesterol efflux[J]. Curr Opin Lipidol, 2017, 28(1): 52-59.
[32] van der Westhuyzen DR, de Beer FC, Webb NR. HDL cholesterol transport during inflammation[J]. Curr Opin Lipidol, 2007, 18(2): 147-151.
[33] Du X, Zhang SL, Xu J, et al. Diagnostic value of monocyte to high-density lipoprotein ratio in acute aortic dissection in a Chinese Han population[J]. Expert Rev Mol Diagn, 2020, 20(12): 1243-1252.
[34] Jeffrey IW, James CF, John WE. A test in context: D-dimer[J]. J Am Coll Cardiol, 2017, 70(19): 110.
[35] Aydin S, Ugur K, Aydin S, et al. Biomarkers in acute myocardial infarction: current perspectives[J]. Vasc Health Risk Manag, 2019, 15: 1-10.
-

计量
- 文章访问数: 433
- 施引文献: 0



 下载:
下载: