Advances in the diagnosis and pharmacological treatment of heart failure combined with diuretic resistance
-
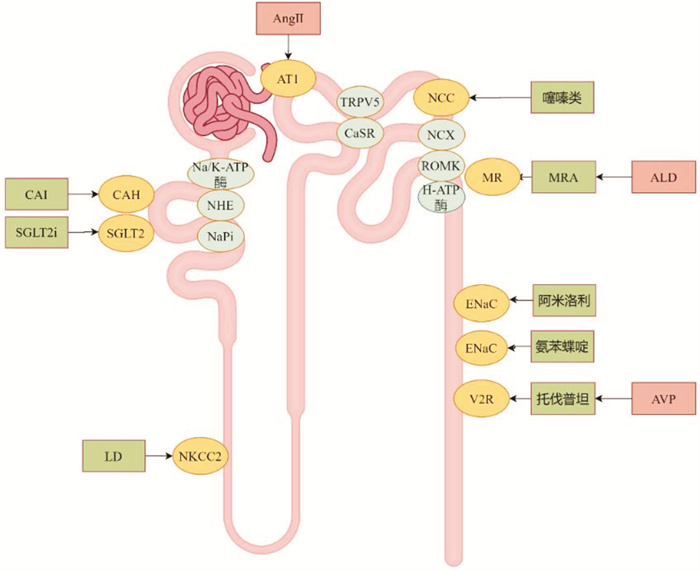
摘要: 目前认为心力衰竭合并利尿剂抵抗(DR)的主要诊断依据是尿钠(UNa)和尿量。患者每日静脉应用呋塞米剂量≥80 mg(或同等剂量的其他利尿剂),24 h尿量<800 mL,或钠排泄分数(FENa)<0.2%、UNa<50 mmol/L、UNa/UK<1.0,或应用一定剂量的利尿剂后,2 h UNa<50~70 mmol/L或6 h尿量<100~150 mL/h,则考虑存在DR。DR的药物治疗方案包括调整利尿剂剂量、改变用药途径、更改利尿剂种类、多种作用靶点的利尿剂联合使用等。Abstract: At present, the diagnosis of diuretic resistance (DR) in heart failure (HF) is mainly based on urine sodium (UNa) level and urine volume. DR is diagnosed when patients require a daily intravenous dose of furosemide≥80 mg (or equivalent dose of other diuretics), have a 24 h urine volume < 800 mL, or exhibit a sodium excretion fraction (FENa) < 0.2%, UNa < 50 mmol/L, and UNa/UK < 1.0. Additional indicators of DR include a 2 h UNa < 50-70 mEq/L or 6 h urine volume < 100-150 mL/h when administered a certain dose of diuretics. The pharmacological treatment of DR includes adjusting diuretic dosage, changing the medication route, switching to a different type of diuretic, or combining multiple diuretics targeting various mechanisms.
-
Key words:
- heart failure /
- diuretic resistance /
- diagnosis /
- pharmacological treatment
-

-
表 1 UNa作为临床结果预测因子的部分研究
Table 1. Partial studies on UNa as a predictor of clinical outcomes
研究 测量点 例数 标准 预测价值/结果 Singh,et al(2014) 随机 52 UNa < 50 mmol/L 24 h尿量减少,不良事件增多 Ferreira,et al(2016) 第3天 100 UNa>60 mmol/L UNa/UK>2 不良事件减少 Testani,et al(2016) 1~2 h 50 UNa < 60 mmol/L 不良事件发生率升高 Luk,et al(2018) 首次排尿 103 UNa < 60 mmol/L 不良临床事件升高 Brinkley,et al(2018) 首次排尿 176 UNa < 60 mmol/L 30 d住院或急诊率升高 Collins,et al(2018) 1 h 61 UNa < 35 mmol/L 恶化性HF -
[1] Mcdonagh TA, Metra M, Adamo M, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure[J]. Eur Heart J, 2021, 42(36): 3599-3726. doi: 10.1093/eurheartj/ehab368
[2] 董蔚, 任景怡, 徐东杰. 心力衰竭患者利尿剂抵抗诊断及管理中国专家共识[J]. 临床心血管病杂志, 2024, 40(4): 257-267. doi: 10.13201/j.issn.1001-1439.2024.04.002
[3] Gupta R, Testani J, Collins S. Diuretic Resistance in Heart Failure[J]. Curr Heart Fail Rep, 2019, 16(2): 57-66. doi: 10.1007/s11897-019-0424-1
[4] Testani JM, Brisco MA, Turner JM, et al. Loop diuretic efficiency: a metric of diuretic responsiveness with prognostic importance in acute decompensated heart failure[J]. Circ Heart Fail, 2014, 7(2): 261-270. doi: 10.1161/CIRCHEARTFAILURE.113.000895
[5] Alevroudis I, Kotoulas SC, Tzikas S, et al. Congestion in Heart Failure: From the Secret of a Mummy to Today's Novel Diagnostic and Therapeutic Approaches: A Comprehensive Review[J]. J Clin Med, 2023, 13(1): 12. doi: 10.3390/jcm13010012
[6] Singh D, Shrestha K, Testani JM, et al. Insufficient natriuretic response to continuous intravenous furosemide is associated with poor long-term outcomes in acute decompensated heart failure[J]. J Card Fail, 2014, 20(6): 392-399. doi: 10.1016/j.cardfail.2014.03.006
[7] Ferreira JP, Girerd N, Medeiros PB, et al. Spot urine sodium excretion as prognostic marker in acutely decompensated heart failure: the spironolactone effect[J]. Clin Res Cardiol, 2016, 105(6): 489-507. doi: 10.1007/s00392-015-0945-x
[8] Luk A, Groarke JD, Desai AS, et al. First spot urine sodium after initial diuretic identifies patients at high risk for adverse outcome after heart failure hospitalization[J]. Am Heart J, 2018, 203: 95-100. doi: 10.1016/j.ahj.2018.01.013
[9] Brinkley DM, Jr Burpee LJ, Chaudhry SP, et al. Spot Urine Sodium as Triage for Effective Diuretic Infusion in an Ambulatory Heart Failure Unit[J]. J Card Fail, 2018, 24(6): 349-354. doi: 10.1016/j.cardfail.2018.01.009
[10] Collins SP, Jenkins CA, Baughman A, et al. Early urine electrolyte patterns in patients with acute heart failure[J]. ESC Heart Fail, 2019, 6(1): 80-88. doi: 10.1002/ehf2.12368
[11] Doering A, Jenkins CA, Storrow AB, et al. Markers of diuretic resistance in emergency department patients with acute heart failure[J]. Int J Emerg Med, 2017, 10(1): 17. doi: 10.1186/s12245-017-0143-x
[12] Mullens W, Abrahams Z, Francis GS, et al. Importance of venous congestion for worsening of renal function in advanced decompensated heart failure[J]. J Am Coll Cardiol, 2009, 53(7): 589-596. doi: 10.1016/j.jacc.2008.05.068
[13] Felker GM, Ellison DH, Mullens W, et al. Diuretic Therapy for Patients With Heart Failure: JACC State-of-the-Art Review[J]. J Am Coll Cardiol, 2020, 75(10): 1178-1195. doi: 10.1016/j.jacc.2019.12.059
[14] Ter Maaten JM, Rao VS, Hanberg JS, et al. Renal tubular resistance is the primary driver for loop diuretic resistance in acute heart failure[J]. Eur J Heart Fail, 2017, 19(8): 1014-1022. doi: 10.1002/ejhf.757
[15] Cox ZL, Rao VS, Ivey-Miranda JB, et al. Compensatory post-diuretic renal sodium reabsorption is not a dominant mechanism of diuretic resistance in acute heart failure[J]. Eur Heart J, 2021, 42(43): 4468-4477. doi: 10.1093/eurheartj/ehab620
[16] Minegishi S, Luft FC, Titze J, et al. Sodium Handling and Interaction in Numerous Organs[J]. Am J Hypertens, 2020, 33(8): 687-694. doi: 10.1093/ajh/hpaa049
[17] Bjornstad P, Greasley PJ, Wheeler DC, et al. The Potential Roles of Osmotic and Nonosmotic Sodium Handling in Mediating the Effects of Sodium-Glucose Cotransporter 2 Inhibitors on Heart Failure[J]. J Card Fail, 2021, 27(12): 1447-1455. doi: 10.1016/j.cardfail.2021.07.003
[18] Boorsma EM, Ter Maaten JM, Damman K, et al. Congestion in heart failure: a contemporary look at physiology, diagnosis and treatment[J]. Nat Rev Cardiol, 2020, 17(10): 641-655. doi: 10.1038/s41569-020-0379-7
[19] Frea S, Pidello S, Volpe A, et al. Diuretic treatment in high-risk acute decompensation of advanced chronic heart failure-bolus intermittent vs. continuous infusion of furosemide: a randomized controlled trial[J]. Clin Res Cardiol, 2020, 109(4): 417-425. doi: 10.1007/s00392-019-01521-y
[20] Wilcox CS, Testani JM, Pitt B. Pathophysiology of Diuretic Resistance and Its Implications for the Management of Chronic Heart Failure[J]. Hypertension, 2020, 76(4): 1045-1054. doi: 10.1161/HYPERTENSIONAHA.120.15205
[21] Brisco-Bacik MA, Ter Maaten JM, Houser SR, et al. Outcomes Associated With a Strategy of Adjuvant Metolazone or High-Dose Loop Diuretics in Acute Decompensated Heart Failure: A Propensity Analysis[J]. J Am Heart Assoc, 2018, 7(18): e009149. doi: 10.1161/JAHA.118.009149
[22] Yeoh SE, Osmanska J, Petrie MC, et al. Dapagliflozin vs. metolazone in heart failure resistant to loop diuretics[J]. Eur Heart J, 2023, 44(31): 2966-2977. doi: 10.1093/eurheartj/ehad341
[23] Trullàs JC, Morales-Rull JL, Casado J, et al. Combining loop with thiazide diuretics for decompensated heart failure: the CLOROTIC trial[J]. Eur Heart J, 2023, 44(5): 411-421. doi: 10.1093/eurheartj/ehac689
[24] Isaksson GL, Hinrichs GR, Andersen H, et al. Amiloride Reduces Urokinase/Plasminogen-Driven Intratubular Complement Activation in Glomerular Proteinuria[J]. J Am Soc Nephrol, 2024, 35(4): 410-425. doi: 10.1681/ASN.0000000000000312
[25] Almajid AN, Patel P, Cassagnol M. Amiloride[M]. StatPearls. Treasure Island (FL). StatPearls Publishing CopyrightⒸ 2024, StatPearls Publishing LLC. 2024.
[26] Pratama V, Budiono J, Thobari JA, et al. The role of tolvaptan add-on therapy in patients with acute heart failure: a systematic review and network meta-analysis[J]. Front Cardiovasc Med, 2024, 11: 1367442. doi: 10.3389/fcvm.2024.1367442
[27] Pan Y, Li H, Gao J, et al. Tolvaptan for water retention in heart failure: a systematic review[J]. Syst Rev, 2023, 12(1): 130. doi: 10.1186/s13643-023-02293-3
[28] Butler J, Anstrom KJ, Felker GM, et al. Efficacy and Safety of Spironolactone in Acute Heart Failure: The ATHENA-HF Randomized Clinical Trial[J]. JAMA Cardiol, 2017, 2(9): 950-958. doi: 10.1001/jamacardio.2017.2198
[29] Bansal S, Munoz K, Brune S, et al. High-Dose Spironolactone When Patients With Acute Decompensated Heart Failure Are Resistant to Loop Diuretics: A Pilot Study[J]. Ann Intern Med, 2019, 171(6): 443-447. doi: 10.7326/M18-3285
[30] Mullens W, Dauw J, Martens P, et al. Acetazolamide in Acute Decompensated Heart Failure with Volume Overload[J]. N Engl J Med, 2022, 387(13): 1185-1195. doi: 10.1056/NEJMoa2203094
[31] Martens P, Testani J, Damman K. Prevention and treatment of diuretic resistance in acute heart failure: when to use which combination of diuretics?[J]. Eur Heart J, 2023, 44(31): 2978-2981. doi: 10.1093/eurheartj/ehad463
[32] Kuriyama A, Urushidani S. Continuous versus intermittent administration of furosemide in acute decompensated heart failure: a systematic review and meta-analysis[J]. Heart Fail Rev, 2019, 24(1): 31-39. doi: 10.1007/s10741-018-9727-7
[33] Alsalem A, Alsultan MM, Alqarni F, et al. Real-world evidence of the effects of sodium-glucose co-transporter 2 inhibitors on the dosing of diuretics in patients with heart failure: a retrospective cohort study[J]. Front Pharmacol, 2024, 15: 1366439. doi: 10.3389/fphar.2024.1366439
[34] Griffin M, Rao VS, Ivey-Miranda J, et al. Empagliflozin in Heart Failure: Diuretic and Cardiorenal Effects[J]. Circulation, 2020, 142(11): 1028-1039. doi: 10.1161/CIRCULATIONAHA.120.045691
[35] Stachteas P, Nasoufidou A, Patoulias D, et al. The Role of Sodium-Glucose Co-Transporter-2 Inhibitors on Diuretic Resistance in Heart Failure[J]. Int J Mol Sci, 2024, 25(6): 3122. doi: 10.3390/ijms25063122
[36] Goyfman M, Zamudio P, Jang K, et al. Combined aquaretic and diuretic therapy in acute heart failure[J]. Int J Nephrol Renovasc Dis, 2017, 10: 129-134. doi: 10.2147/IJNRD.S135660
[37] Cox ZL, Sarrell BA, Cella MK, et al. Multinephron Segment Diuretic Therapy to Overcome Diuretic Resistance in Acute Heart Failure: A Single-Center Experience[J]. J Card Fail, 2022, 28(1): 21-31. doi: 10.1016/j.cardfail.2021.07.016
[38] Cao W, Zhou QG, Nie J, et al. Albumin overload activates intrarenal renin-angiotensin system through protein kinase C and NADPH oxidase-dependent pathway[J]. J Hypertens, 2011, 29(7): 1411-1421. doi: 10.1097/HJH.0b013e32834786f0
[39] Chen HH, Anstrom KJ, Givertz MM, et al. Low-dose dopamine or low-dose nesiritide in acute heart failure with renal dysfunction: the ROSE acute heart failure randomized trial[J]. JAMA, 2013, 310(23): 2533-2543. doi: 10.1001/jama.2013.282190
[40] Gentile P, Marini C, Ammirati E, et al. Long-term administration of intravenous inotropes in advanced heart failure[J]. ESC Heart Fail, 2021, 8(5): 4322-4327. doi: 10.1002/ehf2.13394
[41] Griffin M, Soufer A, Goljo E, et al. Real World Use of Hypertonic Saline in Refractory Acute Decompensated Heart Failure: A U.S. Center's Experience[J]. JACC Heart Fail, 2020, 8(3): 199-208. doi: 10.1016/j.jchf.2019.10.012
[42] Colin-Ramirez E, Sepehrvand N, Rathwell S, et al. Sodium Restriction in Patients With Heart Failure: A Systematic Review and Meta-Analysis of Randomized Clinical Trials[J]. Circ Heart Fail, 2023, 16(1): e009879.
[43] Srivastava M, Harrison N, Caetano AFS, et al. Ultrafiltration for acute heart failure[J]. Cochrane Database Syst Rev, 2022, 1(1): Cd013593.
-

计量
- 文章访问数: 302
- 施引文献: 0




 下载:
下载: