-
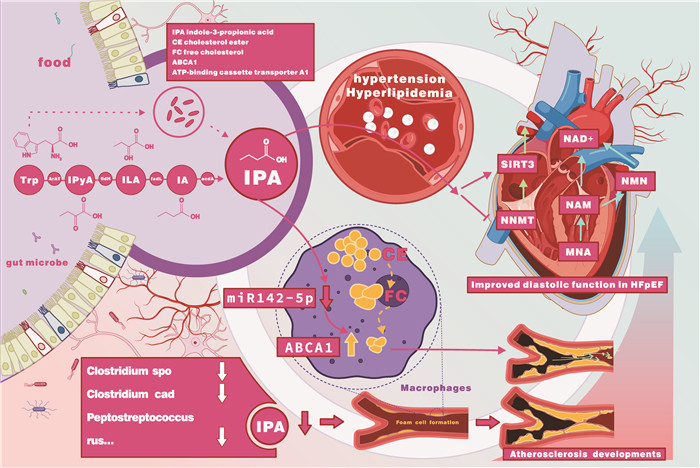
摘要: 心血管疾病(CVD)是全球健康的主要威胁,与肠道微生物代谢物吲哚丙酸(IPA)密切相关。本文综述了IPA的来源、代谢过程及其在CVD中的作用,强调肠-心轴的重要性,并讨论了IPA对肠道屏障功能和内毒素的影响。IPA是色氨酸的代谢产物,其水平受肠道细菌、饮食习惯和遗传因素影响。肠-心轴揭示了肠道微生物与心血管系统间的双向作用,IPA在其中扮演核心角色,与血压调节、抗炎、代谢平衡及动脉粥样硬化相关。Abstract: Cardiovascular diseases(CVD) are a major global health threat, and closely related to the gut microbial metabolite indole-3-propionic acid(IPA). This article reviews the sources, metabolic processes of IPA, and its role in CVD. We emphasized the importance of the gut-heart axis and discussed the impact of IPA on intestinal barrier function and endotoxin leakage. IPA is a metabolite of tryptophan, and its levels are influenced by gut bacteria, dietary habits, and genetic factors. The gut-heart axis reveals the bidirectional interaction between the gut microbiota and the cardiovascular system. IPA played a central role in blood pressure regulation, anti-inflammation, metabolic balance, and atherosclerosis.
-
Key words:
- cardiovascular diseases /
- gut microbiota /
- indole-3-propionic acid
-

-
[1] Wen YN, Sun ZF, Xie SY, et al. Intestinal flora derived metabolites affect the occurrence and development of cardiovascular disease[J]. J Multidiscip Healthc, 2022, 15: 2591-2603. doi: 10.2147/JMDH.S367591
[2] 刘明波, 何新叶, 杨晓红, 等. 《中国心血管健康与疾病报告2023》要点解读[J]. 临床心血管病杂志, 2024, 40(8): 599-616. doi: 10.3969/j.issn.1007-5410.2024.04.002
[3] Beloborodova NV, Chernevskaya EA, Getsina ML. Indolic structure metabolites as potential biomarkers of non-infectious diseases[J]. Curr Pharm Des, 2021, 27(2): 238-249. doi: 10.2174/1381612826666201022121653
[4] Hyland NP, Cavanaugh CR, Hornby PJ. Emerging effects of tryptophan pathway metabolites and intestinal microbiota on metabolism and intestinal function[J]. Amino Acids, 2022, 54(1): 57-70. doi: 10.1007/s00726-022-03123-x
[5] Zhang BB, Jiang MJ, Zhao JN, et al. The mechanism underlying the influence of indole-3-propionic acid: a relevance to metabolic disorders[J]. Front Endocrinol(Lausanne), 2022, 13: 841703. doi: 10.3389/fendo.2022.841703
[6] Ballanti M, Antonetti L, Mavilio M, et al. Decreased circulating IPA levels identify subjects with metabolic comorbidities: a multi-omics study[J]. Pharmacol Res, 2024, 204: 107207. doi: 10.1016/j.phrs.2024.107207
[7] Qi QB, Li J, Yu B, et al. Host and gut microbial tryptophan metabolism and type 2 diabetes: an integrative analysis of host genetics, diet, gut microbiome and circulating metabolites in cohort studies[J]. Gut, 2022, 71(6): 1095-1105. doi: 10.1136/gutjnl-2021-324053
[8] Zhang YX, Wang Y, Ke BB, et al. TMAO: how gut microbiota contributes to heart failure[J]. Transl Res, 2021, 228: 109-125. doi: 10.1016/j.trsl.2020.08.007
[9] Sulaiman D, Reddy ST, Fogelman AM. Evidence further linking the intestine to cardiovascular disease[J]. Curr Opin Lipidol, 2024, 35(5): 223-227. doi: 10.1097/MOL.0000000000000944
[10] Li Q, You YR, Zeng YP, et al. Associations between plasma tryptophan and indole-3-propionic acid levels and mortality in patients with coronary artery disease[J]. Am J Clin Nutr, 2022, 116(4): 1070-1077. doi: 10.1093/ajcn/nqac170
[11] 实用心脑肺血管病杂志编辑部. 数据"说"心血管病[J]. 实用心脑肺血管病杂志, 2024, 32(9): 5.
[12] Yang YZ, Karampoor S, Mirzaei R, et al. The interplay between microbial metabolites and macrophages in cardiovascular diseases: a comprehensive review[J]. Int Immunopharmacol, 2023, 121: 110546. doi: 10.1016/j.intimp.2023.110546
[13] Adua E. Decoding the mechanism of hypertension through multiomics profiling[J]. J Hum Hypertens, 2023, 37(4): 253-264.
[14] Zhou JD, Hao JJ, Zhong ZQ, et al. Fecal microbiota transplantation in mice exerts a protective effect against doxorubicin-induced cardiac toxicity by regulating Nrf2-mediated cardiac mitochondrial fission and fusion[J]. Antioxid Redox Signal, 2024, 41(1-3): 1-23. doi: 10.1089/ars.2023.0355
[15] Jennis M, Cavanaugh CR, Leo GC, et al. Microbiota-derived tryptophan indoles increase after gastric bypass surgery and reduce intestinal permeability in vitro and in vivo[J]. Neurogastroenterol Motil, 2018, 30(2): 110.
[16] Konopelski P, Chabowski D, Aleksandrowicz M, et al. Indole-3-propionic acid, a tryptophan-derived bacterial metabolite, increases blood pressure via cardiac and vascular mechanisms in rats[J]. Am J Physiol Regul Integr Comp Physiol, 2021, 321(6): R969-R981. doi: 10.1152/ajpregu.00142.2021
[17] Huc T, Konop M, Onyszkiewicz M, et al. Colonic indole, gut bacteria metabolite of tryptophan, increases portal blood pressure in rats[J]. Am J Physiol Regul Integr Comp Physiol, 2018, 315(4): R646-R655. doi: 10.1152/ajpregu.00111.2018
[18] Yisireyili M, Takeshita K, Saito S, et al. Indole-3-propionic acid suppresses indoxyl sulfate-induced expression of fibrotic and inflammatory genes in proximal tubular cells[J]. Nagoya J Med Sci, 2017, 79(4): 477-486.
[19] Paeslack N, Mimmler M, Becker S, et al. Microbiota-derived tryptophan metabolites in vascular inflammation and cardiovascular disease[J]. Amino Acids, 2022, 54(10): 1339-1356. doi: 10.1007/s00726-022-03161-5
[20] Gesper M, Nonnast ABH, Kumowski N, et al. Gut-derived metabolite indole-3-propionic acid modulates mitochondrial function in cardiomyocytes and alters cardiac function[J]. Front Med(Lausanne), 2021, 8: 648259.
[21] Baranwal G, Goodlett BL, Arenaz CM, et al. Indole propionic acid increases T regulatory cells and decreases T helper 17 cells and blood pressure in mice with salt-sensitive hypertension[J]. Int J Mol Sci, 2023, 24(11): 9192. doi: 10.3390/ijms24119192
[22] Meng HY, Ruan JJ, Yan ZH, et al. New progress in early diagnosis of atherosclerosis[J]. Int J Mol Sci, 2022, 23(16): 8939. doi: 10.3390/ijms23168939
[23] Kumar Vinay. 病理学[M]. 北京: 北京大学医学出版社, 2023: 110.
[24] Geddo F, Antoniotti S, Gallo MP, et al. Indole-3-propionic acid, a gut microbiota-derived tryptophan metabolite, promotes endothelial dysfunction impairing purinergic-induced nitric oxide release in endothelial cells[J]. Int J Mol Sci, 2024, 25(6): 3389. doi: 10.3390/ijms25063389
[25] Xue HL, Chen X, Yu C, et al. Gut microbially produced indole-3-propionic acid inhibits atherosclerosis by promoting reverse cholesterol transport and its deficiency is causally related to atherosclerotic cardiovascular disease[J]. Circ Res, 2022, 131(5): 404-420. doi: 10.1161/CIRCRESAHA.122.321253
[26] Zhang YQ, Li SS, Fan XJ, et al. Pretreatment with indole-3-propionic acid attenuates lipopolysaccharide-induced cardiac dysfunction and inflammation through the AhR/NF-κB/NLRP3 pathway[J]. J Inflamm Res, 2024, 17: 5293-5309. doi: 10.2147/JIR.S466777
[27] Teunis C, Nieuwdorp M, Hanssen N. Interactions between tryptophan metabolism, the gut microbiome and the immune system as potential drivers of non-alcoholic fatty liver disease(NAFLD)and metabolic diseases[J]. Metabolites, 2022, 12(6): 514. doi: 10.3390/metabo12060514
[28] Poznyak AV, Ivanova EA, Sobenin IA, et al. The role of mitochondria in cardiovascular diseases[J]. Biology(Basel), 2020, 9(6): 137.
[29] Cason CA, Dolan KT, Sharma G, et al. Plasma microbiome-modulated indole-and phenyl-derived metabolites associate with advanced atherosclerosis and postoperative outcomes[J]. J Vasc Surg, 2018, 68(5): 1552-1562. e7. doi: 10.1016/j.jvs.2017.09.029
[30] 中华医学会心血管病学分会, 中国医师协会心血管内科医师分会, 中国医师协会心力衰竭专业委员会, 等. 中国心力衰竭诊断和治疗指南2024[J]. 中华心血管病杂志, 2024, 52(3): 235-275.
[31] Vlasov AA, Salikova SP, Grinevich VB, et al. Gut microbiota and systemic inflammation in patients with chronic heart failure[J]. Kardiologiia, 2020, 60(5): 859.
[32] Chen AT, Zhang J, Zhang YH. Gut microbiota in heart failure and related interventions[J]. Imeta, 2023, 2(3): e125. doi: 10.1002/imt2.125
[33] Masenga SK, Povia JP, Lwiindi PC, et al. Recent advances in microbiota-associated metabolites in heart failure[J]. Biomedicines, 2023, 11(8): 2313. doi: 10.3390/biomedicines11082313
[34] Wlodarska M, Luo CW, Kolde R, et al. Indoleacrylic acid produced by commensal Peptostreptococcus species suppresses inflammation[J]. Cell Host Microbe, 2017, 22(1): 25-37. e6. doi: 10.1016/j.chom.2017.06.007
[35] Chen Y, Li Y, Li XJ, et al. Indole-3-propionic acid alleviates intestinal epithelial cell injuryviaregulation of the TLR4/NF-κB pathway to improve intestinal barrier function[J]. Mol Med Rep, 2024, 30(4): 189. doi: 10.3892/mmr.2024.13313
[36] Vacca A, Schiattarella GG. From gut to heart: role of indole-3-propionic acid in HFpEF[J]. Circ Res, 2024, 134(4): 390-392. doi: 10.1161/CIRCRESAHA.123.323947
[37] Wang YC, Koay YC, Pan C, et al. Indole-3-propionic acid protects against heart failure with preserved ejection fraction[J]. Circ Res, 2024, 134(4): 371-389. doi: 10.1161/CIRCRESAHA.123.322381
[38] Li C, Chang J, Wang Y, et al. Indole-3-propionic acid, a product of intestinal flora, inhibits the HDAC6/NOX2 signaling and relieves doxorubicin-induced cardiomyocyte damage[J]. Folia Morphol(Warsz), 2023, 83(2): 382-390.
[39] 涂哲禹, 苏丰贺, 王艺婷, 等. 急性心力衰竭代谢标志物的研究进展[J]. 中华医学杂志, 2023, 103(1): 67-70.
[40] Kretzschmar T, Westphal J, Neugebauer S, et al. Metabolic profiling identifies 1-MetHis and 3-IPA as potential diagnostic biomarkers for patients with acute and chronic heart failure with reduced ejection fraction[J]. Circ Heart Fail, 2024, 17(1): e010813.
[41] Li JJ, Zhang L, Wu T, et al. Indole-3-propionic acid improved the intestinal barrier by enhancing epithelial barrier and mucus barrier[J]. J Agric Food Chem, 2021, 69(5): 1487-1495. doi: 10.1021/acs.jafc.0c05205
[42] Wu Y, Li JJ, Ding WJ, et al. Enhanced intestinal barriers by puerarin in combination with tryptophan[J]. J Agric Food Chem, 2021, 69(51): 15575-15584. doi: 10.1021/acs.jafc.1c05830
[43] Wang K, Lai WW, Min TQ, et al. The effect of enteric-derived lipopolysaccharides on obesity[J]. Int J Mol Sci, 2024, 25(8): 4305. doi: 10.3390/ijms25084305
[44] Liberale L, Badimon L, Montecucco F, et al. Inflammation, aging, and cardiovascular disease: JACC review topic of the week[J]. J Am Coll Cardiol, 2022, 79(8): 837-847. doi: 10.1016/j.jacc.2021.12.017
[45] Chen Y, Li YP, Liu MQ, et al. Association between systemic immunity-inflammation index and hypertension in US adults from NHANES 1999-2018[J]. Sci Rep, 2024, 14(1): 5677. doi: 10.1038/s41598-024-56387-6
[46] Soysal P, Arik F, Smith L, et al. Inflammation, frailty and cardiovascular disease[J]. Adv Exp Med Biol, 2020, 1216: 55-64.
[47] Boulet J, Sridhar VS, Bouabdallaoui N, et al. Inflammation in heart failure: pathophysiology and therapeutic strategies[J]. Inflamm Res, 2024, 73(5): 709-723.
[48] Dang KK, Wang XY, Hu JX, et al. The association between triglyceride-glucose index and its combination with obesity indicators and cardiovascular disease: NHANES 2003-2018[J]. Cardiovasc Diabetol, 2024, 23(1): 8.
[49] Kim KS, Hong SM, Han K, et al. Association of non-alcoholic fatty liver disease with cardiovascular disease and all cause death in patients with type 2 diabetes mellitus: nationwide population based study[J]. BMJ, 2024, 384: e076388.
[50] Yang M, Cai WH, Li XX, et al. The effect of type 2 resistant starch and indole-3-propionic acid on ameliorating high-fat-diet-induced hepatic steatosis and gut dysbiosis[J]. Foods, 2024, 13(11): 1625.
[51] Li YG, Xu WY, Zhang F, et al. The gut microbiota-produced indole-3-propionic acid confers the antihyperlipidemic effect of mulberry-derived 1-deoxynojirimycin[J]. mSystems, 2020, 5(5): e00313-00320.
[52] Peron G, Merono T, Gargari G, et al. A polyphenol-rich diet increases the gut microbiota metabolite indole 3-propionic acid in older adults with preserved kidney function[J]. Mol Nutr Food Res, 2022, 66(21): e2100349.
[53] Xie Y, Li X, Meng Q, et al. Interplay between gut microbiota and tryptophan metabolism in type 2 diabetic mice treated with metformin[J]. Microbiol Spectr, 2024, 12(10): e0029124.
-

计量
- 文章访问数: 37
- 施引文献: 0



 下载:
下载: