Analysis of risk factors for mortality in obese patients with chronic heart failure and modeling of column-line diagrams
-
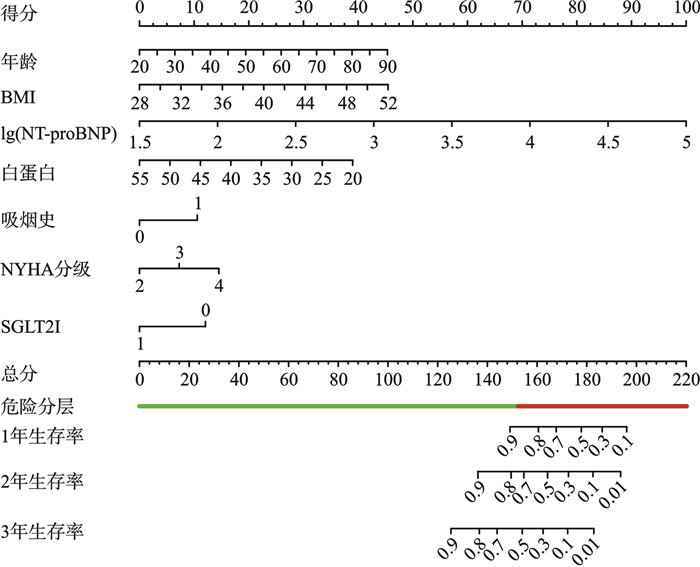
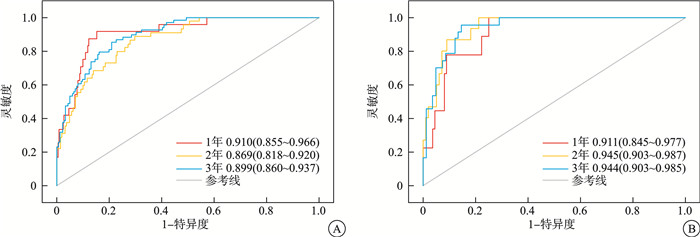
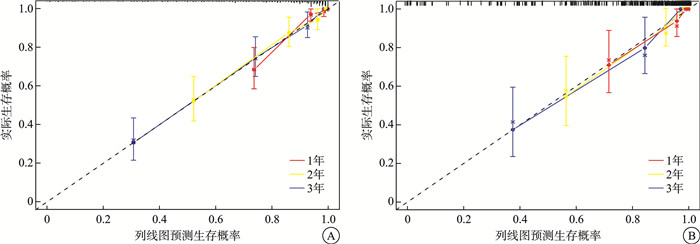
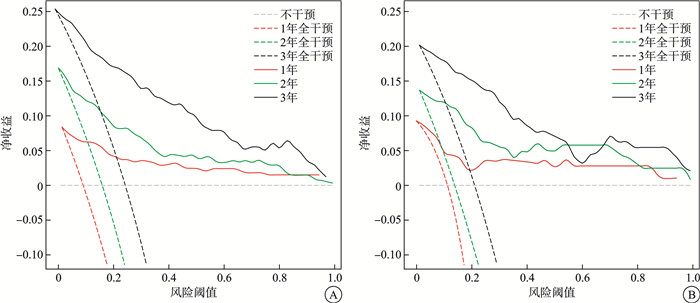
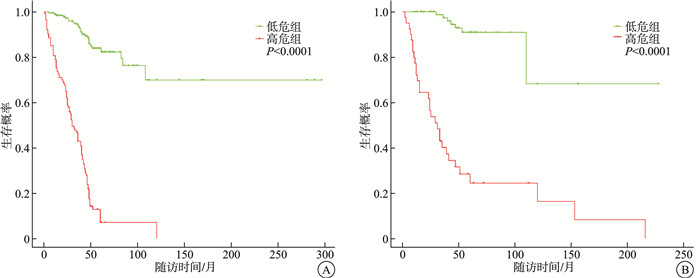
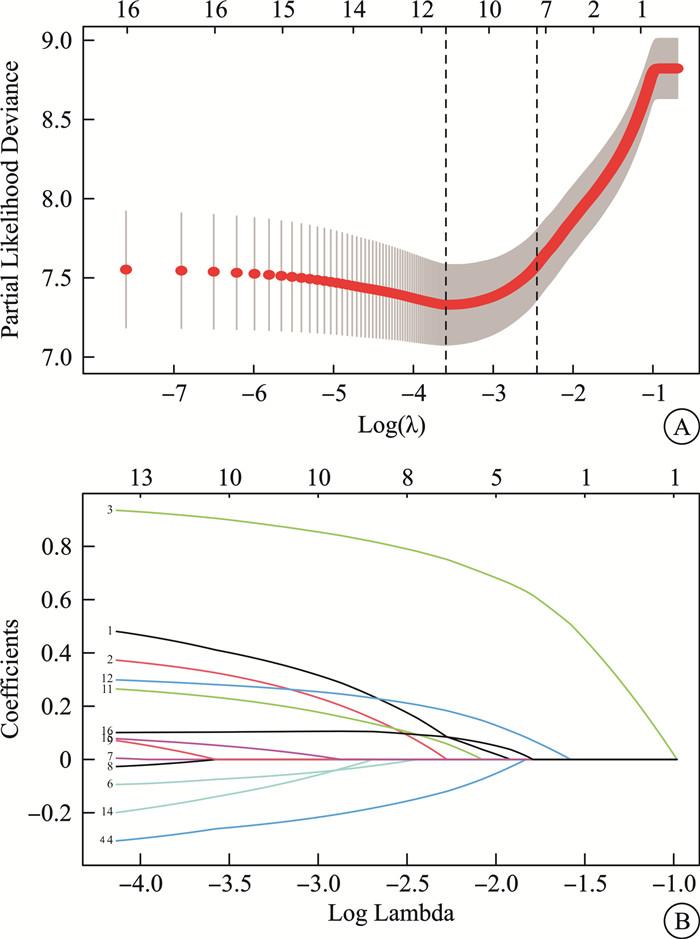
摘要: 目的 探讨肥胖慢性心力衰竭(CHF)患者全因死亡的影响因素,构建列线图模型用于预测其1年、2年、3年的全因死亡率。 方法 选择2019年12月—2023年12月石河子大学第一附属医院BMI≥28 kg/m2的CHF住院患者421例,以全因死亡为终点事件,随访截至2024年7月1日。将其以7∶3比例随机分为训练集和验证集。利用LASSO回归及Cox回归分析患者全因死亡的因素,R4.4.0建立列线图模型。受试者工作曲线下面积(AUC)、C指数(C-index)及校准曲线用于评估模型的区分度和预测效能。绘制临床决策曲线(DCA)评估模型的临床应用价值。用受试者工作特征曲线技术确定最佳风险截断阈值并进行死亡风险分层。绘制不同风险组的Kaplan-Meier生存曲线并比较组间的生存差异。 结果 多因素Cox回归分析提示,年龄(HR=1.040,95%CI 1.020~1.060,P < 0.001)、lg(NT-proBNP)(HR=5.650,95%CI 3.350~9.510,P < 0.001)、BMI(HR=1.130,95%CI 1.080~1.190,P < 0.001)增加、合并吸烟史(HR=1.990,95%CI 1.340~2.940,P=0.001)及NYHA分级Ⅳ级(HR=3.480,95%CI 1.610~7.530,P=0.002)是患者全因死亡的危险因素,而白蛋白(HR=0.921,95%CI 0.882~0.961,P < 0.001)水平升高和服用SGLT2i类药物(HR=0.414,95%CI 0.189~0.906,P=0.027)可降低全因死亡风险。以此构建的模型验证集C-index为0.895,1、3、5年生存期预测模型的AUC为0.911、0.945、0.944。校准曲线与实际生存情况贴合较好,DCA曲线结果提示模型有较好的临床适用性。风险分层可以有效区分高、低危患者的预后。 结论 年龄、BMI、吸烟史、NYHA分级、NT-proBNP、白蛋白、SGLT2i类药物是影响肥胖CHF患者全因死亡的独立预后因子,根据其构建的列线图模型有助于临床医师早期识别高危肥胖CHF患者,并给予个性化治疗方案。Abstract: Objective To explore the influencing factors of all-cause death in obese patients with chronic heart failure, and construct a nomogram model to predict their all-cause mortality at 1 year, 2 years and 3 years. Methods The 421 chronic heart failure inpatients with BMI ≥28 kg/m2 in the First Affiliated Hospital of Shihezi University from December 2019 to December 2023 were selected, with all-cause death as the endpoint event, and followed up until July 1, 2024. They were randomized into training and validation sets in a 7: 3 ratio. LASSO regression and Cox regression were used to analyze the factors of all-cause mortality in patients, and R4.4.0 was used to establish a nomogram model. The area under the working curve(AUC), C-index and calibration curves of the subjects were used to assess the discrimination and predictive efficacy of the model. Clinical decision curves(DCA) were plotted to assess the clinical applicability of the model. The optimal risk cut-off threshold was determined and stratified for mortality risk using the subject operating characteristic curve technique. Kaplan-Meier survival curves were plotted for different risk groups and survival differences between groups were compared. Results Multifactorial Cox regression analysis suggested that age(HR=1.040, 95%CI: 1.020-1.060)(P < 0.001), lg(NT-proBNP)(HR=5.650, 95%CI: 3.350-9.510)(P < 0.001), increased BMI(HR=1.130, 95%CI: 1.080-1.190)(P < 0.001), comorbid smoking history(HR=1.990, 95%CI: 1.340-2.940)(P=0.001) and NYHA classification Ⅳ(HR=3.480, 95%CI: 1.610-7.530)(P=0.002) were risk factors for all-cause mortality in patients, whereas increased albumin levels(HR=0.921, 95%CI: 0.882-0.961)(P < 0.001) and administration of SGLT2I analogs(HR=0.414, 95%CI: 0.189-0.906)(P=0.027) reduced the risk of all-cause mortality. The C-index of the model verification set was 0.895, and the AUC of the 1-, 3-and 5-year survival prediction models were 0.911, 0.945 and 0.944. The calibration curves fit well with the actual survival situation, and the results of the DCA curves suggested that the model had good clinical applicability. Risk stratification can effectively distinguish the prognosis of high-and low-risk patients. Conclusion Age, BMI, smoking history, NYHA classification, NT-proBNP, albumin and SGLT2I drugs are independent prognostic factors of all-cause mortality in obese CHF patients, and the column-line diagram model constructed based on them can help clinicians to identify high-risk obese CHF patients at an early stage and give them personalized treatment plans.
-
Key words:
- chronic heart failure /
- obesity /
- all-cause death /
- influencing factors /
- nomograms
-

-
表 1 生存组与死亡组患者基线资料的比较
Table 1. Basic data between surviving patients and dead patients
M(P25, P75), 例(%) 变量 生存组(257例) 死亡组(164例) Z/χ2 P 年龄/岁 58.00(50.00,73.00) 73.00(56.00,80.25) -6.27 < 0.001 男性 172(66.93) 108(65.85) 0.05 0.820 BMI/(kg/m2) 29.84(28.76,31.51) 31.11(29.32,33.31) -3.53 < 0.001 吸烟史 54(21.01) 68(41.46) 20.35 < 0.001 NYHA分级 61.80 < 0.001 Ⅱ 89(34.63) 10(6.10) Ⅲ 126(49.03) 83(50.61) Ⅳ 42(16.34) 71(43.29) lg(NT-proBNP)/(pg/mL) 3.16(2.79,3.51) 3.84(3.63,4.05) -13.45 < 0.001 白蛋白/(g/L) 40.80(37.50,43.10) 37.80(34.90,41.20) -5.02 < 0.001 尿素/(mmol/L) 6.75(5.40,8.20) 7.51(5.76,10.15) -3.16 0.002 尿酸/(μmol/L) 424.00(347.80,514.00) 436.00(344.75,560.85) -1.05 0.295 肌酐/(μmol/L) 80.40(66.30,97.30) 86.50(69.77,123.55) -3.05 0.002 eGFR/(mL/min/1.73m2) 83.63(64.63,97.80) 65.12(43.17,84.17) -6.13 < 0.001 血钾/(mmol/L) 3.97(3.73,4.29) 4.11(3.80,4.36) -2.45 0.014 血钠/(mmol/L) 140.30(138.40,142.50) 139.00(136.40,141.70) -3.28 0.001 血红蛋白/(g/L) 143.00(128.00,156.00) 136.00(122.75,146.25) -3.46 < 0.001 NLR 2.65(1.94,3.67) 3.35(2.23,5.09) -4.39 < 0.001 LVEF/% 43(34,56.) 39(32,50) -2.23 0.026 利尿剂 220(85.60) 136(82.93) 0.55 0.459 ACEI/ARB 96(37.35) 53(32.32) 1.11 0.292 β受体阻滞剂 197(76.65) 103(62.80) 9.38 0.002 ARNI 115(44.75) 48(29.27) 10.11 0.001 SGLT2i 48(18.68) 7(4.27) 18.30 < 0.001 接受心脏手术治疗 51(19.84) 38(23.17) 0.66 0.415 高血压 172(66.93) 123(75.00) 3.11 0.078 糖尿病 89(34.63) 51(31.10) 0.56 0.453 冠心病 143(55.64) 114(69.51) 8.10 0.004 心房颤动 81(31.52) 84(51.22) 16.31 < 0.001 COPD 19(7.39) 42(25.61) 26.81 < 0.001 脑卒中 78(30.35) 69(42.07) 6.05 0.014 肾功能不全 52(20.23) 40(24.39) 1.01 0.314 注:接受心脏手术治疗包括经皮冠状动脉介入治疗、冠状动脉旁路移植术、植入起搏器、心脏射频消融术。ACEI/ARB:血管紧张素转换酶抑制剂/血管紧张素Ⅱ受体阻滞剂;ARNI:血管紧张素受体-脑啡肽酶抑制剂。 表 2 Cox回归单因素分析
Table 2. Univariate Cox regression analysis
变量 HR 95%CI P 年龄 1.032 1.018~1.047 < 0.001 男性 0.746 0.508~1.095 0.135 BMI 1.100 1.050~1.152 < 0.001 吸烟史 2.521 1.732~3.671 < 0.001 NYHA分级 Ⅱ 参考值 Ⅲ 6.199 2.671~14.384 < 0.001 Ⅳ 12.509 5.360~29.196 < 0.001 lg(NT-proBNP) 10.320 6.676~15.952 < 0.001 白蛋白 0.913 0.881~0.946 < 0.001 尿素 1.096 1.054~1.140 < 0.001 尿酸 1.000 0.999~1.001 0.795 肌酐 1.004 1.002~1.006 < 0.001 eGFR 0.980 0.973~0.988 < 0.001 血钾 1.505 1.043~2.171 0.029 血钠 0.934 0.892~0.978 0.003 NLR 1.028 0.999~1.057 0.058 血红蛋白 0.992 0.985~0.999 0.022 LVEF 0.992 0.979~1.005 0.210 高血压 1.442 0.943~2.206 0.091 心房颤动 2.300 1.597~3.312 < 0.001 冠心病 1.330 0.902~1.962 0.150 COPD 2.729 1.776~4.193 < 0.001 脑卒中 1.440 0.995~2.083 0.053 肾功能不全 1.348 0.883~2.058 0.166 糖尿病 0.710 0.476~1.060 0.094 SGLT2i 0.354 0.165~0.760 0.008 ACEI/ARB 0.714 0.485~1.050 0.087 β受体阻滞剂 0.688 0.469~1.010 0.056 利尿剂 0.922 0.550~1.543 0.757 ARNI 0.560 0.370~0.848 0.006 接受心脏手术治疗 0.943 0.606~1.469 0.796 表 3 Cox回归多因素分析
Table 3. Multiple Cox regression analysis
变量 HR 95%CI P 年龄 1.040 1.020~1.060 < 0.001 BMI 1.130 1.080~1.190 < 0.001 lg(NT-proBNP) 5.650 3.350~9.510 < 0.001 NYHA分级 Ⅲ 2.670 1.270~5.640 0.010 Ⅳ 3.480 1.610~7.530 0.002 吸烟史 1.990 1.340~2.940 0.001 白蛋白 0.921 0.882~0.961 < 0.001 SGLT2i 0.414 0.189~0.906 0.027 -
[1] 湖北省心血管内科医疗质量控制中心, 武汉医学会心血管病学分会心衰学组, 湖北省医师协会心血管内科医师分会, 等. 心力衰竭常见病因及合并症的基层处理专家建议[J]. 临床心血管病杂志, 2024, 40(3): 161-166. doi: 10.13201/j.issn.1001-1439.2024.03.001
[2] 许顶立, 宋霖. 《中国心力衰竭诊断和治疗指南2024》解读[J]. 临床心血管病杂志, 2024, 40(6): 437-439. doi: 10.13201/j.issn.1001-1439.2024.06.002
[3] Powell-Wiley TM, Poirier P, Burke LE, et al. Obesity and cardiovascular disease: a scientific statement from the american heart association[J]. Circulation, 2021, 143(21): e984-e1010.
[4] 国家心血管病中心. 中国心血管健康与疾病报告2023概要[J]. 中国循环杂志, 2024, 39(7): 625-660.
[5] Yang Y, Song L, Wang L, et al. Effect of body mass index trajectory on lifetime risk of cardiovascular disease in a Chinese population: A cohort study[J]. Nutr Metab Cardiovasc Dis, 2023, 33(3): 523-531. doi: 10.1016/j.numecd.2022.11.025
[6] Jiang CQ, Xu L, Zhang WS, et al. Adiposity and mortality in older Chinese: an 11-year follow-up of the Guangzhou Biobank Cohort Study[J]. Sci Rep, 2020, 10(1): 1924. doi: 10.1038/s41598-020-58633-z
[7] Wang Z, Yao L, Li D, et al. Mortality prediction system for heart failure with orthogonal relief and dynamic radius means[J]. Int J Med Inform, 2018, 115: 10-17. doi: 10.1016/j.ijmedinf.2018.04.003
[8] Gao Y, Bai X, Lu J, et al. Prognostic value of multiple circulating biomarkers for 2-year death in acute heart failure with preserved ejection fraction[J]. Front Cardiovasc Med, 2021, 8: 779282. doi: 10.3389/fcvm.2021.779282
[9] Komajda M, Carson PE, Hetzel S, et al. Factors associated with outcome in heart failure with preserved ejection fraction: findings from the Irbesartan in Heart Failure with Preserved Ejection Fraction Study(I-PRESERVE)[J]. Circ Heart Fail, 2011, 4(1): 27-35. doi: 10.1161/CIRCHEARTFAILURE.109.932996
[10] Pocock SJ, Ferreira JP, Packer M, et al. Biomarker-driven prognostic models in chronic heart failure with preserved ejection fraction: the EMPEROR-Preserved trial[J]. Eur J Heart Fail, 2022, 24(10): 1869-1878. doi: 10.1002/ejhf.2607
[11] Vergaro G, Gentile F, Meems LMG, et al. NT-proBNP for risk prediction in heart failure[J]. JACC: Heart Failure, 2021, 9(9): 653-663. doi: 10.1016/j.jchf.2021.05.014
[12] Wang H, Li Y, Chai K, et al. Mortality in patients admitted to hospital with heart failure in China: a nationwide Cardiovascular Association Database-Heart Failure Centre Registry cohort study[J]. Lancet Glob Health, 2024, 12(4): e611-e622. doi: 10.1016/S2214-109X(23)00605-8
[13] Savarese G, Becher PM, Lund LH, et al. Global burden of heart failure: a comprehensive and updated review of epidemiology[J]. Cardiovasc Res, 2023, 118(17): 3272-3287. doi: 10.1093/cvr/cvac013
[14] 杨明艳, 陈薇, 高扬, 等. 基于无创血流动力学参数预测老年慢性心力衰竭患者院内死亡的列线图构建与验证[J]. 中华老年心脑血管病杂志, 2024, 26(2): 124-127.
[15] Jurica J, Pec MJ, Benko J, et al. Obesity as a risk factor in atrial fibrillation and heart failure[J]. J Diabetes Metab Disord, 2024, 23(1): 125-134.
[16] 赵灿, 王刚, 刘霄燕, 等. BMI对慢性心力衰竭的预后价值[J]. 临床心血管病杂志, 2024, 40(3): 194-198. doi: 10.13201/j.issn.1001-1439.2024.03.007
[17] 中国营养学会肥胖防控分会. 中国居民肥胖防治专家共识[J]. 西安交通大学学报(医学版), 2022, 4(43): 619-631.
[18] Kitzman DW, Brubaker P, Morgan T, et al. Effect of caloric restriction or aerobic exercise training on peak oxygen consumption and quality of life in obese older patients with heart failure with preserved ejection fraction: a randomized clinical trial[J]. JAMA, 2016, 315(1): 36-46.
[19] Butler J, Shah SJ, Petrie MC, et al. Semaglutide versus placebo in people with obesity-related heart failure with preserved ejection fraction: a pooled analysis of the STEP-HFpEF and STEP-HFpEF DM randomised trials[J]. Lancet, 2024, 403(10437): 1635-1648.
[20] Liang L, Zhao X, Huang L, et al. Prevalence and prognostic importance of malnutrition, as assessed by four different scoring systems, in elder patients with heart failure[J]. Nutr Metab Cardiovasc Dis, 2023, 33(5): 978-986.
[21] Chien SC, Chandramouli C, Lo CI, et al. Associations of obesity and malnutrition with cardiac remodeling and cardiovascular outcomes in Asian adults: A cohort study[J]. PLoS Med, 2021, 18(6): e1003661.
[22] Armentaro G, Condoleo V, Pastura CA, et al. Prognostic role of serum albumin levels in patients with chronic heart failure[J]. Intern Emerg Med, 2024, 19(5): 1323-1333.
[23] 安宣齐, 张健, 周琼. 临床研究综述: 肥胖对心力衰竭的发展与转归的影响[J]. 中华心力衰竭和心肌病杂志, 2020, 4(3): 222-230.
[24] 田庄, 芦阳. 心力衰竭治疗进展[J]. 临床心血管病杂志, 2024, 40(4): 268-271. doi: 10.13201/j.issn.1001-1439.2024.04.003
[25] 杨敏, 殷跃辉, 陈芸霖, 等. 心力衰竭临床预后预测模型研究进展[J]. 心血管病学进展, 2023, 44(10): 878-882.
[26] 于丽, 郑超楠, 贾梦楠, 等. 心力衰竭中医风险评估预警模型的构建[J]. 中华中医药杂志, 2023, 11(38): 5447-5453.
-

计量
- 文章访问数: 35
- 施引文献: 0



 下载:
下载: