Application of left bundle branch pacing in heart failure with mildly reduced ejection fraction and left bundle branch block
-
摘要: 目的 探讨左束支起搏(LBBP)在完全性左束支传导阻滞(CLBBB)合并射血分数轻度降低型心力衰竭(HFmrEF)患者中的临床应用。 方法 连续入选2017年1月—2022年12月于浙江大学医学院附属邵逸夫医院符合CLBBB合并HFmrEF的患者78例,评估导线参数和超声心动图指标。 结果 51例患者成功行LBBP(LBBP组),27例患者仅指南导向药物治疗(GDMT组)。术中LBBP电极(0.7±0.3) V/0.4ms,R波感知幅度(6.1±4.5) mV,阻抗(584.1±165.3)Ω。术后QRS时限较术前差异有统计学意义[(120.0±16.3) ms vs (169.9±18.8) ms,P < 0.01]。随访2年,LBBP电极阈值、感知幅度均无明显差异。心功能分级及超声心动图参数LBBP组与GDMT组比较均有统计学差异。 结论 LBBP在CLBBB合并HFmrEF的患者中的应用是安全有效的。
-
关键词:
- 心脏起搏,人工 /
- 左束支起搏 /
- 完全性左束支传导阻滞 /
- 射血分数轻度降低型心力衰竭 /
- 机械同步性
Abstract: Objective To explore the clinical application of left bundle branch pacing(LBBP) in heart failure with mildly reduced ejection fraction(HFmrEF) and complete left bundle branch block(CLBBB). Methods We consecutively recruited 78 patients with HFmrEF and CLBBB from January 2017 to December 2022 in Sir Run Run Shaw Hospital, School of Medicine, Zhejiang University and explored LBBP parameter changes and clinical outcomes. Results Fifty-one patients received LBBP successfully, while twenty-seven patients received only guideline-directed medical therapy. The acute pacing threshold was(0.7±0.3) V/0.4ms, and the sensed potentials were(6.1±4.5) mV, and the impedance was(584.1±165.3) Ω. During follow-up of 24 months, the threshold and sensed potentials had no significant difference compared with the measurements at implantation respectively. Median NYHA functional class and echocardiography parameters improved in LBBP group compared with GDMT group. Conclusion LBBP is feasible and safe in patients with HFmrEF and CLBBB. -

-
表 1 两组术前基线资料
Table 1. General data
例(%), X±S 项目 LBBP组(51例) GDMT组(27例) P 年龄/岁 71.2±8.1 75.4±11.8 0.17 男性 33(64.7) 17(63.0) 0.88 BMI/(kg/m2) 26.0±1.6 25.2±8.2 0.28 NT-proBNP/(pg/mL) 3 337.9±3 650.8 3 298.4±3 860.1 0.45 QRS波时限/ms 169.9±18.8 171.5±16.1 0.78 心功能NYHA分级 2.5±0.7 2.4±0.8 0.98 6 min步行试验距离/m 362.7±108.5 348.1±102.6 0.83 LVEDd/mm 59.5±6.2 59.8±8.5 0.89 LVEF/% 44.3±2.9 44.9±3.6 0.44 合并疾病 高血压 35(68.6) 17(63.0) 0.62 糖尿病 21(41.2) 13(48.1) 0.56 冠心病 18(35.3) 13(48.1) 0.28 慢性肾功能不全 15(29.4) 9(33.3) 0.72 表 2 不同时间LBBP电极参数
Table 2. LBBP electrode parameters at different times
X±S 时间 阈值/V 感知幅度/mV 阻抗/Ω 术中基线 0.7±0.3 6.1±4.5 584.1±165.3 术后1个月 1.2±1.7 6.6±2.8 491.9±113.61) 术后3个月 1.2±1.6 6.2±2.7 493.9±91.71) 术后6个月 0.9±0.5 7.2±2.7 463.0±94.41) 术后1年及以上 0.9±0.3 7.5±4.0 471.8±77.01) 与术中基线比较,1)P < 0.05。 表 3 LBBP起搏前后的左心室及左右心室间同步性指标
Table 3. Indicators before and after LBBP pacing
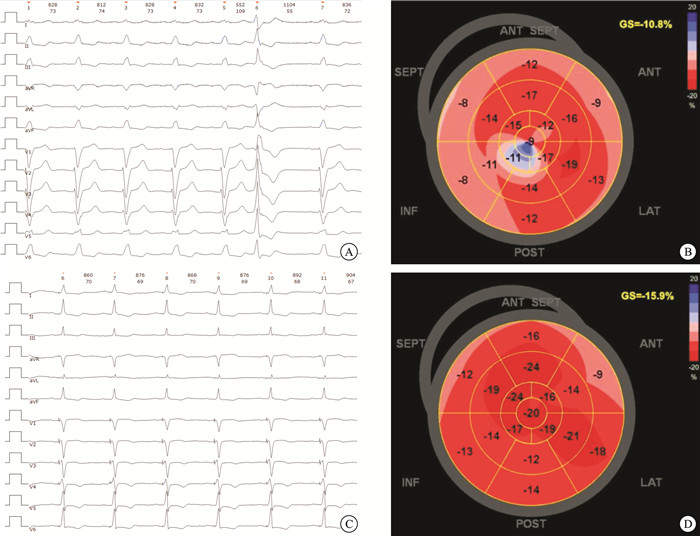
X±S 指标 术前 LBBP起搏后 P GLS/% -(11.1±9.4) -(15.4±4.0) 0.03 PSD/ms 101.4±46.8 78.3±25.3 < 0.01 IVMD>40ms/例(%) 31(72.1) 5(11.6) < 0.01 IVMD/ms 51.3±22.4 22.1±21.0 < 0.01 表 4 比较LBBP组与GDMT组心脏超声指标
Table 4. Cardiac ultrasound indicators between LBBP group and GDMT group
X±S 指标 LBBP组(51例) GDMT组(27例) P LVEF/% 基线 44.3±2.9 44.9±3.6 0.44 随访1个月 49.2±9.3 43.7±4.9 < 0.01 随访3个月 54.7±10.7 44.5±9.1 < 0.01 随访6个月 54.0±11.7 42.9±7.6 < 0.01 随访1年 54.4±10.9 41.7±11.4 < 0.01 随访2年 53.7±12.8 40.4±13.7 < 0.01 LVEDd/mm 基线 59.5±6.2 59.8±8.5 0.89 随访1个月 56.9±5.8 58.3±8.1 0.35 随访3个月 54.3±4.5 58.2±9.9 0.02 随访6个月 53.7±9.6 59.4±13.9 < 0.01 随访1年 53.0±7.9 59.7±11.8 < 0.01 随访2年 52.6±7.5 60.3±12.7 < 0.01 三尖瓣反流/(m/s) 基线 2.6±0.6 2.5±0.7 0.63 随访1个月 2.4±0.4 2.4±0.5 0.75 随访3个月 2.5±0.6 2.6±0.5 0.66 随访6个月 2.5±0.5 2.6±0.6 0.46 随访1年 2.4±0.6 2.5±0.4 0.72 随访2年 2.7±0.6 2.7±0.7 0.73 右室收缩压/mmHg 基线 33.0±13.9 30.5±8.3 0.79 随访1个月 28.5±7.5 32.3±8.7 0.23 随访3个月 30.8±12.6 33.8±16.5 0.72 随访6个月 30.8±10.0 32.9±10.6 0.53 随访1年 30.4±11.9 30.3±9.8 0.81 随访2年 32.8±18.1 32.6±18.7 0.29 -
[1] van Bommel RJ, Bax JJ, Abraham WT, et al. Characteristics of heart failure patients associated with good and poor response to cardiac resynchronization therapy: a PROSPECT(Predictors of Responseto CRT)sub-analysis[J]. Eur Heart J, 2009, 30: 2470-2477. doi: 10.1093/eurheartj/ehp368
[2] Su L, Wang S, Wu S, et al. Long-term safety and feasibility of left bundle branch pacing in a large single-center study[J]. Circ Arrhythm Electrophysiol, 2021, 14(2): e009261. doi: 10.1161/CIRCEP.120.009261
[3] Huang W, Wu S, Vijayaraman P, et al. Cardiac resynchronization therapy in patients with nonischemic cardiomyopathy using left bundle branch pacing[J]. JACC Clin Electrophysiol, 2020, 6(7): 849-858. doi: 10.1016/j.jacep.2020.04.011
[4] 中华医学会心电生理和起搏分会, 中国医师协会心律学专业委员会. 希氏-浦肯野系统起搏中国专家共识[J]. 中华心律失常学杂志, 2021, 25(1): 10-36.
[5] Writing Committee Members. ACC/AHA Joint Committee Members. 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure[J]. J Card Fail, 2022, 28(5): e1-e167. doi: 10.1016/j.cardfail.2022.02.010
[6] Savarese G, Stolfo D, Sinagra G, et al. Heart failure with mid-range or mildly reduced ejection fraction[J]. Nat Rev Cardiol, 2022, 19(2): 100-116. doi: 10.1038/s41569-021-00605-5
[7] 中华医学会心血管病学分会, 中国医师协会心血管内科医师分会, 中国医师协会心力衰竭专业委员会, 等. 中国心力衰竭诊断和治疗指南2024[J]. 中华心血管病杂志, 2024, 52(3): 235-275. doi: 10.3760/cma.j.cn112148-20231101-00405
[8] Witt CM, Wu G, Yang D, et al. Outcomes with left bundle branch block and mildly to moderately reduced left ventricular function[J]. JACC Heart Fail, 2016, 4(11): 897-903. doi: 10.1016/j.jchf.2016.07.002
[9] Sharma S, Barot HV, Schwartzman AD, et al. Risk and predictors of dyssynchrony cardiomyopathy in left bundle branch block with preserved left ventricular ejection fraction[J]. Clin Cardiol, 2020, 43(12): 1494-1500. doi: 10.1002/clc.23467
[10] Ponnusamy SS, Vijayaraman P. Left bundle branch block-induced cardiomyopathy: insights from left bundle branch pacing[J]. JACC Clin Electrophysiol, 2021 7(9): 1155-1165. doi: 10.1016/j.jacep.2021.02.004
[11] Strauss DG, Selvester RH, Wagner GS. Defining left bundle branch block in the era of cardiac resynchronization therapy[J]. Am J Cardiol, 2011, 107(6): 927-934. doi: 10.1016/j.amjcard.2010.11.010
[12] Huang W, Chen X, Su L, et al. A beginner's guide to permanent left bundle branch pacing[J]. Heart Rhythm, 2019, 16(12): 1791-1796. doi: 10.1016/j.hrthm.2019.06.016
[13] Wu S, Chen X, Wang S, et al. Evaluation of the criteria to distinguish left bundle branch pacing from left ventricular septal pacing[J]. JACC Clin Electrophysiol, 2021, 7(9): 1166-1177. doi: 10.1016/j.jacep.2021.02.018
[14] Ghio S, Constantin C, Klersy C, et al. Interventricular and intraventricular dyssynchrony are common in heart failure patients, regardless of QRS duration[J]. Eur Heart J, 2004, 25(7): 571-578. doi: 10.1016/j.ehj.2003.09.030
[15] Wang Y, Zhu H, Hou X, et al. Randomized trial of left bundle branch vs biventricular pacing for cardiac resynchronization therapy[J]. J Am Coll Cardiol, 2022, 80(13): 1205-1216. doi: 10.1016/j.jacc.2022.07.019
[16] Pan YW, Zhou X, Yu C, et al. Clinical features and outcomes of long-term lead performance by left bundle branch pacing[J]. Int Heart J, 2024, 65(5): 800-807. doi: 10.1536/ihj.24-038
[17] Zeng J, He C, Zou F, et al. Early left bundle branch pacing in heart failure with mildly reduced ejection fraction and left bundle branch block[J]. Heart Rhythm, 2023, 20(10): 1436-1444. doi: 10.1016/j.hrthm.2023.07.063
[18] 姚云婕, 李柯蓓, 盛宇峰, 等. 比较左束支区域起搏与右室间隔部起搏对三尖瓣反流的影响[J]. 临床心血管病杂志, 2024, 40(2): 150-154. doi: 10.13201/j.issn.1001-1439.2024.02.012
[19] Rijks JHJ, Heckman L, Westra S, et al. Assessment of ventricular electrical heterogeneity in left bundle branch pacing and left ventricular septal pacing by using various electrophysiological methods[J]. J Cardiovasc Electrophysiol, 2024, 35(12): 2282-2292. doi: 10.1111/jce.16435
-

计量
- 文章访问数: 24
- 施引文献: 0



 下载:
下载: