The application value of caFFR in non-target vessel lesions in patients with ST-segment elevation myocardial infarction
-
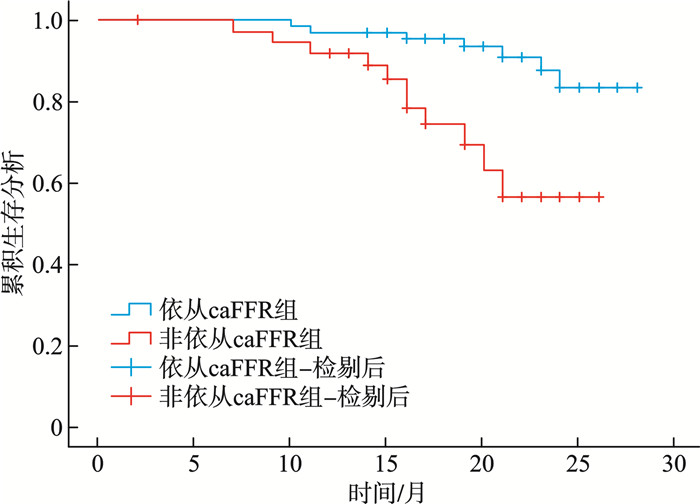
摘要: 目的 探讨冠状动脉造影衍生的血流储备分数(caFFR)在急性ST段抬高型心肌梗死(STEMI)非靶血管病变干预中的应用价值。 方法 回顾性纳入急性STEMI伴多支病变患者110例,测定非靶血管病变caFFR值,将患者分为缺血组(caFFR≤0.8,64例)和非缺血组(caFFR>0.8,46例)。其中,缺血组行PCI 38例,未行PCI 26例;非缺血组行PCI 12例,未行PCI 34例。将缺血组行PCI和非缺血组未行PCI的患者纳入依从caFFR组(72例),缺血组未行PCI和非缺血组行PCI的患者纳入非依从caFFR组(38例)。比较各组临床资料及预后差异。使用logistic回归分析筛选非靶血管病变caFFR≤0.8的危险因素。使用Kaplan-Meier生存分析比较依从组与非依从组组间的预后差异。使用Cox比例风险模型分析预后的危险因素。 结果 多因素logistic回归分析显示,合并高血压(OR=3.406,95%CI:1.421~8.161,P=0.006)、糖尿病(OR=2.918,95%CI:1.059~8.045,P=0.038)是非靶血管病变caFFR≤0.8的危险因素。截至随访终点,缺血组行PCI患者的主要不良心血管事件(MACE)发生率显著低于未行PCI患者(7.9% vs.34.6%,P=0.018),非缺血组行PCI与未行PCI患者间的MACE发生率差异无统计学意义(16.6% vs.11.7%,P=0.644),依从caFFR组MACE发生率显著低于非依从caFFR组(9.7% vs.28.9%,P=0.010)。Cox回归分析显示,依从caFFR进行治疗显著降低MACE发生风险(HR=0.317,95%CI:0.120~0.838,P=0.021)。 结论 caFFR有助于在临床实践中制定合适的血运重建策略。
-
关键词:
- ST段抬高型心肌梗死 /
- 多支病变 /
- 冠状动脉造影衍生的血流储备分数 /
- 经皮冠状动脉介入治疗
Abstract: Objective To observe the application value of coronary angiography-derived fractional flow reserve(caFFR) in guiding treatment for non-target vessel lesions in patients with acute ST-segment elevation myocardial infarction(STEMI). Methods A total of 110 patients with acute STEMI and multivessel disease were included. The caFFR values of non-target vessel lesions were measured, and all patients were divided into the ischemic group(caFFR≤0.8, n=64) and the non-ischemic group(caFFR>0.8, n=46). In the ischemic group, 38 patients underwent PCI and 26 did not. In the non-ischemic group, 12 underwent PCI and 34 did not. Patients from the ischemic group who underwent PCI and those from the non-ischemic group who didn't undergo PCI were included in the caFFR-adherent group(n=72), while patients from the ischemic group who didn't undergo PCI and those from the non-ischemic group who underwent PCI were included in the non-adherent group(n=38). Clinical characteristics and outcomes were compared. Logistic regression analysis was used to identify risk factors associated with non-target vessel lesions with caFFR ≤0.8. Kaplan-Meier analysis was used to compare prognosis between the caFFR-adherent and non-adherent groups. The Cox proportional hazards model was used to identify risk factors for prognosis. Results Multivariate logistic regression revealed hypertension(OR=3.406, 95%CI: 1.421-8.161, P=0.006) and/or diabetes(OR=2.918, 95%CI: 1.059-8.045, P=0.038) as independent risk factors for caFFR ≤0.8. By the end of follow-up, the incidence of major adverse cardiovascular events(MACE) in the ischemia group was significantly lower among patients who underwent PCI compared to those who did not(7.9% vs. 34.6%, P=0.018), there was no statistically significant difference in MACE incidence was observed between PCI and non-PCI patients in the non-ischemia group(16.6% vs. 11.7%, P=0.644), the caFFR-adherent group demonstrated a significantly lower MACE incidence than the non-adherent caFFR group(9.7% vs. 28.9%, P=0.01). Cox regression analysis identified that adherence to caFFR-guided treatment significantly reduces the risk of MACE(HR=0.317, 95%CI: 0.120-0.838, P=0.021). Conclusion caFFR provides valuable long-term prognostic information and can help develop optimal revascularization strategies in clinical practice. -

-
表 1 非缺血组与缺血组基线特征
Table 1. Baseline characteristics of the non-ischemia group and the ischemia group
例(%), X±S, M(P25, P75) 项目 非缺血组(46例) 缺血组(64例) P 年龄/岁 60.7±9.39 62.5±9.25 0.318 性别 0.196 男 36(78.3) 56(87.5) 女 10(21.7) 8(12.5) BMI/(kg/m2) 24.73±1.90 24.48±2.13 0.514 吸烟史 23(50.0) 30(46.9) 0.746 饮酒史 16(34.8) 15(23.4) 0.192 高血压 12(26.1) 30(46.9) 0.027 糖尿病 7(15.2) 25(39.0) 0.007 高脂血症 8(17.4) 19(29.7) 0.139 心衰 10(21.7) 10(15.6) 0.412 心律失常 8(17.4) 15(23.4) 0.442 脑血管病 0 4(6.3) 0.110 慢性肺疾病 3(6.5) 1(1.6) 0.393 慢性肾脏病 2(4.3) 3(4.7) 0.933 CK-MB峰值/(U/L) 116.25(38.76) 86.15(35.40,148.25) 0.123 cTnT峰值/(ng/mL) 123 00.00(5 877.50,40 150.00) 9 345(2 858.50,26 050.00) 0.242 NT-proBNP峰值/(pg/mL) 1 250.00(400.50,2 399.00) 1 228.00(546.75,2 252.75) 0.884 白细胞/(×109/L) 9.91±2.85 10.27±3.33 0.556 血小板/(×109/L) 167.50(147.75,203.50) 159.00(136.50,202.75) 0.685 血红蛋白/(g/L) 157.50(143.50,172.25) 152.50(138.00,162.75) 0.229 LDL-C/(mmol/L) 2.59(2.09,3.22) 2.53(2.11,3.12) 0.916 HDL-C/(mmol/L) 0.99(0.89,1.13) 0.98(0.86,1.10) 0.394 载脂蛋白B/(g/L) 0.93(0.70,1.10) 0.85(0.74,1.05) 0.590 K+/(mmol/L) 3.95±0.38 3.97±0.37 0.798 尿酸/(μmol/L) 353.87±11.15 348.52±87.86 0.777 肌酐/(μmol/L) 70.85(61.13,83.50) 76.90(61.10,86.03) 0.194 eGFR/(mL/min/1.73 m2) 94.40(83.18,101.60) 92.05(78.43,99.85) 0.310 LVEF/% 43.72±6.76 47.17±8.19 0.021 表 2 caFFR≤0.8危险因素的logistic回归分析
Table 2. Logistic regression analysis of risk factors for caFFR ≤0.8
项目 单因素logistic回归分析 多因素logistic回归分析 OR 95%CI P OR 95%CI P 高血压 2.378 1.060~5.334 0.036 2.729 1.150~6.475 0.023 糖尿病 3.207 1.287~7.991 0.012 3.419 1.293~9.039 0.013 LVEF 1.059 1.005~1.117 0.032 1.042 0.984~1.103 0.156 表 3 非缺血组与缺血组MACE发生情况
Table 3. MACE in the non-ischemic group and the ischemic group
例(%) 组别 PCI+ PCI- χ2 P 缺血组(64例) 38例 26例 MACE 3(7.9) 9(34.6) 5.587 0.018 心源性死亡 0(0) 1(3.8) 0.406* 再发心绞痛 2(5.3) 7(26.9) 4.335 0.025 再发心肌梗死 0 4(15.4) 0.024* 缺血驱动血运重建 0 8(30.8) 0.002* 症状性心衰 3(7.9) 3(11.5) 0.003 0.680 新发心律失常 2(5.3) 2(7.7) < 0.001 1.000 消化道出血 1(2.6) 1(3.8) < 0.001 1.000 非缺血组(46例) 12例 34例 MACE 2(16.6) 4(11.7) < 0.001 0.644 心源性死亡 0 0 再发心绞痛 2(16.6) 3(8.8) 0.045 0.833 再发心肌梗死 0 0 缺血驱动血运重建 1(8.3) 0.261* 症状性心衰 1(8.3) 4(11.7) < 0.001 1.000 新发心律失常 2(16.6) 2(5.9) 0.296 0.586 消化道出血 1(8.3) 1(2.9) < 0.001 1.000 注:*Fisher确切概率检验。 表 4 依从caFFR组和非依从caFFR组MACE发生情况
Table 4. MACE in the caFFR-adherent group and the non-adherent group
项目 依从
caFFR组
(72例)非依从
caFFR组
(38例)χ2 P MACE 7(9.7) 11(28.9) 6.717 0.010 心源性死亡 0 1(2.6) 0.345* 再发心绞痛 5(6.9) 9(23.7) 4.597 0.032 再发心肌梗死 0 4(10.5) 0.013* 缺血驱动血运重建 0 9(23.7) < 0.001* 症状性心衰 7(9.7) 4(10.5) 0 1.000 新发心律失常 4(5.6) 4(10.5) 0.323 0.444 消化道出血 2(2.8) 2(5.3) 0.016 0.607 注:*Fisher确切概率检验。 表 5 MACE影响因素的Cox回归分析
Table 5. Cox regression analysis of risk factors for MACE
项目 Cox单因素分析 Cox多因素分析 HR 95%CI P HR 95%CI P 缺血组(64例) 年龄 1.020 0.960~1.084 0.524 性别 1.129 0.250~5.097 0.875 高血压 6.711 1.486~30.307 0.013 4.650 1.002~21.579 0.050 糖尿病 1.303 0.438~3.877 0.635 高脂血症 4.32 1.413~13.255 0.010 吸烟 2.923 0.899~9.500 0.075 PCI 0.243 0.075~0.789 0.019 0.238 0.063~0.892 0.033 非缺血组(46例) 年龄 1.076 0.979~1.183 0.130 性别 1.877 0.343~10.268 0.468 高血压 0.542 0.063~4.646 0.576 糖尿病 2.659 0.001~3.328 0.650 高脂血症 0.036 0.001~262.149 0.464 吸烟 0.923 0.186~4.577 0.922 PCI 1.601 0.293~8.747 0.587 整体(110例) 年龄 1.396 0.459~4.240 0.557 性别 1.037 0.983~1.093 0.180 高血压 2.737 1.022~6.803 0.045 1.543 0.531~4.488 0.426 糖尿病 5.161 1.935~13.767 0.001 4.816 1.776~13.056 0.002 高脂血症 2.628 1.037~6.660 0.042 1.761 0.618~5.016 0.289 吸烟 2.254 0.846~6.005 0.104 PCI 0.429 0.153~1.203 0.108 依从caFFR 0.275 0.107~0.711 0.008 0.317 0.120~0.838 0.021 -
[1] Liu S, Li Y, Zeng X, et al. Burden of Cardiovascular Diseases in China, 1990-2016: Findings From the 2016 Global Burden of Disease Study[J]. JAMA Cardiol, 2019, 4(4): 342-352. doi: 10.1001/jamacardio.2019.0295
[2] Byrne RA, Rossello X, Coughlan JJ, et al. 2023 ESC Guidelines for the management of acutecoronarysyndromes[J]. Eur Heart J, 2023, 44(38): 37203826.
[3] 李云曌, 吴辉, 刘滴. 急性心肌梗死合并心源性休克诊治进展[J]. 临床心血管病杂志, 2020, 36(8): 692-695. doi: 10.13201/j.issn.1001-1439.2020.08.003
[4] Manuca RD, Covic AM, Brinza C, et al. Updated Strategies in Non-Culprit Stenosis Management of Multivessel Coronary Disease-A Contemporary Review[J]. Medicina(Kaunas), 2024, 60(2): 263.
[5] Alaswad K, Alqarqaz M. Complete Revascularization in STEMI: Why, How, and When?[J]. JACC Cardiovasc Interv, 2020, 13(13): 1583-1585. doi: 10.1016/j.jcin.2020.05.022
[6] 蒋俊, 史雷忠, 谢鹏程, 等. 外周血嗜酸粒细胞百分率联合高敏C反应蛋白对ST段抬高型心肌梗死患者PCI术后院内主要不良心脏事件的预测价值[J]. 临床急诊杂志, 2020, 21(12): 954-959.
[7] Prati F, Romagnoli E, Gatto L, et al. Relationship between coronary plaque morphology of the left anterior descending artery and 12 months clinical outcome: the CLIMA study[J]. Eur Heart J, 2020, 41(3): 383-391. doi: 10.1093/eurheartj/ehz520
[8] Lee SH, Hong D, Shin D, et al. QFR Assessment and Prognosis After Nonculprit PCI in Patients With Acute Myocardial Infarction[J]. JACC Cardiovasc Interv, 2023, 16(19): 2365-2379. doi: 10.1016/j.jcin.2023.08.032
[9] Li J, Gong Y, Wang W, et al. Accuracy of computational pressure-fluid dynamics applied to coronary angiography to derive fractional flow reserve: FLASH FFR[J]. Cardiovasc Res, 2020, 116(7): 1349-1356. doi: 10.1093/cvr/cvz289
[10] Caullery B, Riou L, Barone-Rochette G. Coronary Angiography Upgraded by Imaging Post-Processing: Present and Future Directions[J]. Diagnostics(Basel), 2023, 13(11): 1978.
[11] Mehta SR, Wood DA, Storey RF, et al. Complete Revascularization with Multivessel PCI for Myocardial Infarction[J]. N Engl J Med, 2019, 381(15): 1411-1421. doi: 10.1056/NEJMoa1907775
[12] Erlinge D, Maehara A, Ben-Yehuda O, et al. Identification of vulnerable plaques and patients by intracoronary near-infrared spectroscopy and ultrasound(PROSPECT Ⅱ): a prospective natural history study[J]. Lancet, 2021, 397(10278): 985-995. doi: 10.1016/S0140-6736(21)00249-X
[13] Fabris E, Berta B, Hommels T, et al. Long-term outcomes of patients with normal fractional flow reserve and thin-cap fibroatheroma[J]. EuroIntervention, 2023, 18(13): e1099-e1107. doi: 10.4244/EIJ-D-22-00306
[14] Van Belle E, Rioufol G, Pouillot C, et al. Outcome impact of coronary revascularization strategy reclassification with fractional flow reserve at time of diagnostic angiography: insights from a large French multicenter fractional flow reserve registry[J]. Circulation, 2014, 129(2): 173-185. doi: 10.1161/CIRCULATIONAHA.113.006646
[15] Xu B, Tu S, Song L, et al. Angiographic quantitative flow ratio-guided coronary intervention(FAVOR Ⅲ China): a multicentre, randomised, sham-controlled trial[J]. Lancet, 2021, 398(10317): 2149-2159. doi: 10.1016/S0140-6736(21)02248-0
[16] Ai H, Zheng N, Li L, et al. Agreement of Angiography-Derived and Wire-Based Fractional Flow Reserves in Percutaneous Coronary Intervention[J]. Front Cardiovasc Med, 2021, 8: 654392. doi: 10.3389/fcvm.2021.654392
[17] Zhang Z, Xie M, Dai X, et al. The prognostic value and economic benefits of coronary angiography-derived fractional flow reserve-guided strategy in patients with coronary artery disease[J]. Heliyon, 2023, 9(6): e17464. doi: 10.1016/j.heliyon.2023.e17464
[18] Liu J, Zhang K, Wang X, et al. Complete revascularization based on angiography derived fractional flow reserve versus incomplete revascularization in patients with ST-segment elevation myocardial infarction[J]. Cardiol J, 2024, 31(2): 226-234. doi: 10.5603/cj.92762
[19] 韩超, 张弘, 张慧, 等. 冠状动脉微循环阻力评估急性ST段抬高型心肌梗死PCI患者预后的临床研究[J]. 临床心血管病杂志, 2024, 40(4): 317-323. doi: 10.13201/j.issn.1001-1439.2024.04.013
[20] Zheng W, Guo Q, Guo R, et al. Predicting left ventricular remodeling post-MI through coronary physiological measurements based on computational fluid dynamics[J]. iScience, 2024, 27(4): 109513. doi: 10.1016/j.isci.2024.109513
-

计量
- 文章访问数: 17
- 施引文献: 0



 下载:
下载: