Application of critical care ultrasound in extracorporeal membrane oxygenation and cardiopulmonary
-
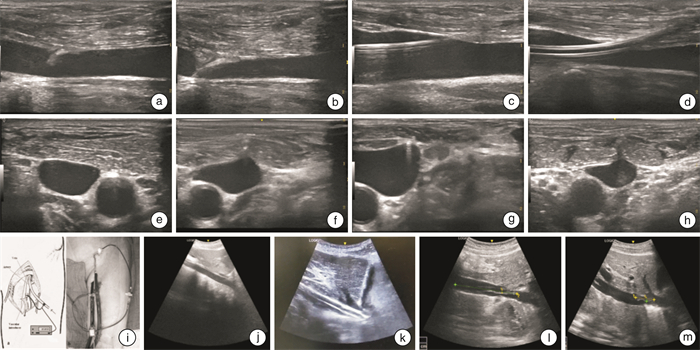
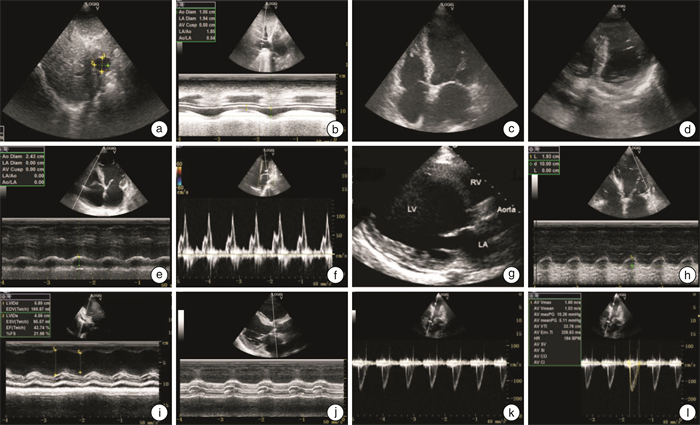
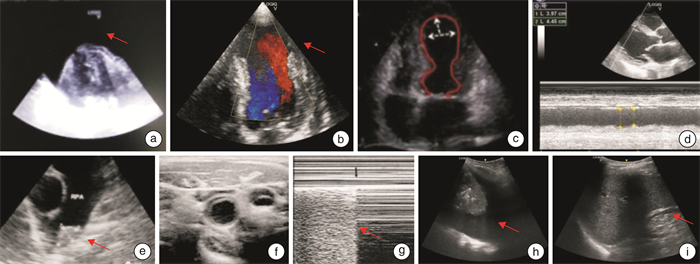
摘要: 体外膜肺氧合(ECMO)越来越多地应用于成人严重呼吸或心力衰竭的支持,重症超声在ECMO全程管理中起着重要作用。本文就重症超声在ECMO运行期间心肺支持可视化和精细化管理中的应用加以综述。Abstract: Extracorporeal membrane oxygenation(ECMO) is increasingly used to support severe respiratory and heart failure in adults, and critical care ultrasound plays an important role in the whole process management of ECMO. This article reviews the visualization and fine management of cardiopulmonary support by critical care ultrasound during ECMO operation.
-

-
[1] Tsangaris A, Alexy T, Kalra R, et al. Overview of Veno-Arterial Extracorporeal Membrane Oxygenation(VA-ECMO)Support for the Management of Cardiogenic Shock[J]. Front Cardiovasc Med, 2021, 8: 686558. doi: 10.3389/fcvm.2021.686558
[2] Kalra R, Bartos JA, Kosmopoulos M, et al. Echocardiographic evaluation of cardiac recovery after refractory out-of-hospital cardiac arrest[J]. Resuscitation, 2020, 154: 38-46. doi: 10.1016/j.resuscitation.2020.06.037
[3] 刘大为, 王小亭. 重症超声[M]. 北京, 人民卫生出版社, 2018: 49-97.
[4] Thangaraj PR. The physiological basis of clinical decision-making in venoarterial extracorporeal life support[J]. Indian J Thorac Cardiovasc Surg, 2021, 37(Suppl 2): 210-220.
[5] Ketelaars R, Reijnders G, van Geffen GJ, et al. ABCDE of prehospital ultrasonography: a narrative review[J]. Crit Ultrasound J, 2018, 10(1): 17. doi: 10.1186/s13089-018-0099-y
[6] 陈瑞珍. 病毒性心肌炎后扩张型心肌病的临床认知[J]. 临床心血管病杂志, 2022, 38(2): 85-87. doi: 10.13201/j.issn.1001-1439.2022.02.001 https://lcxxg.whuhzzs.com/article/doi/10.13201/j.issn.1001-1439.2022.02.001
[7] Ramadan A, Abdallah T, Abdelsalam H, et al. Accuracy of echocardiography and ultrasound protocol to identify shock etiology in emergency department[J]. BMC Emerg Med, 2022, 22(1): 117. doi: 10.1186/s12873-022-00678-6
[8] Harnisch LO, Moerer O. Contraindications to the Initiation of Veno-Venous ECMO for Severe Acute Respiratory Failure in Adults: A Systematic Review and Practical Approach Based on the Current Literature[J]. Membranes(Basel), 2021, 11(8).
[9] Ma Z, Gai J, Sun Y, et al. Measuring the ratio of femoral vein diameter to femoral artery diameter by ultrasound to estimate volume status[J]. BMC Cardiovasc Disord, 2021, 21(1): 506. doi: 10.1186/s12872-021-02309-7
[10] Cairo SB, Arbuthnot M, Boomer L, et al. Comparing Percutaneous to Open Access for Extracorporeal Membrane Oxygenation in Pediatric Respiratory Failure[J]. Pediatr Crit Care Med, 2018, 19(10): 981-991. doi: 10.1097/PCC.0000000000001691
[11] Bonicolini E, Martucci G, Simons J, et al. Limb ischemia in peripheral veno-arterial extracorporeal membrane oxygenation: a narrative review of incidence, prevention, monitoring, and treatment[J]. Crit Care, 2019, 23(1): 266. doi: 10.1186/s13054-019-2541-3
[12] Gottlieb M, Holladay D, Peksa GD. Comparison of Short-vs Long-axis Technique for Ultrasound-guided Peripheral Line Placement: A Systematic Review and Meta-analysis[J]. Cureus, 2018, 10(5): e2718.
[13] Crivellari M, Pappalardo F. Femoro-jugular cannulation in veno-venous extracorporeal membrane oxygenation PRO/CON[J]. J Thorac Dis, 2018, 10(Suppl 5): S613-S615.
[14] Jayaraman AL, Cormican D, Shah P, et al. Cannulation strategies in adult veno-arterial and veno-venous extracorporeal membrane oxygenation: Techniques, limitations, and special considerations[J]. Ann Card Anaesth, 2017, 20(Supplement): S11-S18.
[15] Pavlushkov E, Berman M, Valchanov K. Cannulation techniques for extracorporeal life support[J]. Ann Transl Med, 2017, 5(4): 70. doi: 10.21037/atm.2016.11.47
[16] Patton-Rivera K, Beck J, Fung K, et al. Using near-infrared reflectance spectroscopy(NIRS)to assess distal-limb perfusion on venoarterial(V-A)extracorporeal membrane oxygenation(ECMO)patients with femoral cannulation[J]. Perfusion, 2018, 33(8): 618-623. doi: 10.1177/0267659118777670
[17] Argaiz ER, Koratala A, Reisinger N. Comprehensive Assessment of Fluid Status by Point-of-Care Ultrasonography[J]. Kidney360, 2021, 2(8): 1326-1338. doi: 10.34067/KID.0006482020
[18] Staudacher DL, Gold W, Biever PM, et al. Early fluid resuscitation and volume therapy in venoarterial extracorporeal membrane oxygenation[J]. J Crit Care, 2017, 37: 130-135. doi: 10.1016/j.jcrc.2016.09.017
[19] Monnet X, Shi R, Teboul JL. Prediction of fluid responsiveness. What's new?[J]. Ann Intensive Care, 2022, 12(1): 46. doi: 10.1186/s13613-022-01022-8
[20] Pellicori P, Platz E, Dauw J, et al. Ultrasound imaging of congestion in heart failure: examinations beyond the heart[J]. Eur J Heart Fail, 2021, 23(5): 703-712. doi: 10.1002/ejhf.2032
[21] Huang KC, Lin LY, Chen YS, et al. Three-Dimensional Echocardiography-Derived Right Ventricular Ejection Fraction Correlates with Success of Decannulation and Prognosis in Patients Stabilized by Venoarterial Extracorporeal Life Support[J]. J Am Soc Echocardiogr, 2018, 31(2): 169-179. doi: 10.1016/j.echo.2017.09.004
[22] Lang RM, Bierig M, Devereux RB, et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography's Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology[J]. J Am Soc Echocardiogr, 2005, 18(12): 1440-1463. doi: 10.1016/j.echo.2005.10.005
[23] Nikitin NP, Witte KK, Thackray SD, et al. Longitudinal ventricular function: normal values of atrioventricular annular and myocardial velocities measured with quantitative two-dimensional color Doppler tissue imaging[J]. J Am Soc Echocardiogr, 2003, 16(9): 906-921. doi: 10.1016/S0894-7317(03)00279-7
[24] 严霜霜, 熊峰, 张丽娟, 等. 二维斑点追踪技术评价左束支区域起搏早期右心室收缩功能及同步性[J]. 临床心血管病杂志, 2022, 38(7): 561-565. doi: 10.13201/j.issn.1001-1439.2022.07.009 https://lcxxg.whuhzzs.com/article/doi/10.13201/j.issn.1001-1439.2022.07.009
[25] Chao G, Zheng C, Meng D, et al. Tei index: The earliest detectable cardiac structural and functional abnormality detectable in Hb Bart's foetal edema. [J]. Int J Cardiol, 2009, 134(3): e150-e154. doi: 10.1016/j.ijcard.2008.12.182
[26] Keranov S, Haen S, Vietheer J, et al. Application and Validation of the Tricuspid Annular Plane Systolic Excursion/Systolic Pulmonary Artery Pressure Ratio in Patients with Ischemic and Non-Ischemic Cardiomyopathy[J]. Diagnostics, 2021, 11(12): 2188. doi: 10.3390/diagnostics11122188
[27] Crotti S, Bottino N, Spinelli E. Spontaneous breathing during veno-venous extracorporeal membrane oxygenation[J]. J Thorac Dis, 2018, 10(5): S661-S669.
[28] Jentzer JC, Anavekar NS, Mankad SV, et al. Changes in left ventricular systolic and diastolic function on serial echocardiography after out-of-hospital cardiac arrest[J]. Resuscitation, 2018, 126: 1-6. doi: 10.1016/j.resuscitation.2018.01.050
[29] Shah A, Dave S, Goerlich CE, et al. Hybrid and parallel extracorporeal membrane oxygenation circuits[J]. JTCVS Tech, 2021, 8: 77-85. doi: 10.1016/j.xjtc.2021.02.024
[30] Jenkins S, Alabed S, Swift A, et al. Diagnostic accuracy of handheld cardiac ultrasound device for assessment of left ventricular structure and function: systematic review and meta-analysis[J]. Heart, 2021, 107(22): 1826-1834. doi: 10.1136/heartjnl-2021-319561
[31] Yin W, Li Y, Wang S, et al. The PIEPEAR Workflow: A Critical Care Ultrasound Based 7-Step Approach as a Standard Procedure to Manage Patients with Acute Cardiorespiratory Compromise, with Two Example Cases Presented[J]. Biomed Res Int, 2018: 4687346.
[32] 薛婷, 张鹏英, 陈允安, 等. 超声心动图研究新视角: 无创左室压力-应变环[J]. 临床心血管病杂志, 2021, 37(6): 507-511. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXB202106003.htm
[33] Weber C, Deppe AC, Sabashnikov A, et al. Left ventricular thrombus formation in patients undergoing femoral veno-arterial extracorporeal membrane oxygenation[J]. Perfusion, 2018, 33(4): 283-288. doi: 10.1177/0267659117745369
[34] Ricarte Bratti JP, Cavayas YA, Noly PE, et al. Modalities of Left Ventricle Decompression during VA-ECMO Therapy[J]. Membranes(Basel), 2021, 11(3): 209.
[35] Di Vece D, Silverio A, Bellino M, et al. Dynamic Left Intraventricular Obstruction Phenotype in Takotsubo Syndrome[J]. J Clin Med, 2021, 10(15): 3235. doi: 10.3390/jcm10153235
[36] Grune J, Beyhoff N, Hegemann N, et al. From bedside to bench: lung ultrasound for the assessment of pulmonary edema in animal models[J]. Cell Tissue Res, 2020, 380(2): 379-392. doi: 10.1007/s00441-020-03172-2
[37] Ortuno S, Delmas C, Diehl JL, et al. Weaning from veno-arterial extra-corporeal membrane oxygenation: which strategy to use?[J]. Ann Cardiothorac Surg, 2019, 8(1): E1-E8. doi: 10.21037/acs.2018.08.05
[38] Sawada K, Kawakami S, Murata S, et al. Predicting Parameters for Successful Weaning from Veno-Arterial Extracorporeal Membrane Oxygenation in Cardiogenic Shock[J]. ESC Heart Fail, 2021, 8(1): 471-480. doi: 10.1002/ehf2.13097
-




 下载:
下载: