Correlation between glycosylated hemoglobin variability and in-stent restenosis after PCI in patients with type 2 diabetes
-
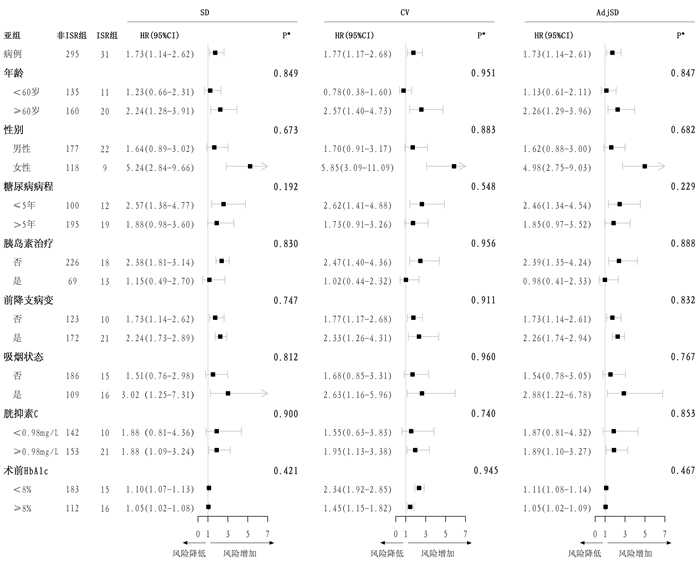
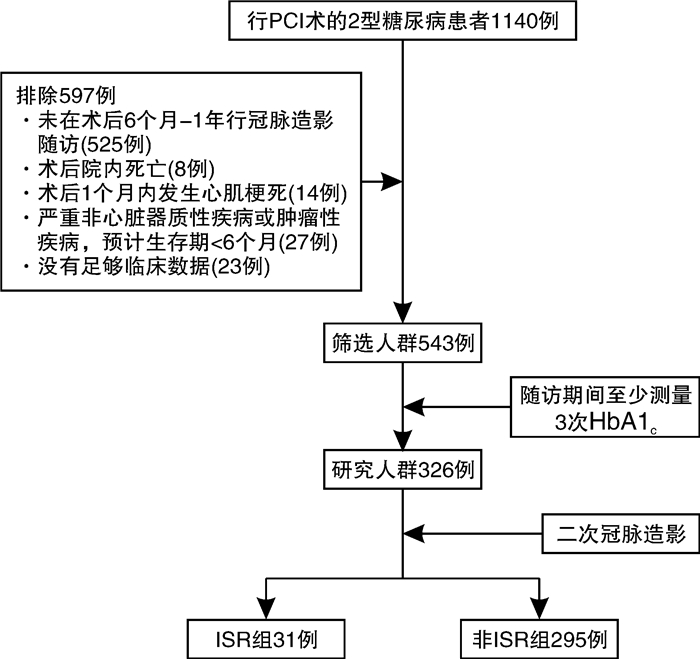
摘要: 目的 探讨2型糖尿病患者糖化血红蛋白(HbA1c)变异性与经皮冠状动脉(冠脉)介入治疗(PCI)术后支架内再狭窄(ISR)的关系。方法 连续纳入2017年9月—2021年3月在郑州大学第一附属医院心内科行PCI术的326例2型糖尿病患者。根据术后6个月至1年随访的冠脉造影结果分为ISR组和非ISR组。HbA1c变异性以HbA1c测量值的标准差、变异系数和校正后的标准差表示。建立多因素Cox回归模型分析HbA1c变异性与ISR的关系。结果 基线分析表明,两组在胱抑素C、术前HbA1c、平均HbA1c、钙通道阻滞剂、口服降糖药、胰岛素应用、饮酒状态、脑卒中史、支架数量等方面存在差异(均P < 0.05)。在多因素分析中,依次校正多个混杂因素后发现高HbA1c变异性与发生ISR的风险增加独立相关,HR(每1-SD增加)分别为1.73(95%CI:1.14~2.62)、1.77(95%CI:1.17~2.68)、1.73(95%CI:1.14~2.61)。结论 高HbA1c变异性与2型糖尿病患者PCI术后发生ISR的风险增加独立相关。
-
关键词:
- 2型糖尿病 /
- 糖化血红蛋白变异性 /
- 支架内再狭窄 /
- 经皮冠状动脉介入治疗
Abstract: Objective To investigate the association between glycated hemoglobin(HbA1c) variability and in-stent restenosis(ISR) after percutaneous coronary intervention(PCI) in patients with type 2 diabetes.Methods A total of 326 patients with type 2 diabetes who underwent PCI were continuously screened from September 2017 to March 2021, in the Department of Cardiology, the First Affiliated Hospital of Zhengzhou University. They were divided into ISR group and non-ISR group based on results of follow-up 6 months to 1 year after coronary angiography. Multivariable Cox models were established to analyze the association between ISR and HbA1cvariability, expressed as standard deviation, coefficient of variation, and adjusted-standard deviation.Results Baseline analysis showed differences in cystatin C, preoperative HbA1c, mean HbA1c, calcium channel blockers, oral hypoglycemic agent, insulin use, drinking status, history of stroke, and numbers of stents. Multivariate analysis showed that increased HbA1cvariability was independently associated with higher risk of ISR. HR(per 1-SD) was 1.73(95%CI: 1.14-2.62), 1.77(95%CI: 1.17-2.68), 1.73(95%CI: 1.14-2.61).Conclusion Increased HbA1cvariability is independently associated with higher risk of ISR after coronary stent implantation in type 2 diabetic patients. -

-
表 1 基线特征
Table 1. Baseline characteristics
例(%), X±S, M(P25, P75) 项目 非ISR组(295例) ISR组(31例) P值 女性 118(40.0) 9(29.0) 0.318 年龄/岁 59.93±9.12 61.94±9.03 0.244 收缩压/mmHg 133.00(123.00,145.00) 133.00(125.50,140.50) 0.877 舒张压/mmHg 78.00(71.00,86.00) 84.00(71.00,86.50) 0.530 糖尿病病程/年 8.00(4.00,14.00) 9.00(2.00,15.00) 0.944 LVEF/% 60.00(54.00,63.00) 61.00(56.50,63.00) 0.991 LVEDV/mm 47.00(44.00,50.00) 47.00(45.00,53.00) 0.234 术前HbA1c/% 7.60(6.65,8.55) 8.00(7.40,8.80) 0.051 末次HbA1c/% 7.70(6.90,8.10) 7.70(7.00,8.05) 0.517 平均HbA1c/% 7.68(6.93,8.25) 7.83(7.37,8.38) 0.183 血红蛋白/(g·L-1) 128.18±16.38 132.92±15.67 0.124 中性粒细胞绝对值/(×109·L-1) 4.45(3.42,5.87) 4.50(3.14,5.04) 0.314 TC/(mmol·L-1) 3.74(3.06,4.60) 3.46(2.91,4.09) 0.146 TG/(mmol·L-1) 1.87(1.35,2.68) 1.41(1.08,2.26) 0.065 HDL-C/(mmol·L-1) 0.94(0.79,1.12) 0.96(0.78,1.10) 0.683 LDL-C/(mmol·L-1) 2.12(1.60,2.79) 2.06(1.73,2.36) 0.538 谷丙转氨酶/(U·L-1) 23.00(16.00,35.50) 21.00(17.00,26.50) 0.272 SCr/(μmol·L-1) 69.00(58.00,84.00) 69.00(61.50,83.50) 0.764 尿酸/(μmol·L-1) 293.00(238.00,350.50) 286.00(241.00,354.00) 0.991 胱抑素C/(mg·L-1) 0.98(0.84,1.13) 1.05(0.94,1.23) 0.044 NT-proBNP/(pg·mL-1) 492.00(157.52,1175.50) 705.00(189.50,1209.00) 0.502 阿司匹林 291(98.6) 30(96.8) 0.395 P2Y12受体拮抗剂 283(95.9) 29(93.5) 0.631 β受体阻滞剂 243(82.4) 28(90.3) 0.383 ACEI 86(29.3) 6(19.4) 0.340 ARB 101(34.2) 13(41.9) 0.511 CCB 114(38.6) 1(3.2) <0.001 利尿剂 66(22.4) 9(29.0) 0.539 他汀 292(99.0) 30(96.8) 0.331 OHA 269(91.2) 24(77.4) 0.025 胰岛素 69(23.4) 13(41.9) 0.041 OHA联合胰岛素 33(11.2) 5(16.1) 0.383 高血压 181(61.4) 17(54.8) 0.608 脑卒中史 139(47.1) 3(9.7) < 0.001 吸烟状态 0.146 从未吸烟 158(53.6) 11(35.5) 目前吸烟 109(36.9) 16(51.6) 已戒烟 28(9.5) 4(12.9) 饮酒状态* 0.008 从未饮酒 170(57.6) 14(45.2) 目前饮酒 93(31.5) 7(22.6) 已戒酒 32(10.8) 10(32.3) 注:1 mmHg=0.133 kPa;ACEI:血管紧张素转化酶抑制剂;ARB:血管紧张素Ⅱ受体拮抗剂;CCB:钙通道阻滞剂;OHA:口服降糖药物;*:进一步两两比较,从未饮酒与目前饮酒P=0.99,从未饮酒与已戒酒P=0.005,目前饮酒与已戒酒P=0.009。 表 2 手术特征
Table 2. Procedural characteristics
例(%), M(P25, P75) 项目 非ISR组(295例) ISR组(31例) P值 支架数量/个 2.00(1.00,3.00) 3.00(2.00,4.00) 0.002 支架直径/mm 3.00(2.75,3.25) 2.88(2.72,3.12) 0.384 支架长度/mm 25.33(21.50,29.25) 26.00(22.08,29.80) 0.595 多支病变 91(30.8) 11(35.5) 0.744 左主干病变 12(4.1) 2(6.5) 0.631 前降支病变 172(58.3) 21(67.7) 0.409 回旋支病变 93(31.5) 9(29.0) 0.935 右冠病变 116(39.3) 10(32.3) 0.566 表 3 HbA1c变异性对发生ISR的单因素和多因素Cox回归分析
Table 3. Cox regression analysis
项目 HR(95%CI) P C-index 单因素分析 SD 1.58(1.23~2.04) < 0.001 — CV 1.47(1.12~1.93) 0.006 — AdjSD 1.56(1.21~2.03) 0.001 — 模型1 SD 1.61(1.25~2.07) < 0.001 0.678 CV 1.50(1.13~1.99) 0.005 0.672 AdjSD 1.58(1.23~2.06) < 0.001 0.676 模型2 SD 1.97(1.42~2.74) < 0.001 0.907 CV 1.99(1.37~2.88) < 0.001 0.910 AdjSD 1.97(1.41~2.74) < 0.001 0.908 模型3 SD 1.83(1.25~2.67) 0.002 0.907 CV 1.87(1.27~2.74) 0.001 0.910 AdjSD 1.81(1.24~2.65) 0.002 0.907 模型4 SD 1.73(1.14~2.62) 0.009 0.912 CV 1.77(1.17~2.68) 0.007 0.912 AdjSD 1.73(1.14~2.61) 0.010 0.911 注:多因素分析包括以下4个模型:模型1校正了性别和年龄;模型2在模型1的基础上校正了CCB、OHA、胰岛素应用、脑卒中史、饮酒、吸烟状态、收缩压、舒张压、TG、LDL-C、SCr、胱抑素C、支架数量;模型3进一步校正了术前HbA1c;模型4进一步校正了平均HbA1c。 表 4 不同HbA1c变异性水平对发生ISR风险的影响
Table 4. The impact of different HbA1cvariability levels on ISR
分组 HR(95%CI) P 校正的HR(95%CI) P 低SD 参考 - 参考 - 高SD 2.43(1.20~4.92) 0.014 2.68(1.07~6.70) 0.035 低CV 参考 - 参考 - 高CV 3.21(1.56~6.62) 0.002 4.87(1.94~12.25) 0.001 低AdjSD 参考 - 参考 - 高AdjSD 2.41(1.19~4.88) 0.015 3.23(1.29~8.07) 0.012 -
[1] Liu Y, Xu C, Fu P, et al. Family history of myocardial infarction as a strong independent predictor of in-stent restenosis in the era of drug eluting stents[J]. Int J Cardiol, 2015, 179: 55-57. doi: 10.1016/j.ijcard.2014.10.082
[2] Nusca A, Tuccinardi D, Albano M, et al. Glycemic variability in the development of cardiovascular complications in diabetes[J]. Diabetes Metab Res Rev, 2018, 34(8): e3047. doi: 10.1002/dmrr.3047
[3] Funamizu T, Iwata H, Nishida Y, et al. Increased risk of cardiovascular mortality by strict glycemic control(pre-procedural HbA1c < 6.5%)in Japanese medically-treated diabetic patients following percutaneous coronary intervention: a 10-year follow-up study[J]. Cardiovasc Diabetol, 2020, 19(1): 21. doi: 10.1186/s12933-020-00996-8
[4] Beck RW, Connor CG, Mullen DM, et al. The Fallacy of Average: How Using HbA1c Alone to Assess Glycemic Control Can Be Misleading[J]. Diabetes Care, 2017, 40(8): 994-999. doi: 10.2337/dc17-0636
[5] Kilpatrick ES. The rise and fall of HbA(1c)as a risk marker for diabetes complications[J]. Diabetologia, 2012, 55(8): 2089-2091. doi: 10.1007/s00125-012-2610-5
[6] Škrha J, Šoupal J, Škrha J Jr, et al. Glucose variability, HbA1c and microvascular complications[J]. Rev Endocr Metab Disord, 2016, 17(1): 103-110. doi: 10.1007/s11154-016-9347-2
[7] Li S, Tang X, Luo Y, et al. Impact of long-term glucose variability on coronary atherosclerosis progression in patients with type 2 diabetes: a 2.3 year follow-up study[J]. Cardiovasc Diabetol, 2020, 19(1): 146. doi: 10.1186/s12933-020-01126-0
[8] Alraies MC, Darmoch F, Tummala R, et al. Diagnosis and management challenges of in-stent restenosis in coronary arteries[J]. World J Cardiol, 2017, 9(8): 640-651. doi: 10.4330/wjc.v9.i8.640
[9] Orsi E, Solini A, Bonora E, et al. Haemoglobin A1c variability is a strong, independent predictor of all-cause mortality in patients with type 2 diabetes[J]. Diabetes Obes Metab, 2018, 20(8): 1885-1893. doi: 10.1111/dom.13306
[10] American Diabetes Association. 6. Glycemic targets: standards of medical care in diabetes-2018[J]. Diabetes Care, 2018, 41(Suppl 1): S55-S64.
[11] Yang CD, Shen Y, Lu L, et al. Visit-to-visit HbA1c variability is associated with in-stent restenosis in patients with type 2 diabetes after percutaneous coronary intervention[J]. Cardiovasc Diabetol, 2020, 19(1): 133. doi: 10.1186/s12933-020-01111-7
[12] Li S, Nemeth I, Donnelly L, et al. Visit-to-visit HbA1c variability is associated with cardiovascular disease and microvascular complications in patients with newly diagnosed type 2 diabetes[J]. Diabetes Care, 2020, 43(2): 426-432. doi: 10.2337/dc19-0823
[13] Zhou JJ, Schwenke DC, Bahn G, et al. Glycemic variation and cardiovascular risk in the veterans affairs diabetes trial[J]. Diabetes Care, 2018, 41(10): 2187-2194. doi: 10.2337/dc18-0548
[14] Lee EJ, Kim YJ, Kim TN, et al. A1c variability can predict coronary artery disease in patients with type 2 diabetes with mean a1c levels greater than 7[J]. Endocrinol Metab(Seoul), 2013, 28(2): 125-132. doi: 10.3803/EnM.2013.28.2.125
[15] Schisano B, Tripathi G, McGee K, et al. Glucose oscillations, more than constant high glucose, induce p53 activation and a metabolic memory in human endothelial cells[J]. Diabetologia, 2011, 54(5): 1219-1226. doi: 10.1007/s00125-011-2049-0
[16] 马雅楠, 刘德敏, 谷国强. 2型糖尿病与血管衰老研究进展[J]. 临床心血管病杂志, 2021, 37(9): 791-795. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXB202109003.htm
[17] Kitta Y, Nakamura T, Kodama Y, et al. Endothelial vasomotor dysfunction in the brachial artery is associated with late in-stent coronary restenosis[J]. J Am Coll Cardiol, 2005, 46(4): 648-655. doi: 10.1016/j.jacc.2005.04.055
[18] Thanyasiri P, Kathir K, Celermajer D S, et al. Endothelial dysfunction and restenosis following percutaneous coronary intervention[J]. Int J Cardiol, 2007, 119(3): 362-367. doi: 10.1016/j.ijcard.2006.08.015
[19] Reddy MA, Zhang E, Natarajan R. Epigenetic mechanisms in diabetic complications and metabolic memory[J]. Diabetologia, 2015, 58(3): 443-455. doi: 10.1007/s00125-014-3462-y
[20] Shen Y, Zhou J, Shi L, et al. Association between visit-to-visit HbA1c variability and the risk of cardiovascular disease in patients with type 2 diabetes[J]. Diabetes Obes Metab, 2021, 23(1): 125-135. doi: 10.1111/dom.14201
[21] Pieber TR, Marso SP, McGuire DK, et al. DEVOTE 3: temporal relationships between severe hypoglycaemia, cardiovascular outcomes and mortality[J]. Diabetologia, 2018, 61(1): 58-65. doi: 10.1007/s00125-017-4422-0
[22] Bonke FC, Donnachie E, Schneider A, et al. Association of the average rate of change in HbA1c with severe adverse events: a longitudinal evaluation of audit data from the Bavarian Disease Management Program for patients with type 2 diabetes mellitus[J]. Diabetologia, 2016, 59(2): 286-293. doi: 10.1007/s00125-015-3797-z
-




 下载:
下载: