Relationship between hemoglobin glycation index and coronary artery disease in patients with type 2 diabetes mellitus complicated and coronary heart disease
-
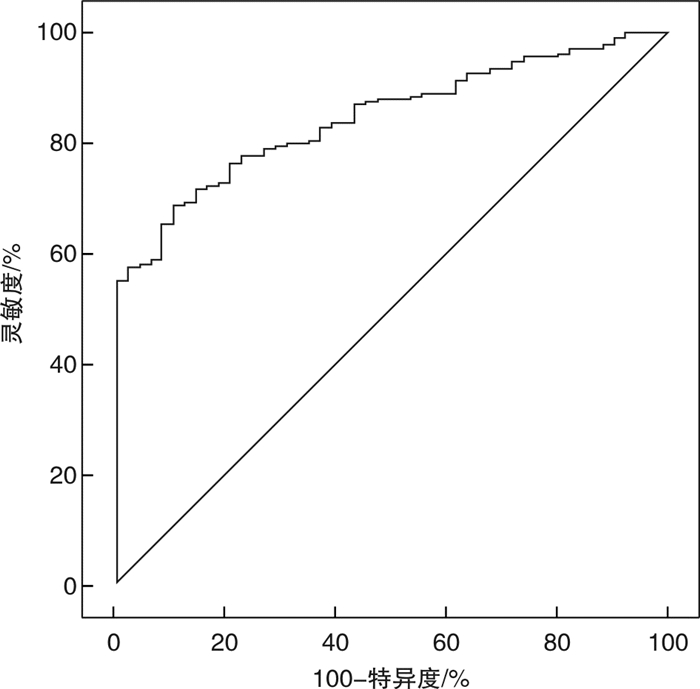
摘要: 目的 探讨糖化血红蛋白变异指数(HGI)与2型糖尿病(T2DM)合并冠心病(CHD)患者冠状动脉(冠脉)病变的相关性。方法 收集2020年6月—2021年7月在赣南医学院第一附属医院就诊的284例T2DM患者的临床资料,其中单纯T2DM组49例,T2DM合并CHD组235例,分析两组患者的社会人口学特征、烟酒嗜好以及血液生化指标的差异。采用多因素logistic回归分析影响T2DM合并CHD发生的危险因素,受试者操作特征曲线(ROC)分析HGI对T2DM合并CHD发生的诊断价值,并通过多元线性回归分析探讨HGI与Gensini评分的相关性。结果 T2DM+CHD组空腹血糖(FPG)、糖化血红蛋白(HbA1c)、餐后2 h血糖(2hPBG)、HGI、男性比例、吸烟率高于单纯T2DM组,而收缩压(SBP)、舒张压(DBP)、高密度脂蛋白(HDL-C)、载脂蛋白b、左室射血分数(LVEF)低于T2DM组,差异有统计学意义(P < 0.05);logistic回归分析显示,HGI升高为T2DM合并CHD发生的独立危险因素(OR=2.985,95%CI:1.506~5.915,P < 0.05)。ROC曲线示HGI预测T2DM合并CHD发生的曲线下面积为0.840,当HGI为-0.488%时,灵敏度为68.09%,特异度为89.80%,具有较好的诊断效能。相关性分析示,Gensini评分与HGI、TC、LDL-C、FBG、2hPBG、血肌酐(Scr)、HbA1c呈正相关,与SBP、DBP、HDL-C、LVEF、BMI呈负相关(P < 0.05)。多元线性回归分析示,即使校正混杂因素后,Gensini评分与HGI之间存在剂量-反应关系,Gensini评分随HGI水平升高而增加(P < 0.01)。结论 HGI是T2DM合并CHD患者冠脉病变的独立危险因素,且HGI水平越高,其冠脉狭窄程度越严重。
-
关键词:
- 糖化血红蛋白变异指数 /
- 2型糖尿病 /
- 冠心病 /
- Gensini评分
Abstract: Objective To investigate the relationship between hemoglobin glycation index(HGI) and coronary artery disease in patients with type 2 diabetes mellitus(T2DM) complicated with coronary heart disease(CHD).Methods The clinical data of 284 patients with T2DM were collected from June 2020 to July 2021 in the first affiliated Hospital of Gannan Medical College, including 49 patients in T2DM group and 235 patients in T2DM+CHD group. The differences of social demographic characteristics, smoking and drinking habits and blood biochemical indexes between the two groups were analyzed. Multivariate Logistic regression analysis was used to analyze the risk factors of T2DM complicated with CHD. The receiver operating characteristic curve(ROC) was used to analyze the diagnostic value of HGI in T2DM complicated with CHD. Multiple linear regression analysis was used to explore the correlation between HGI and Gensini score.Results Fasting blood glucose(FPG), glycosylated hemoglobin(HbA1c), 2-hour postprandial blood glucose(2hPBG), HGI, male proportion and smoking rate in T2DM+CHD group were higher than those in T2DM group, while systolic blood pressure(SBP), diastolic blood pressure(DBP), high density lipoprotein(HDL-C), apolipoprotein b and left ventricular ejection fraction(LVEF) in T2DM+CHD group were significantly lower than those in T2DM group(P < 0.05). Logistic regression analysis showed that the increase of HGI was an independent risk factor for the occurrence of T2DM complicated with CHD(OR=2.985, 95%CI: 1.506-5.915, P < 0.05). The ROC curve showed that the area under the curve in which HGI predicts the occurrence of T2DM combined with CHD was 0.840. When HGI was-0.488%, the sensitivity was 68.09% and the specificity was 89.80%. Correlation analysis showed that Gensini score was positively correlated with HGI, TC, LDL-C, FBG, 2hPBG, serum creatinine(SCr) and HbA1c, but negatively correlated with SBP, DBP, HDL-C, LVEF and BMI(P < 0.05). Multiple linear regression analysis showed that even after adjusting for confounding factors, there was a dose-response relationship between Gensini score and HGI(P < 0.05).Conclusion HGI is an independent risk factor for coronary artery stenosis in patients with T2DM complicated with CHD. -

-
表 1 冠脉病变部位系数及管腔狭窄程度
Table 1. Coronary lesion location coefficient and lumen stenosis degree
冠脉病变部位 系数 管腔狭窄程度 评分 左主干 5 100% 32 左前降支或回旋支近段 2.5 91%~99% 16 左前降支或回旋支中段 1.5 76%~90% 8 左前降支或回旋支远段 1 51%~75% 4 右冠或第一对角支 1 26%~50% 2 小分支 0.5 1%~25% 1 表 2 一般资料比较
Table 2. General data
X±S 项目 T2DM组 T2DM+CHD组 t/χ2值 P值 男性/例% 18(36.7) 153(65.1) 13.623 < 0.01 年龄/岁 60.98±8.87 63.60±9.85 -1.722 0.086 病程/年 6.63±5.33 6.61±5.80 0.041 0.967 SBP/mmHg 143.88±17.85 135.81±19.92 2.649 0.09 DBP/mmHg 82.02±11.45 77.43±13.11 2.441 0.015 BMI/(kg·m-2) 25.63±3.81 24.71±3.07 1.805 0.072 载脂蛋白a/(mg·dL-1) 1.17±0.25 1.15±0.41 0.356 0.722 TC/(mmol·L-1) 4.18±1.04 4.16±1.11 0.493 0.87 TG/(mmol·L-1) 1.73±0.85 1.88±1.44 -0.812 0.417 HDL-C/(mmol·L-1) 1.08±0.23 0.97±0.26 0.142 0.049 LDL-C/(mmol·L-1) 2.59±0.88 2.634±0.95 0.041 0.968 SCr/(μmol·L-1) 77.61±43.46 90.77±58.87 -1.529 0.127 UA/(μmol·L-1) 336.94±90.81 347.83±111.31 0.319 0.586 载脂蛋白b/(mg·dL-1) 2.95±14.30 1.01±0.58 2.086 0.038 FPG/(mmol·L-1) 7.17±1.61 8.45±3.16 -2.555 0.011 HbA1c/% 6.66±0.87 8.48±1.69 -6.905 < 0.01 HGI/% -1.11±0.58 0.23±1.30 -6.725 < 0.01 2hPBG/(mmol·L-1) 11.22±2.90 12.56±3.85 -2.539 0.012 LVEF/% 64.09±7.54 58.64±8.75 3.73 < 0.01 吸烟/例(%) 12(24.5) 115(48.9) 9.082 < 0.01 饮酒/例(%) 7(14.3) 42(17.9) 0.365 0.546 表 3 Logistic回归分析影响T2DM合并CHD发生的危险因素
Table 3. Risk factors of T2DM complicated with CHD by logistic regression analysis
B SE Wald P值 OR(95%CI) HGI 1.093 0.349 9.82 0.002 2.985(1.506~5.915) 男性 1.125 0.408 7.607 0.006 3.081(1.385~6.856) DBP -0.049 0.017 8.121 0.004 0.952(0.920~0.985) LVEF -0.057 0.028 4.191 0.041 0.944(0.894~0.998) HbA1c 0.687 0.242 8.046 0.005 1.988(1.237~3.196) 表 4 T2DM合并CHD患者Gensini评分与HGI、冠心病危险因素的相关性
Table 4. Correlation of Gensini score with HGI and risk factors of CHD in patients with T2DM complicated with CHD
Gensini评分 HGI HbA1c SDP BDP SCr TC HDL-C LDL-C FPG 2hPBG LVEF BMI r值 0.644 0.621 -0.134 -0.136 0.140 0.258 -0.145 0.248 0.202 0.129 -0.408 -0.125 P值 < 0.05 < 0.05 0.024 0.022 0.018 < 0.05 0.015 < 0.05 < 0.05 0.029 < 0.05 0.035 表 5 T2DM合并CHD患者Gensini评分与HGI水平的多元线性回归分析
Table 5. Multiple linear regression analysis
项目 B(95%CI) SE Beta t P值 模型1 16.043(13.808~18.277) 1.135 0.644 14.13 < 0.01 模型2 15.809(13.622~17.996) 1.111 0.634 14.229 < 0.01 模型3 13.562(11.520~15.603) 1.037 0.544 13.077 < 0.01 模型4 13.701(11.705~15.696) 1.014 0.550 13.517 < 0.01 -
[1] Wang L, Gao P, Zhang M, et al. Prevalence and ethnic pattern of diabetes and prediabetes in China in 2013[J]. JAMA, 2017, 317(24): 2515-2523. doi: 10.1001/jama.2017.7596
[2] Sarwar N, Gao P, Seshasai SR, et al. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies[J]. Lancet, 2010, 375(9733): 2215-2222. doi: 10.1016/S0140-6736(10)60484-9
[3] Kalofoutis C, Piperi C, Kalofoutis A, et al. Type Ⅱ diabetes mellitus and cardiovascular risk factors: Current therapeutic approaches[J]. Exp Clin Cardiol, 2007, 12(1): 17-28.
[4] 林珑, 刘冠男, 高丽霓, 等. 经皮冠状动脉介入术后主要不良心脏事件危险因素研究进展[J]. 临床急诊杂志, 2020, 21(11): 918-922. https://www.cnki.com.cn/Article/CJFDTOTAL-ZZLC202011015.htm
[5] 杨坤, 陈剑飞, 刘林琼, 等. 急诊PCI术后急性造影剂相关性肾损伤发生情况及其影响因素分析[J]. 临床急诊杂志, 2021, 22(6): 390-394. https://www.cnki.com.cn/Article/CJFDTOTAL-ZZLC202106006.htm
[6] Herman WH, Ma Y, Uwaifo G, et al. Differences in A1C by race and ethnicity among patients with impaired glucose tolerance in the Diabetes Prevention Program[J]. Diabetes Care, 2007, 30(10): 2453-2457. doi: 10.2337/dc06-2003
[7] Hempe JM, Gomez R, McCarter RJ Jr, et al. High and low hemoglobin glycation phenotypes in type 1 diabetes: a challenge for interpretation of glycemic control[J]. J Diabetes Complications, 2002, 16(5): 313-320. doi: 10.1016/S1056-8727(01)00227-6
[8] Kim MK, Jeong JS, Yun JS, et al. Hemoglobin glycation index predicts cardiovascular disease in people with type 2 diabetes mellitus: A 10-year longitudinal cohort study[J]. J Diabetes Complications, 2018, 32(10): 906-910. doi: 10.1016/j.jdiacomp.2018.08.007
[9] Ahn CH, Min SH, Lee DH, et al. Hemoglobin glycation index is associated with cardiovascular diseases in people with impaired glucose metabolism[J]. J Clin Endocrinol Metab, 2017, 102(8): 2905-2913. doi: 10.1210/jc.2017-00191
[10] Dluhy RG, McMahon GT. Intensive glycemic control in the ACCORD and ADVANCE trials[J]. N Engl J Med, 2008, 358(24): 2630-2633. doi: 10.1056/NEJMe0804182
[11] UK Prospective Diabetes Study(UKPDS)Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes(UKPDS 33)[J]. Lancet, 1998, 352(9131): 837-853. doi: 10.1016/S0140-6736(98)07019-6
[12] Hempe JM, Liu S, Myers L, et al. The hemoglobin glycation index identifies subpopulations with harms or benefits from intensive treatment in the ACCORD trial[J]. Diabetes Care, 2015, 38(6): 1067-1074. doi: 10.2337/dc14-1844
[13] Mo Y, Zhou J, Ma X, et al. Haemoglobin A1c variability as an independent correlate of atherosclerosis and cardiovascular disease in Chinese type 2 diabetes[J]. Diab Vasc Dis Res, 2018, 15(5): 402-408. doi: 10.1177/1479164118778850
[14] Rhee EJ, Cho JH, Kwon H, et al. Association between coronary artery calcification and the hemoglobin glycation index: the kangbuk samsung health study[J]. J Clin Endocrinol Metab, 2017, 102(12): 4634-4641. doi: 10.1210/jc.2017-01723
[15] Cheng PC, Hsu SR, Cheng YC, et al. Relationship between hemoglobin glycation index and extent of coronary heart disease in individuals with type 2 diabetes mellitus: a cross-sectional study[J]. PeerJ, 2017, 5: e3875. doi: 10.7717/peerj.3875
[16] Felipe DL, Hempe JM, Liu S, et al. Skin intrinsic fluorescence is associated with hemoglobin A(1c)and hemoglobin glycation index but not mean blood glucose in children with type 1 diabetes[J]. Diabetes Care, 2011, 34(8): 1816-1820. doi: 10.2337/dc11-0049
[17] Fishman SL, Sonmez H, Basman C, et al. The role of advanced glycation end-products in the development of coronary artery disease in patients with and without diabetes mellitus: a review[J]. Mol Med, 2018, 24(1): 59. doi: 10.1186/s10020-018-0060-3
-




 下载:
下载: