Association between fasting blood glucose and microvascuar obstruction in nodiabetic patients with ST-elevation myocardial infarction after primary percutaneous coronary intervention
-
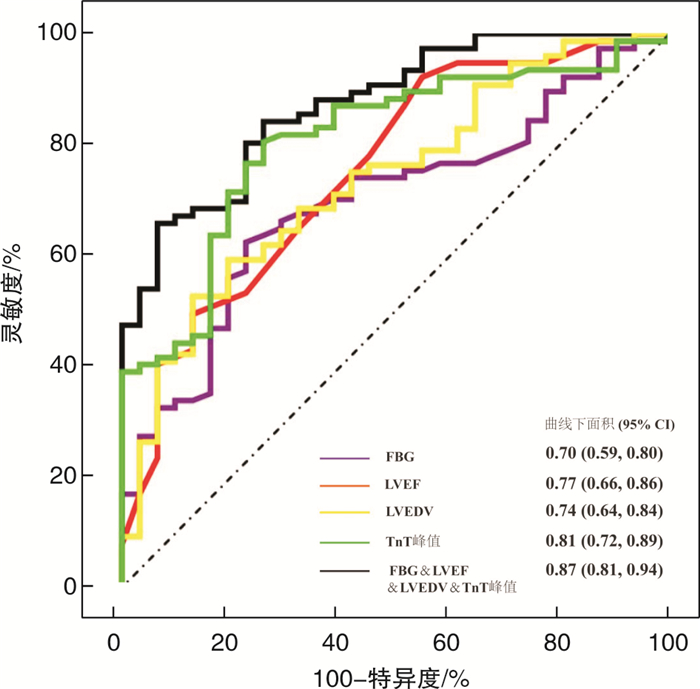
摘要: 目的 评估非糖尿病ST段抬高型心肌梗死(STEMI)患者空腹血糖(FBG)与直接经皮冠状动脉介入治疗(PPCI)术后发生微血管阻塞(MVO)的关系。方法 本研究入组108例非糖尿病STEMI患者,按照心脏磁共振结果分为MVO组及非MVO组。比较两组基础临床资料、实验室资料、介入手术资料、心脏超声及心脏磁共振资料。单因素及多因素logistic回归分析评估MVO的独立影响因子。受试者操作曲线(ROC)曲线评估FBG及联合指标的预测价值。结果 MVO组的FBG明显高于非MVO组。FBG、肌钙蛋白T峰值、左室射血分数及左室舒张末期容积均与MVO独立相关。ROC显示FBG曲线下面积为0.70,FBG>5.47 mmol/L预测MVO的灵敏度为0.623,特异度为0.774,联合指标的ROC曲线下面积为0.87。结论 FBG是非糖尿病STEMI患者PPCI术后发生MVO的独立预测因子,联合各个指标预测价值更高。
-
关键词:
- ST段抬高型心肌梗死 /
- 空腹血糖 /
- 微血管阻塞
Abstract: Objective To evaluate the relationship between fasting blood glucose(FBG) and microvascular occlusion(MVO) after primary percutaneous coronary intervention(PPCI) in nondiabetic patients with ST elevation myocardial infarction(STEMI).Methods A total of 108 nondabetic patients with STEMI were divided into MVO group and non MVO group according to the results of cardiac magnetic resonance. The basic clinical data, laboratory data, interventional surgery data, echocardiography and cardiac magnetic resonance imaging data were compared between the two groups. Univariate regression analysis and multivariate regression analysis were used to evaluate the independent predictors of MVO. Receiver operating characteristic(ROC) curve was used to evaluate the predictive value of FBG and other predictors.Results FBG of MVO group was significantly higher than that of non MVO group. FBG, peak TnT, LVEF and LVEDV were correlated with MVO independently. The ROC curve showed that the area under the curve of FBG was 0.70, the sensitivity and specificity of FBG>5.47 mmol/L in predicting MVO were 0.623 and 0.774, respectively. However, the area under the curve of the combination was 0.87.Conclusion FBG is an independent predictor of MVO after PPCI in nondiabetic STEMI patients. Furthermore, combination of the markers was a strong predictor for MVO after PPCI in nondiabetic STEMI patients. -

-
表 1 MVO组与非MVO组患者临床基线资料与实验室检查资料
Table 1. Clinical baseline data and laboratory examination data of patients in MVO group and non MVO group
例(%), X±S, M(P25, P75) 指标 非MVO组(31例) MVO组(77例) P值 年龄/岁 62.7±12.4 60.5±12.3 0.379 男性 24(77.4) 70(90.9) 0.109 高血压 15(48.4) 38(49.4) 0.928 梗死前心绞痛 11(35.5) 18(23.4) 0.199 吸烟 17(54.8) 45(58.4) 0.732 BMI/(kg·m-2) 24.7±2.7 24.8±3.1 0.830 收缩压/mmHg 133.4±24.4 127.7±25.6 0.291 舒张压/mmHg 83.5±10.2 84.2±13.1 0.788 心率/(次·min-1) 79.9±14.5 78.1±16.2 0.600 Killip分级 0.215 Ⅰ级 29(93.5) 68(88.3) - Ⅱ级 1(3.3) 6(7.8) - Ⅲ级 1(3.3) 0(0) - Ⅳ级 0(0) 3(3.9) - 发病至球囊通过时间/h 4.8(3.0,8.0) 5.0(3.5,8.0) 0.835 肌酐/(μmol·L-1) 72.5±18.6 71.6±14.5 0.796 C反应蛋白/(mg·L-1) 4.8(3.2,9.4) 6.3(3.7,14.8) 0.181 总胆固醇/(mmol·L-1) 4.2±0.8 4.1±0.8 0.797 HDL/(mmol·L-1) 1.0±0.3 1.0±0.3 0.894 LDL/(mmol·L-1) 2.5±0.7 2.5±0.7 0.959 FBG/(mmol·L-1) 5.2±0.6 6.0±1.8 0.010 HbA1c/% 5.8±0.5 6.0± 1.1 0.264 TnT峰值/(μg·L-1) 2.6(1.5,3.7) 6.7(4.2,10.0) < 0.001 BNP/(pg·mL-1) 33.1(19.0,104.0) 65.9(24.1,209.8) 0.356 表 2 MVO组与非MVO组患者介入、心脏超声、心脏磁共振相关资料
Table 2. Data related to intervention, echocardiography and cardiac magnetic resonance of patients in MVO group and non MVO group
例(%), X±S, M(P25, P75) 指标 非MVO组(31例) MVO组(77例) P值 梗死相关血管 0.229 左前降支 13(41.9) 45(58.4) - 左回旋支 4(12.9) 10(13.0) - 右冠状动脉 14(45.2) 22(28.6) - 血栓抽吸 10(32.3) 33(42.9) 0.309 SYNTAX评分/分 15.5(9.0,22.2) 15.0(11.0,22.5) 0.736 支架长度/mm 33.0(20.5,38.0) 33.0(23.0,46.0) 0.333 支架直径/mm 2.8±1.2 3.0±0.8 0.173 替罗非班 20(64.5) 53(68.8) 0.665 PCI术前TIMI 3级 5(16.1) 3(3.9) 0.042 PCI术后TIMI 3级 31(100.0) 74(96.1) 0.556 LVDD/cm 5.3±0.3 5.5±0.4 0.016 LAD/cm 4.0±0.3 4.1±0.4 0.076 LVEF/% 49.5±4.5 44.9±4.6 < 0.001 梗死面积/% 15.2(9.0,21.0) 21.0(17.0,30.2) 0.007 MVO面积/% 0(0,0) 2.0(1.0,3.7) < 0.001 LVEDV/mL 70.9±21.8 93.5±29.9 < 0.001 GRS/% 24.3±7.9 21.1±7.3 0.053 GCS/% -16.2±3.7 -13.8±3.1 0.001 GLS/% -9.9±3.0 -8.6±3.0 0.059 表 3 预测MVO因素的单因素和多因素回归分析
Table 3. Univariate regression analysis and multivariate logistic regression analysis of independent predictors of MVO
指标 单因素回归分析 多因素回归分析 OR(95%CI) P值 OR(95%CI) P值 年龄 0.98(0.95~1.02) 0.376 - - 女性 0.34(0.11~1.08) 0.067 - - FBG 2.47(1.31~4.68) 0.005 2.49(1.13~5.47) 0.0237 TnT峰值 1.42(1.20~1.66) < 0.001 1.27(1.02~1.59) 0.0332 术前TIMI血流3级 0.21(0.05~0.94) 0.042 - - LVDD 24.74(1.30~17.33) 0.019 - - LVEF 0.80(0.71~0.89) 0.001 0.77(0.63~0.94) 0.0112 梗死面积 1.06(1.02~1.12) 0.010 - - LVEDV 1.04(1.02~1.06) < 0.001 1.04(1.01~1.07) 0.0223 GLS 1.15(0.99~1.33) 0.064 - - -
[1] Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation[J]. Kardiol Pol, 2018, 76(2): 229-313. doi: 10.5603/KP.2018.0041
[2] 肖宇杨. 急性心肌梗死患者冠状动脉微循环灌注障碍风险评估及功能检测的系列研究[D]. 石家庄: 河北医科大学, 2018: 222.
[3] Pinto DS, Kirtane AJ, Pride YB, et al. Association of blood glucose with angiographic and clinical outcomes among patients with ST-segment elevation myocardial infarction(from the CLARITY-TIMI-28 study). [J]. Am J Cardiol, 2008, 101(3): 303-307. doi: 10.1016/j.amjcard.2007.08.034
[4] Galea N, Dacquino GM, Ammendola RM, et al. Microvascular obstruction extent predicts major adverse cardiovascular events in patients with acute myocardial infarction and preserved ejection fraction. [J]. Eur Radiol, 2019, 29(5): 2369-2377. doi: 10.1007/s00330-018-5895-z
[5] 马敏, 贺勇. 冠状动脉微血管阻塞的临床及心脏磁共振研究进展. [J]. 临床心血管病杂志, 2017, 33(10), 937-940. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXB201710005.htm
[6] Geng N, Ren L, Xu L, et al. Clinical outcomes of nicorandil administration in patients with acute ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention: a systematic review and meta-analysis of randomized controlled trials. [J]. BMC Cardiovasc Disord, 2021, 21(1): 488. doi: 10.1186/s12872-021-02301-1
[7] Corban MT, Khorramirouz R, Yang SW, et al. Non-infarct related artery microvascular obstruction is associated with worse persistent diastolic dysfunction in patients with revascularized ST elevation myocardial infarction[J]. Int J Cardiol, 2020, 300: 27-33. doi: 10.1016/j.ijcard.2019.09.043
[8] van Lavieren MA, Bax M, Stegehuis VE, et al. Acute alterations in glucose homeostasis impact coronary microvascular function in patients presenting with ST-segment elevation myocardial infarction. [J]. Neth Heart J, 2020, 28(3): 161-170. doi: 10.1007/s12471-020-01366-5
[9] Khalfallah M, Abdelmageed R, Elgendy E, et al. Incidence, predictors and outcomes of stress hyperglycemia in patients with ST elevation myocardial infarction undergoing primary percutaneous coronary intervention. [J]. Diab Vasc Dis Res, 2020, 17(1): 1-7.
[10] Niccoli G, Scalone G, Lerman A, et al. Coronary microvascular obstruction in acute myocardial infarction. [J]. Eur Heart J, 2016.37(13): 1024-1033. doi: 10.1093/eurheartj/ehv484
[11] Zhang Z, Zhang S, Wang Y, et al. Autophagy inhibits high glucose induced cardiac microvascular endothelial cells apoptosis by mTOR signal pathway. [J]. Apoptosis, 2017, 22(12): 1510-1523. doi: 10.1007/s10495-017-1398-7
[12] Yan X, Xun M, Dou X, et al. Regulation of Na(+)-K(+)-ATPase effected high glucose-induced myocardial cell injury through c-Src dependent NADPH oxidase/ROS pathway. [J]. Exp Cell Res, 2017, 357(2): 243-251. doi: 10.1016/j.yexcr.2017.05.023
[13] Qiu Z, He Y, Ming H, et al. Lipopolysaccharide(LPS)Aggravates High Glucose-and Hypoxia/Reoxygenation-Induced Injury through Activating ROS-Dependent NLRP3 Inflammasome-Mediated Pyroptosis in H9C2 Cardiomyocytes[J]. J Diabetes Res, 2019, 2019: 8151836.
[14] Padilla J, Carpenter AJ, Das NA, et al. TRAF3IP2 mediates high glucose-induced endothelin-1 production as well as endothelin-1-induced inflammation in endothelial cells. [J]. Am J Physiol Heart Circ Physiol, 2018, 314(1): H52-H64. doi: 10.1152/ajpheart.00478.2017
[15] Dangwal S, Rauch BH, Gensch T, et al. High glucose enhances thrombin responses via protease-activated receptor-4 in human vascular smooth muscle cells. [J]. Arterioscler Thromb Vasc Biol, 2011, 31(3): 624-633. doi: 10.1161/ATVBAHA.110.219105
[16] Sudic D, Razmara M, Forslund M, et al. High glucose levels enhance platelet activation: involvement of multiple mechanisms. [J]. Br J Haematol, 2006, 133(3): 315-322. doi: 10.1111/j.1365-2141.2006.06012.x
-




 下载:
下载: