Correlation between breast arterial calcification and coronary heart disease diagnosed by coronary computed tomography angiography in women
-
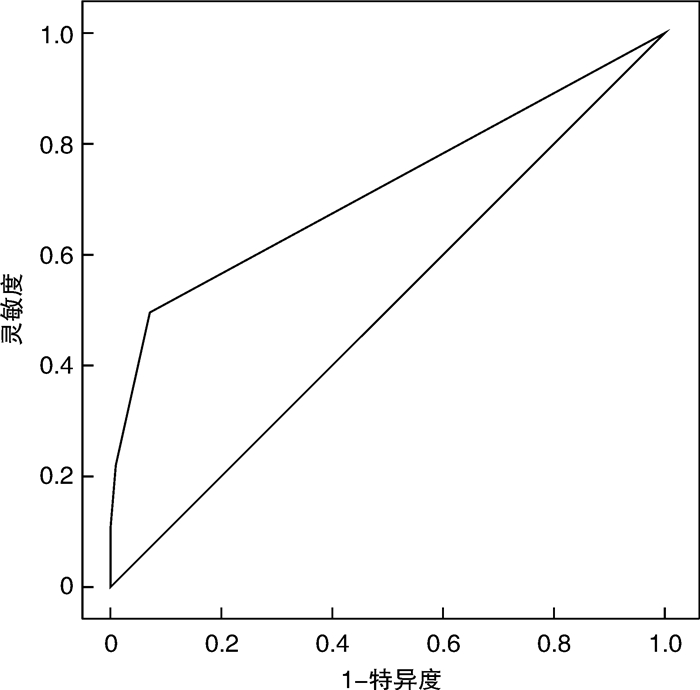
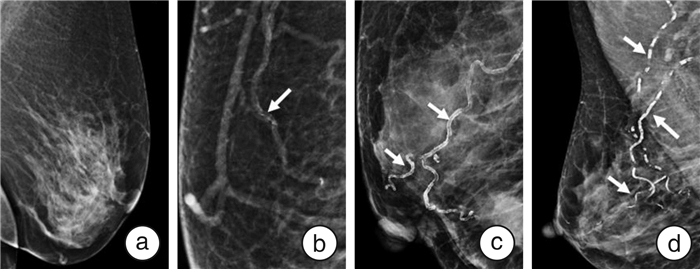
摘要: 目的 探讨女性经乳腺钼靶X线检查发现的乳房动脉钙化(BAC)与冠状动脉CT血管成像(CCTA)诊断的冠心病之间的相关性,评估BAC在女性人群中对冠心病的诊断价值。方法 收集我院2019年1月—2020年12月行双侧乳腺钼靶X线检查与CCTA且检查间隔不超过6个月的217例女性患者资料,分别使用BAC的4分制法与CAD-RADS评分系统对BAC及冠心病进行量化。比较BAC阳性与BAC阴性、冠心病阳性与冠心病阴性组的一般资料,使用单因素与多因素logistic回归分析研究BAC与冠心病的关系。使用Spearman相关性分析评估BCA分级与CAD-RADS分级的相关性。绘制BAC预测冠心病诊断的ROC曲线,计算曲线下面积,评估BAC对冠心病的诊断价值。结果 冠心病患病率为14.75%(32例),BAC阳性患病率为13.36%(29例)。冠心病组BAC阳性率较非冠心病组高(P < 0.05)。对冠心病影响因素的单因素logistic分析显示,BAC阳性与冠心病相关(OR=13.231,95%CI 5.415~32.326,P < 0.001)。在多因素logistic回归分析中,调整传统的冠心病危险因素后,BAC阳性仍与冠心病显著相关,是冠心病的独立危险因素(OR=8.879,95%CI 2.945~26.765,P < 0.001)。Spearman秩相关分析显示,BAC分级与CAD-RADS分级呈正相关(r=0.404,P < 0.001)。BAC预测冠心病的曲线下面积为0.720,灵敏度、特异度、阳性预测值、阴性预测值、准确率分别为50.00%、92.97%、55.17%、91.49%、86.64%。结论 在女性人群中发现的BAC是冠心病的独立危险因素,BAC严重程度与冠心病的严重程度呈正相关。BAC在女性冠心病中具有一定的诊断价值。Abstract: Objective To explore the correlation between female breast arterial calcification(BAC) in mammography and coronary heart disease(CHD) diagnosed by CCTA, and to evaluate the diagnostic value of BAC in the female patients with CHD.Methods The data of 217female patients who underwent bilateral mammary mammography and CCTA with an interval of no more than 6 months from January 2019 to December 2020 were collected. BAC and CHD were quantified by BAC 4-score system and CAD-RADS score system respectively. The general data of positive BAC and negative BAC groups, positive CHD and negative CHD groups were compared. The relationship between BAC and CHD were studied by univariate and multivariate logistic regression analysis. Spearman correlation analysis was used to evaluate the correlation between BCA classification and CAD-RADS classification. We drew the ROC curve of BAC for predicting the diagnosis of CHD and calculated the area under curve(AUC) to evaluate the diagnostic value of BAC for CHD.Results The prevalence of CHD was 14.75%(n=32) and the prevalence of positive BAC was 13.36(n=29). BAC positivity was more frequent in the positive CHD group than in the negative CHD group(P < 0.05), and univariate logistic analysis of the influencing factors for CHD showed that BAC positivity was associated with CHD(OR=13.231, 95%CI: 5.415~32.326, P < 0.001). In multivariate logistic regression analysis, BAC positivity remained significantly associated with CHD after adjustment for traditional CHD risk factors and was an independent risk factor for CHD(OR=8.879, 95%CI: 2.945~26.765, P < 0.001). Spearman rank correlation analysis showed that there was a positive correlation between BAC grade and CAD-RADS grade(r=0.404, P < 0.001). AUC of BAC for predicting coronary heart disease was 0.720. The sensitivity, specificity, positive predictive value, negative predictive value and accuracy were 50.00%, 92.97%, 55.17%, 91.49% and 86.64% respectively.Conclusion Female BAC is an independent risk factor for CHD in women. The severity of female BAC is positively correlated with the severity of CHD. BAC has a certain diagnostic value for CHD in women.
-
Key words:
- breast arterial calcification /
- coronary heart disease /
- diagnosis /
- female /
- imaging
-

-
表 1 冠心病组与非冠心病组的一般资料比较
Table 1. Comparison of general data between positive CHD group and negative CHD group
x±s 项目 冠心病组(32例) 非冠心病组(185例) t/χ2值 P值 年龄/岁 61.75±9.05 55.13±9.29 3.738 < 0.001 高脂血症/例(%) 14(43.75) 44(23.78) 5.553 0.018 高血压/例(%) 23(71.88) 33(17.84) 41.606 < 0.001 糖尿病/例(%) 9(28.13) 20(10.81) 5.647 0.017 卒中史/例(%) 3(9.38) 9(4.86) 0.374 0.541 冠心病家族史/例(%) 6(18.75) 9(4.86) 6.159 0.013 吸烟/例(%) 5(15.63) 4(2.16) 9.282 0.002 生产次数/次 1.97±0.99 1.65±0.68 1.744 0.090 已绝经/例(%) 28(87.50) 113(61.08) 8.367 0.004 BAC阳性/例(%) 16(50.00) 13(7.03) 39.880 < 0.001 表 2 BAC阳性组与BAC阴性组的一般资料比较
Table 2. Comparison of general data between positive BAC group and negative BAC group
x±s 项目 BAC阳性(29例) BAC阴性(188例) t/χ2值 P值 年龄/岁 62.34±8.18 55.14±9.37 3.913 < 0.001 高脂血症/例(%) 11(37.93) 47(25.00) 2.145 0.143 高血压/例(%) 21(72.41) 35(18.62) 37.976 < 0.001 糖尿病/例(%) 8(27.59) 21(11.17) 4.516 0.034 卒中史/例(%) 4(13.79) 8(4.26) 2.740 0.098 冠心病家族史/例(%) 1(3.45) 14(7.45) 0.158 0.691 吸烟/例(%) 3(10.34) 6(3.19) 1.685 0.194 生产次数/次 2.55±0.83 1.56±0.63 6.160 < 0.001 已绝经/例(%) 25(86.21) 116(61.70) 6.630 0.010 表 3 冠心病影响因素的单因素logistic回归分析
Table 3. Univariate logistic regression analysis of influencing factors of CHD
项目 β值 S Wald χ2值 OR值 95%CI P值 年龄 0.070 0.020 11.918 1.073 1.031~1.117 0.001 高脂血症 0.913 0.396 5.319 2.492 1.147~5.416 0.021 高血压 2.466 0.438 31.751 11.711 4.993~27.751 < 0.001 糖尿病 1.172 0.459 6.52 3.228 1.313~7.937 0.011 冠心病家族史 1.507 0.567 7.054 4.513 1.484~13.722 0.008 吸烟 2.126 0.702 9.175 8.38 2.118~33.161 0.002 绝经 1.495 0.555 7.248 4.46 1.502~13.046 0.007 BAC阳性 2.583 0.456 32.106 13.231 5.415~32.326 < 0.001 表 4 冠心病影响因素的多因素logistic回归分析
Table 4. Multivariate logistic regression analysis of influencing factors of CHD
项目 β值 S Wald χ2值 OR值 95%CI P值 年龄 0.022 0.036 0.378 0.978 0.913~1.049 0.539 高脂血症 1.136 0.537 4.471 3.114 1.087~8.924 0.034 高血压 1.470 0.568 6.689 4.350 1.428~13.253 0.010 糖尿病 0.208 0.644 0.104 0.812 0.230~2.871 0.747 冠心病家族史 1.833 0.707 6.726 6.253 1.565~24.988 0.010 吸烟 2.348 0.991 5.615 10.463 1.500~72.957 0.018 绝经 0.775 0.817 0.901 2.171 0.438~10.758 0.342 BAC阳性 2.184 0.563 15.045 8.879 2.945~26.765 < 0.001 表 5 BAC阳性影响因素的单因素logistic回归分析
Table 5. univariate logistic regression analysis of influencing factors of positive BAC
项目 β值 S Wald χ2值 OR值 95%CI P值 年龄 0.076 0.021 12.781 1.079 1.035~1.125 < 0.001 高血压 2.440 0.456 28.665 11.475 4.697~28.035 < 0.001 糖尿病 1.108 0.476 5.431 3.029 1.193~7.695 0.020 生产次数 1.860 0.336 30.661 6.425 3.326~12.411 < 0.001 已绝经 1.356 0.559 5.881 3.879 1.297~11.604 0.015 表 6 BAC阳性影响因素的多因素logistic回归分析
Table 6. multivariate logistic regression analysis of influencing factors of positive BAC
项目 β值 S Wald χ2值 OR值 95%CI P值 年龄 0.076 0.036 4.525 1.079 1.006~1.157 0.033 高血压 1.901 0.566 11.287 6.689 2.207~20.273 0.001 糖尿病 0.991 0.710 1.947 0.371 0.092~1.493 0.163 生产次数 1.649 0.352 21.900 5.201 2.607~10.376 < 0.001 已绝经 0.610 0.860 0.503 0.543 0.101~2.931 0.478 表 7 BAC分级与CAD-RADS分级的关系
Table 7. relationship between BAC classification and CAD-RADS classification
例 BAC分级 CAD-RADS分级 总计 0级 1级 2级 3级 4a级 4b级 5级 1级 102 11 59 13 3 0 0 188 2级 3 1 7 6 3 0 0 20 3级 0 1 1 1 2 1 0 6 4级 0 0 0 1 2 0 0 3 总计 105 13 67 21 10 1 0 217 -
[1] Virani SS, Alonso A, Aparicio HJ, et al. Heart Disease and Stroke Statistics-2021 Update: A Report From the American Heart Association[J]. Circulation, 2021, 143(8): e254-e743.
[2] Brown HL, Warner JJ, Gianos E, et al. Promoting risk identification and reduction of cardiovascular disease in women through collaboration with obstetricians and gynecologists: a presidential advisory from the American Heart Association and the American College of Obstetricians and Gynecologists[J]. Circulation, 2018, 137(24): e843-e852.
[3] Wilmot KA, O'Flaherty M, Capewell S, et al. Coronary heart disease mortality declines in the United States from 1979 through 2011: evidence for stagnation in young adults, especially women[J]. Circulation, 2015, 132(11): 997-1002. doi: 10.1161/CIRCULATIONAHA.115.015293
[4] Shaw LJ, Bairey Merz CN, Pepine CJ, et al. Insights from the NHLBI-Sponsored Women's Ischemia Syndrome Evaluation(WISE)Study: Part Ⅰ: gender differences in traditional and novel risk factors, symptom evaluation, and gender-optimized diagnostic strategies[J]. J Am Coll Cardiol, 2006, 47(3 Suppl): S4-S20.
[5] Goff DC Jr, Lloyd-Jones DM, Bennett G, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines[J]. J Am Coll Cardiol, 2014, 63(25 Pt B): 2935-2959.
[6] Yoon YE, Yun B, Kim KM, et al. Breast Arterial calcification: a potential biomarker for atherosclerotic cardiovascular disease risk?[J]. Curr Atheroscler Rep, 2021, 23(5): 21. doi: 10.1007/s11883-021-00924-5
[7] Suh JW, Yun B. Breast arterial calcification: a potential surrogate marker for cardiovascular disease[J]. J Cardiovasc Imaging, 2018, 26(3): 125-134. doi: 10.4250/jcvi.2018.26.e20
[8] Lee SC, Phillips M, Bellinge J, et al. Is breast arterial calcification associated with coronary artery disease?-A systematic review and meta-analysis[J]. PLoS One, 2020, 15(7): e0236598. doi: 10.1371/journal.pone.0236598
[9] Xie JX, Cury RC, Leipsic J, et al. The Coronary Artery Disease-Reporting and Data System(CAD-RADS): prognostic and clinical implications associated with standardized coronary computed tomography angiography reporting[J]. JACC Cardiovasc Imaging, 2018, 11(1): 78-89. doi: 10.1016/j.jcmg.2017.08.026
[10] Abouzeid C, Bhatt D, Amin N. The top five women's health issues in preventive cardiology[J]. Curr Cardiovasc Risk Rep, 2018, 12(2): 6. doi: 10.1007/s12170-018-0568-7
[11] 郭福佳, 袁正强, 施尚鹏, 等. 早发与晚发冠心病患者临床及冠状动脉病变特点的性别差异分析[J]. 临床心血管病杂志, 2021, 37(1): 28-31. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXB202101006.htm
[12] 蔡莉娜, 杨文博, 强红丽, 等. 393例女性冠心病患者的临床特征及预后探讨[J]. 临床心血管病杂志, 2018, 34(9): 876-879. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXB201809009.htm
[13] 白小涓, 韩璐璐. 关注女性缺血性心脏病冠状动脉微血管病变[J]. 临床心血管病杂志, 2019, 35(10): 871-875. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXB201910001.htm
[14] Trimboli RM, Codari M, Guazzi M, et al. Screening mammography beyond breast cancer: breast arterial calcifications as a sex-specific biomarker of cardiovascular risk[J]. Eur J Radiol, 2019, 119: 108636. doi: 10.1016/j.ejrad.2019.08.005
[15] Quispe R, Al-Rifai M, Di Carlo PA, et al. Breast arterial calcium: a game changer in women's cardiovascular health?[J]. JACC Cardiovasc Imaging, 2019, 12(12): 2538-2548. doi: 10.1016/j.jcmg.2018.07.035
[16] Yoon YE, Kim KM, Lee W, et al. Breast arterial calcification is associated with the progression of coronary atherosclerosis in asymptomatic women: A Preliminary Retrospective Cohort Study[J]. Sci Rep, 2020, 10(1): 2755. doi: 10.1038/s41598-020-59606-y
[17] Kelly BS, ScanlON E, Heneghan H, et al. Breast Arterial Calcification on screening mammography can predict significant Coronary Artery Disease in women[J]. Clin Imaging, 2018, 49: 48-53. doi: 10.1016/j.clinimag.2017.10.021
[18] Huang Z, Xiao J, Xie Y, et al. The correlation of deep learning-based CAD-RADS evaluated by coronary computed tomography angiography with breast arterial calcification on mammography[J]. Sci Rep, 2020, 10(1): 11532. doi: 10.1038/s41598-020-68378-4
[19] Fathala A L, Alfaer F, Aldurabi A, et al. Breast arterial calcification on mammography does not predict coronary artery disease by invasive coronary angiography[J]. Ann Saudi Med, 2020, 40(2): 81-86. doi: 10.5144/0256-4947.2020.81
[20] Yoon YE, Kim KM, Han JS, et al. Prediction of subclinical coronary artery disease with breast arterial calcification and low bone mass in asymptomatic women: registry for the women health cohort for the BBC Study[J]. JACC Cardiovasc Imaging, 2019, 12(7 Pt 1): 1202-1211.
[21] Osman M, Regner S, Osman K, et al. Association between breast arterial calcification on mammography and coronary artery disease: a systematic review and meta-Analysis[J]. J Womens Health(Larchmt), 2021, 10: 111.
[22] Margolies LR, Yip R, Hwang E, et al. Breast arterial calcification in the mammogram report: the patient perspective[J]. AJR Am J Roentgenol, 2019, 212(1): 209-214. doi: 10.2214/AJR.18.20171
[23] 中国抗癌协会乳腺癌专业委员会. 中国抗癌协会乳腺癌诊治指南与规范(2019年版)[J]. 中国癌症杂志, 2019, 29(8): 609-679. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGAZ202110015.htm
[24] 李文涛. 《中国女性乳腺癌筛查标准(T/CPMA 014-2020)》解读[J]. 中华实用诊断与治疗杂志, 2021, 35(5): 433-435. https://www.cnki.com.cn/Article/CJFDTOTAL-HNZD202105001.htm
-




 下载:
下载: