Clinical analysis of seven cases of pulmonary hypertension in children with gene mutation
-
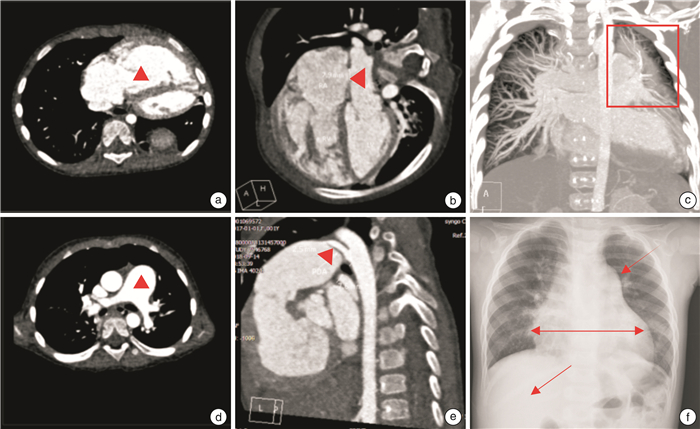
摘要: 收集2014年1月-2018年3月就诊我院,右心导管确诊肺动脉高压,基因检测阳性的患儿共7例,分析其临床特点及预后转归。不明原因儿童肺动脉高压基因阳性发病率为32%,其中BMPR2突变3例,ACVRL1突变2例,FLNA突变1例,NOTCH3突变1例,KMT2D突变1例。男女比例为1∶6,初诊年龄8个月~15岁,随访时间9~31个月。所有患儿均有活动耐量下降,随访中1例因大咯血死亡,2例因心力衰竭死亡,2例出现心力衰竭加重在调整治疗后病情平稳,2例病情平稳。Abstract: A total of 7 children with pulmonary hypertension diagnosed by right cardiac catheterization and positive gene test were collected from January 2014 to March 2018. Their clinical characteristics and prognosis were analyzed. Incidence of gene mutation was 32%. Of which three were BMPR2 mutation, two were ACVRL1 mutation, one was FLNA mutation, one was NOTCH3 mutation, and one was KMT2D mutation. The ratio of male to female was 1∶6. The first diagnosis age was 8 months to 15 years old, and the follow-up time was 9 to 31 months. All the children had decreased activity tolerance. In the follow-up, 1 case died of massive hemoptysis, 2 cases died of heart failure, 2 cases developed heart failure aggravation, and 2 cases were stable.
-
Key words:
- children /
- pulmonary arterial hypertension /
- gene mutation /
- gene detection
-

-
表 1 7例基因突变PAH患儿一般情况
Table 1. General data
例序 性别 年龄 基因及突变类型 NT-proBNP/(pg·mL-1) 症状 NYHA心功能 合并CHD 靶向药物 随访时间/月 随访结果 1 女 9岁 BMPR2、错义突变 710 活动耐量下降 Ⅱ 无 波生坦他达拉非 31 病情反复 2 男 15岁 ACVRL1、错义突变 1192 活动耐量下降、咯血 Ⅲ 无 波生坦西地拉非 9 死亡 3 女 8个月 FLNA、剪切突变 15 000 活动耐量下降、反复呼吸道感染 Ⅳ PDA(2 mm)ASD(5 mm) 波生坦 20 死亡 4 女 3岁 BMPR2、错义突变ACVRL1、错义突变 8000 活动耐量下降 Ⅳ 无 波生坦 12 死亡 5 女 9岁 NOTCH3、错义突变 430 活动耐量下降 Ⅱ PFO 波生坦他达拉非 16 平稳 6 女 3.5岁 KMT2D、移码突变 1200 活动耐量下降 Ⅳ ASD(5 mm)VSD(3 mm) 波生坦西地拉非瑞莫杜林 21 病情反复 7 女 10岁 BMPR2、移码突变 410 活动耐量下降 Ⅱ 无 波生坦他达拉非 10 平稳 注:CHD为先天性心脏病。 表 2 7例基因突变PAH患儿心脏超声数据
Table 2. Echocardiographic data
mm 例序 右房内径 左房内径 右室内径 左室内径 肺动脉内径 主动脉内径 1 32 22 35 32 29 19 2 80 31 70 35 39 23 3 36 19 35 25 24 16 4 23 19 29 25 24 17 5 29 22 34 30 21 17 6 24 19 29 24 23 17 7 30 23 35 30 21 18 表 3 7例基因突变PAH患儿右心导管数据
Table 3. Data of right heart catheterization
例序 MPAP/mmHg DAP/mmHg PVR/(WOOD·U) PVRI/(WOODU·m-2) CO/(L·min-1) CI/(L·min-2) 1 60 62 11.4 15.1 3.77 2.86 2 71 73 18.1 35 6.31 3.26 3 第一次
第二次2467 7056 1741.9 5.419 1.131.85 3.64.07 4 69 66 55.7 24.8 1.37 1.46 5 90 95 43.1 41.4 6.61 6.88 6 68 67 - - - - 7 46 75 - - - - 注:DAP为降主动脉压;PVRI为肺血管阻力指数;CO为心输出量。 表 4 7例基因突变PAH患儿随访数据
Table 4. Follow-up data
随访项目 例1 例2 例3 例4 例5 例6 例7 NT-proBNP/(pg·mL-1) 基线 710 1192 15 000 8 000 430 1 200 410 随访 41.2 >35 000 >35 000 >35 000 - 443.7 151.3 NYHA心功能 基线 Ⅱ Ⅲ Ⅳ Ⅳ Ⅱ Ⅳ Ⅱ 随访 Ⅱ Ⅳ Ⅳ Ⅳ Ⅱ Ⅲ Ⅱ RV/LV 基线 1.1 2 1.4 1.2 1.1 1.2 1.2 随访 1.1 2.2 1.6 1.4 0.8 1.1 1.3 结局 存活 死亡 死亡 死亡 存活 存活 存活 注:RV/LV为右室舒张末内径/左室舒张末内径。 -
[1] Deng X, Jin B, Li S, et al. Guideline implementation and early risk assessment in pulmonary arterial hypertension associated with congenital heart disease: A retrospective cohort study[J]. Clin Respir J, 2019, 13(11): 693-699. doi: 10.1111/crj.13076
[2] 中华医学会心血管病学分会肺血管病学组, 中华心血管病杂志编辑委员会. 中国肺高血压诊断和治疗指南2018[J]. 中华心血管病杂志, 2018, 46(12): 933-964. doi: 10.3760/cma.j.issn.0253-3758.2018.12.006
[3] 秦雨晗, 乔勇, 鄢高亮, 等. CDK1基因在肺动脉高压中表达和临床意义的生物信息学分析[J]. 临床心血管病杂志, 2021, 37(7): 651-658. http://lcxb.cbpt.cnki.net/WKC/WebPublication/paperDigest.aspx?paperID=483c5527-48a4-4c03-8424-1829a0f0ae27
[4] Hansmann G, Koestenberger M, Alastalo TP, et al. 2019 updated consensus statement on the diagnosis and treatment of pediatric pulmonary hypertension: The European Pediatric Pulmonary Vascular Disease Network(EPPVDN), endorsed by AEPC, ESPR and ISHLT[J]. J Heart Lung Transplant, 2019, 38(9): 879-901. doi: 10.1016/j.healun.2019.06.022
[5] Rosenzweig EB, Abman SH, Adatia I, et al. Paediatric pulmonary arterial hypertension: updates on definition, classification, diagnostics and management[J]. Eur Respir J, 2019, 53(1): 100.
[6] Zhu N, Gonzaga-Jauregui C, Welch CL, et al. Exome sequencing in children with pulmonary arterial hypertension demonstrates differences compared with adults[J]. Circ Genom Precis Med, 2018, 11(4): e001887. doi: 10.1161/CIRCGEN.117.001887
[7] Welch CL, Austin ED, Chung WK. Genes that drive the pathobiology of pediatric pulmonary arterial hypertension[J]. Pediatr Pulmonol, 2021, 56(3): 614-620. doi: 10.1002/ppul.24637
[8] Welch CL, Chung WK. Genetics and other omics in pediatric pulmonary arterial hypertension[J]. Chest, 2020, 157(5): 1287-1295. doi: 10.1016/j.chest.2020.01.013
[9] Barozzi C, Galletti M, Tomasi L, et al. A Combined targeted and whole exome sequencing approach identified novel candidate genes involved in heritable pulmonary arterial hypertension[J]. Sci Rep, 2019, 9(1): 753. doi: 10.1038/s41598-018-37277-0
[10] Tatius B, Wasityastuti W, Astarini FD, et al. Significance of BMPR2 mutations in pulmonary arterial hypertension[J]. Respir Investig, 2021, 59(4): 397-407. doi: 10.1016/j.resinv.2021.03.011
[11] Zhu N, Pauciulo MW, Welch CL, et al. Novel risk genes and mechanisms implicated by exome sequencing of 2572 individuals with pulmonary arterial hypertension[J]. Genome Med, 2019, 11(1): 69. doi: 10.1186/s13073-019-0685-z
[12] Rhodes CJ, Batai K, Bleda M, et al. Genetic determinants of risk in pulmonary arterial hypertension: international genome-wide association studies and meta-analysis[J]. Lancet Respir Med, 2019, 7(3): 227-238. doi: 10.1016/S2213-2600(18)30409-0
[13] Yokokawa T, Sugimoto K, Kimishima Y, et al. Pulmonary hypertension and hereditary hemorrhagic telangiectasia related to an ACVRL1 mutation[J]. Intern Med, 2020, 59(2): 221-227. doi: 10.2169/internalmedicine.3625-19
[14] Zhang HS, Liu Q, Piao CM, et al. Genotypes and phenotypes of chinese pediatric patients with idiopathic and heritable pulmonary arterial hypertension-a single-center study[J]. Can J Cardiol, 2019, 35(12): 1851-1856. doi: 10.1016/j.cjca.2019.07.628
[15] Piao C, Zhu Y, Zhang C, et al. Identification of multiple ACVRL1 mutations in patients with pulmonary arterial hypertension by targeted exome capture[J]. Clin Sci(Lond), 2016, 130(17): 1559-1569. doi: 10.1042/CS20160247
[16] Morris HE, Neves KB, Montezano AC, et al. Notch3 signalling and vascular remodelling in pulmonary arterial hypertension[J]. Clin Sci(Lond), 2019, 133(24): 2481-2498. doi: 10.1042/CS20190835
[17] Rafikova O, Al Ghouleh I, Rafikov R. Focus on early events: pathogenesis of pulmonary arterial hypertension development[J]. Antioxid Redox Signal, 2019, 31(13): 933-953. doi: 10.1089/ars.2018.7673
[18] Harter ZJ, Agarwal S, Dalvi P, et al. Drug abuse and HIV-related pulmonary hypertension: double hit injury[J]. AIDS, 2018, 32(18): 2651-2667. doi: 10.1097/QAD.0000000000002030
[19] 李璐, 张改秀, 阎亚琼, 等. 甲基丙二酸血症患者临床特征及基因突变分析[J]. 山西医科大学学报, 2020, 51(9): 986-994. https://www.cnki.com.cn/Article/CJFDTOTAL-SXYX202009018.htm
[20] Zhou J, Kang X, An H, et al. The function and pathogenic mechanism of filamin A[J]. Gene, 2021, 784: 145575. doi: 10.1016/j.gene.2021.145575
[21] Deng X, Li S, Qiu Q, et al. Where the congenital heart disease meets the pulmonary arterial hypertension, FLNA matters: a case report and literature review[J]. BMC Pediatr, 2020, 20(1): 504. doi: 10.1186/s12887-020-02393-2
[22] Wang YR, Xu NX, Wang J, et al. Kabuki syndrome: review of the clinical features, diagnosis and epigenetic mechanisms[J]. World J Pediatr, 2019, 15(6): 528-535. doi: 10.1007/s12519-019-00309-4
[23] uk M, Mazurkiewicz-Antoń K, Migdał A, et al. Prognosis in children with pulmonary arterial hypertension: 10-year single-centre experience[J]. Kardiol Pol, 2016, 74(2): 159-167. doi: 10.5603/KP.a2015.0120
[24] Lin Nie, Jun Li, et al. Correlation between right ventricular-pulmonary artery coupling and the prognosis of patients with pulmonary arterial hypertension[J]. Medicine(Baltimore), 2019, 98(40): e17369.
-




 下载:
下载: