Correlation between alanine aminotransferase and early spontaneous recanalization of infarct related arteries in patients with acute ST segment elevation myocardial infarction
-
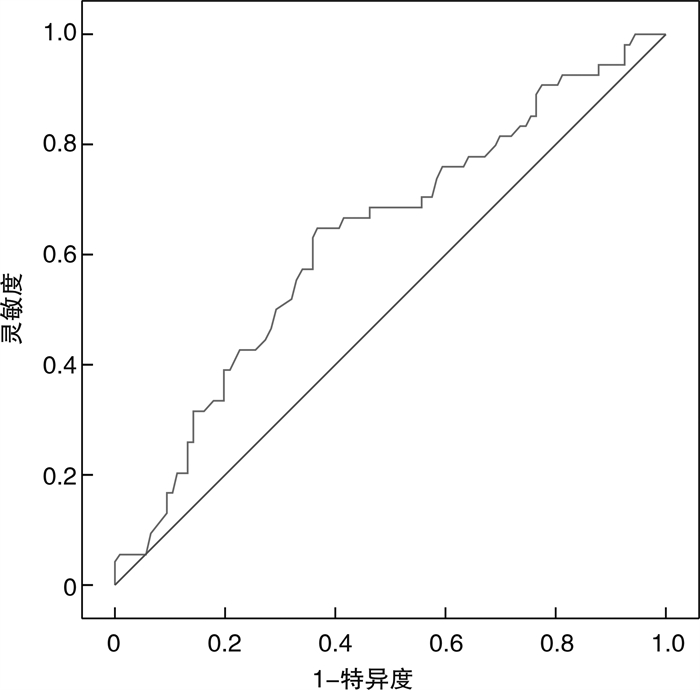
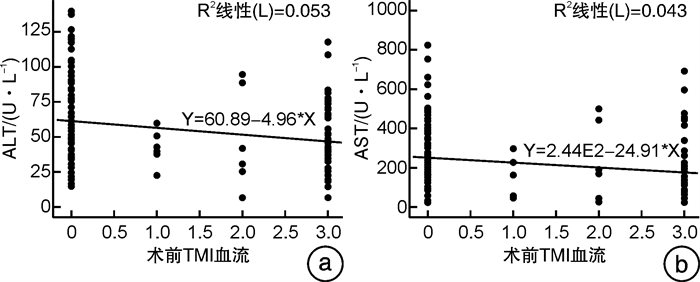
摘要: 目的 急性ST段抬高型心肌梗死(STEMI)患者常发生梗死相关动脉(IRA)的早期自发再通(ESR)。本研究旨在探讨急性STEMI患者IRA-ESR的相关性。方法 对福建医科大学附属闽东医院胸痛中心2020年1月1日—2022年1月31日住院的急性STEMI患者临床资料进行回顾分析。符合入选条件者160例,根据冠状动脉(冠脉)造影判断IRA-TIMI血流分级,将其分为ESR组54例和无自发再通(NSR)组106例;比较2组患者的基线数据以及急诊经皮冠脉介入手术前的谷草转氨酶(AST)和谷丙转氨酶(ALT);采用斯皮尔曼等级变量相关性分析法对AST、ALT与IRA-TIMI血流相关性进行分析;采用二元logistic多因素回归分析筛选IRA-ESR的影响因素,绘制受试者工作特征曲线(ROC),评价ALT预测IRA-ESR的价值。结果 急性STEMI患者NSR组ALT、AST均显著高于ESR组(P< 0.01);斯皮尔曼等级变量相关性分析ALT和AST均与直接冠脉介入治疗术前TIMI血流呈负相关(r=-0.237,P=0.03;r=-0.260,P=0.01);呈偏态分布的自变量先行lg对数转化,建立二元logistic多因素回归分析模型,结果显示急性STEMI患者ALT是IRA-ESR的独立影响因素(OR=0.034,P=0.005);ALT高于55.50 U/L可能是截点值。结论 急性STEMI患者ALT升高是IRA-NSR的预测指标之一。
-
关键词:
- ST段抬高型心肌梗死 /
- 梗死相关动脉 /
- 早期自发再通 /
- 谷丙转氨酶
Abstract: Objective Patients with acute ST segment elevation myocardial infarction (STEMI) often have early spontaneous recanalization (ESR) of infarct related artery (IRA). The purpose of this study was to investigate the correlation of IRA-ESR in patients with acute STEMI.Methods The clinical data of patients with acute STEMI hospitalized in the chest pain center of Mindong Hospital Affiliated to Fujian Medical University from January 1, 2020 to January 31, 2022 were retrospectively analyzed. The 160 eligible patients were divided into ESR group (54 cases) and non spontaneous recanalization (NSR) group (106 cases) according to the ira-timi blood flow classification determined by coronary angiography; The baseline data of the two groups and the levels of aspartate aminotransferase (AST) and alanine aminotransferase (ALT) before emergency percutaneous coronary intervention (PCI) were compared by statistical methods such asχ2-test, independent sample t-test and Mann Whitney U-test; The correlation of AST, ALT and ira-timi blood flow was analyzed by Spearman correlation analysis; Binary logistic regression analysis was used to screen the predictors of ira-esr. We draw the receiver operating characteristic curve (ROC), and evaluate the value of ALT in predicting IRA-ESR.Results ALT and AST in NSR group were significantly higher than those in ESR group(P< 0.01); Spearman rank variable correlation analysis ALT and AST were negatively correlated with TIMI blood flow before direct coronary intervention(r=-0.237,P=0.03;r=-0.260,P=0.01); The independent variables with biased distribution were first LG transformed into logarithm, and a binary logistic multivariate regression model was established. The results showed that ALT was an independent influencing factor of IRA-ESR in patients with acute STEMI(or=0.034,P=0.005); ALT higher than 55.50 U/L may be the cutoff value.Conclusion The elevation of ALT in patients with acute STEMI is one of the predictors of IRA-NSR. -

-
表 1 ESR组与NSR组临床资料比较
Table 1. Comparison of clinical data
例(%), M(P25, P75), X±S 项目 ESR组(54例) NSR组(106例) P 男/女/例 47/7 81/25 0.112 年龄/岁 64.19±12.45 63.67±11.61 0.796 BMI/(kg·m-2) 23.30±2.93 22.90±2.94 0.379 吸烟史 36(66.7) 62(58.5) 0.315 高血压史 26(48.1) 57(53.8) 0.501 糖尿病史 15(27.8) 17(16.0) 0.079 收缩压/mmHg△ 131.98±20.99 126.22±21.82 0.109 舒张压/mmHg 84.04±14.91 79.82±14.80 0.920 心率/(次·min-1) 82.22±14.88 77.64±14.77 0.066 胸痛时间/h 4.0(0.5,72.0) 4.0(0.7,48.0) 0.604 DtoB时间/min 88.48±7.52 86.46±11.80 0.254 △1 mmHg=0.133 kPa。 表 2 2组实验室结果比较
Table 2. Comparison of laboratory results
例(%), M(P25, P75), X±S 项目 ESR组(54例) NSR组(106例) P ALT/(U·L-1) 40.50(6.00,117.00) 57.50(14.00,139.00) 0.007 AST/(U·L-1) 117.00(17.00,686.00) 201.00(16.00,820.00) 0.008 GGT/(U·L-1) 33.00(11.00,325.00) 33.00(4.60,235.00) 0.702 TBIL/(μmol·L-1) 14.30(4.30,39.10) 12.60(4.50,32.50) 0.430 NEUT/(×109·L-1) 10.05(10.70,25.60) 11.00(4.40,113.00) 0.169 HGB/(g·L-1) 143.00(75.00,233.00) 141.00(7.00,177.00) 0.214 LYMPH/(×109·L-1) 1.55(0.40,6.60) 1.40(0.60,27.70) 0.807 MONO/(×109·L-1) 0.70(0.70,1.20) 0.60(0.20,1.80) 0.244 PLT/(×109·L-1) 231.00(95.00,495.00) 244.5(102.00,437.00) 0.302 RDW-SD/fL 41.00(12.00,49.00) 43.00(35.00,53.00) 0.055 CH/(mmol·L-1) 4.80±1.22 4.87±1.11 0.694 TG/(mmol·L-1) 1.64±0.82 2.19±2.86 0.660 HDL-C/(mmol·L-1) 1.09±0.213 1.10±0.237 0.780 LDL-C/(mmol·L-1) 3.01±1.05 3.06±0.92 0.741 ALB/(g·L-1) 38.38±3.66 38.39±3.76 0.993 APOA/(g·L-1) 1.17±0.20 1.18±0.22 0.880 APOB/(g·L-1) 0.97±0.15 0.98±0.24 0.948 GLU/(mmol·L-1) 7.07±2.56 7.10±3.11 0.958 CREA/(μmol·L-1) 75.00(45.00,327.00) 70.00(44.00,176.00) 0.153 GFR/(mL·min-1) 90.96(15.61,112.34) 92.46(11.73,149.34) 0.916 BNP/(pg·mL-1) 109.89(5.00,4923.34) 101.00(5.00,3013.58) 0.358 HbA1c/% 6.37±2.21 6.28±1.93 0.785 LVEDD/mm 49.00±5.10 47.83±4.80 0.836 LVEF/% 58.03±7.37 56.78±7.41 0.312 心室节段运动异常 26(48.1) 57(53.8) 0.509 GGT:谷氨酰转肽酶;TBIL:总胆红素;NEUT:中性粒细胞绝对值;HGB:血红蛋白;LYMPH:淋巴细胞绝对值;MONO:单核细胞绝对值;PLT:血小板计数;RDW-SD:红细胞分布宽度;CH:总胆固醇;TG:甘油三酯;HDL-C:高密度脂蛋白胆固醇;LDL-C:低密度脂蛋白胆固醇;ALB:白蛋白;APOA:载脂蛋白A;APOB:载脂蛋白B;GLU:葡萄糖;CREA:肌酐;GFR:肾小球滤过率;HbA1c:糖化血红蛋白。 表 3 2组ST段抬高部位和梗死相关血管比较
Table 3. Comparison of ST segment elevation and infarct related vessels
例(%) 组别 STEMI心电图抬高部位 梗死相关血管部位 前壁 下壁 高侧壁 后壁 前降支 回旋支 右冠 ESR组(54例) 36(66.7) 17(31.5) 1(1.9) 0(0) 37(68.5) 9(16.7) 8(14.8) NSR组(106例) 51(48.1) 52(49.1) 1(0.9) 2(1.9) 54(50.9) 35(33.0) 17(16.0) χ2 6.082 5.456 P 0.108 0.65 表 4 急性STEMI患者肝酶与IRA-TIMI血流相关分析
Table 4. Correlation analysis
参数 ALT AST 术前 术后 术前 术后 r -0.237 0.040 -0.260 -0.018 P 0.03 0.62 0.01 0.82 表 5 急性STEMI患者IRA-ESR与多因素二元logistic回归分析
Table 5. IRA-ESR and multivariate binary logistic regression analysis
因素 B SE Wald P OR 95%CI 下限 上限 lgALT -3.389 1.201 7.968 0.005 0.034 0.003 0.355 lgAST 0.614 0.747 0.676 0.411 1.848 0.428 7.982 lgGGT 0.119 0.79 0.023 0.881 1.126 0.239 5.298 年龄 0.009 0.022 0.156 0.693 1.009 0.967 1.052 性别 -0.943 0.705 1.789 0.181 0.390 0.098 1.551 BMI 0.04 0.078 0.261 0.610 1.041 0.893 1.212 吸烟 0.143 0.499 0.082 0.775 1.153 0.434 3.065 高血压 -0.271 0.411 0.434 0.510 0.763 0.341 1.708 糖尿病 -0.077 0.522 0.022 0.883 0.926 0.333 2.574 TG -0.224 0.211 1.123 0.289 0.799 0.528 1.210 LDL-C 0.112 0.224 0.251 0.617 1.119 0.721 1.736 HDL-C 0.365 0.953 0.147 0.702 1.440 0.222 9.331 lgRDW -13.659 7.034 3.771 0.052 0 0 1.135 lgHGB 2.114 2.314 0.835 0.361 8.283 0.089 772.348 lgCREA 1.866 1.752 1.135 0.287 6.461 0.209 200.09 lgBNP 0.207 0.319 0.423 0.515 1.230 0.659 2.297 LVEF 0.018 0.034 0.293 0.589 1.019 0.953 1.089 心室节段运动异常 0.132 0.482 0.075 0.784 1.141 0.444 2.937 造影罪犯血管 -0.488 0.289 2.85 0.091 0.614 0.348 1.082 注:模型系数显著性P=0.012(< 0.05),霍斯默-莱梅肖检验P=0.569(>0.05),二元logistic回归模型有统计学意义,模型拟合度良好。 -
[1] Gao M, Cheng Y, Zheng Y, et al. Association of serum transaminases with short-and long-term outcomes in patients with ST-elevation myocardial infarction undergoing primary percutaneous coronary intervention[J]. BMC Cardiovasc Disord, 2017, 17(1): 43. doi: 10.1186/s12872-017-0485-6
[2] Li J, Zhao Z, Jiang H, et al. Predictive value of elevated alanine aminotransferase for in-hospital mortality in patients with acute myocardial infarction[J]. BMC Cardiovasc Disord, 2021, 21(1): 82. doi: 10.1186/s12872-021-01903-z
[3] Bannon L, Merdler I, Bar N, et al. The Cardio-Hepatic Relation in STEMI[J]. J Pers Med, 2021, 11(12).
[4] Wang J, He SY. Clinical and angiographic characteristics of patients with spontaneous reperfusion in ST-segment elevation myocardial infarction[J]. Medicine(Baltimore), 2020, 99(10): 19267-19271.
[5] Kamstrup PR. Lipoprotein(a)and Cardiovascular Disease[J]. Clin Chem, 2021, 67(1): 154-166. doi: 10.1093/clinchem/hvaa247
[6] 齐惠斌, 游向东, 张华, 等. 脂蛋白a与急性心肌梗死患者冠脉侧支循环形成的关系分析[J]. 临床急诊杂志, 2021, 22(12): 829-831. https://www.cnki.com.cn/Article/CJFDTOTAL-ZZLC202112009.htm
[7] 急性ST段抬高型心肌梗死诊断和治疗指南(2019)[J]. 中华心血管病杂志, 2019, 47(10): 766-783.
[8] 汤曾耀, 梅寒颖, 刘继文, 等. 脂蛋白(a)与NLR联合预测老年急性ST段抬高型心肌梗死患者梗死相关动脉自发再通的价值[J]. 中国老年学杂志, 2022, 42(6): 1291-1294. doi: 10.3969/j.issn.1005-9202.2022.06.004
[9] 王顺利, 汤建民, 王丰云, 等. C反应蛋白/白蛋白比值与急性ST段抬高型心肌梗死患者梗死相关动脉自发再通的相关性研究[J]. 中国全科医学, 2020, 23(33): 4167-4171. doi: 10.12114/j.issn.1007-9572.2020.00.500
[10] 龚艳君, 霍勇. 急性ST段抬高型心肌梗死诊断和治疗指南(2019)解读[J]. 中国心血管病研究, 2019, 17(12): 1057-1061. doi: 10.3969/j.issn.1672-5301.2019.12.001
[11] Alrawashdeh A, Nehme Z, Williams B, et al. Impact of emergency medical service delays on time to reperfusion and mortality in STEMI[J]. Open Heart, 2021, 8(1).
[12] Ndrepepa G, Holdenrieder S, Colleran R, et al. Inverse association of alanine aminotransferase within normal range with prognosis in patients with coronary artery disease[J]. Clin Chim Acta, 2019, 496: 55-61. doi: 10.1016/j.cca.2019.06.021
[13] Huang HH, Chen YL, Chen JS, et al. Relationships Among C-Reactive Protein, Alanine Aminotransferase, and Metabolic Syndrome in Apparently Healthy Chinese Subjects[J]. Metab Syndr Relat Disord, 2018, 16(5): 232-239. doi: 10.1089/met.2017.0059
[14] 杜焕民. 成年人群血清肝酶与代谢综合征的相关性研究[D]. 天津: 天津医科大学, 2016.
[15] Di Pino A, DeFronzo RA. Insulin Resistance and Atherosclerosis: Implications for Insulin-Sensitizing Agents[J]. Endocr Rev, 2019, 40(6): 1447-1467.
[16] 鲍微, 徐燕. 血清总胆红素、C反应蛋白及脂蛋白α与高脂血症患者的关系的研究[J]. 临床血液学杂志, 2020, 33(6): 422-424. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXZ202006012.htm
[17] Badimon L, Peña E, Arderiu G, et al. C-Reactive Protein in Atherothrombosis and Angiogenesis[J]. Front Immunol, 2018, 9: 430. doi: 10.3389/fimmu.2018.00430
[18] Tang L, Yuan B, Zhang F, et al. Visceral fat is associated with elevation of serum alanine aminotransferase and gamma glutamyltransferase in middle-aged Chinese adults[J]. Postgrad Med J, 2018, 94(1117): 641-646. doi: 10.1136/postgradmedj-2018-135644
[19] 熊芳, 王宗保, 唐朝克. 富含甘油三酯脂蛋白代谢及其在动脉粥样硬化中的作用[J]. 中国动脉硬化杂志, 2019, 27(1): 81-86. doi: 10.3969/j.issn.1007-3949.2019.01.016
[20] 帕孜丽亚·阿地力, 穆叶赛·尼加提. 动脉粥样硬化与炎症[J]. 临床心血管病杂志, 2020, 36(4): 303-306. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXB202004002.htm
[21] 孙宏鸽, 刘启贵, 王晓蓉, 等. 基于联合模型的谷丙和谷草转氨酶动态变化与代谢综合征的关联研究[J]. 中国卫生统计, 2018, 35(2): 181-185. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGWT201802005.htm
-




 下载:
下载: