Analysis of risk factors for the prognosis of patients with non-ST-segment elevation myocardial infarction and construction and validation of a nomogram
-
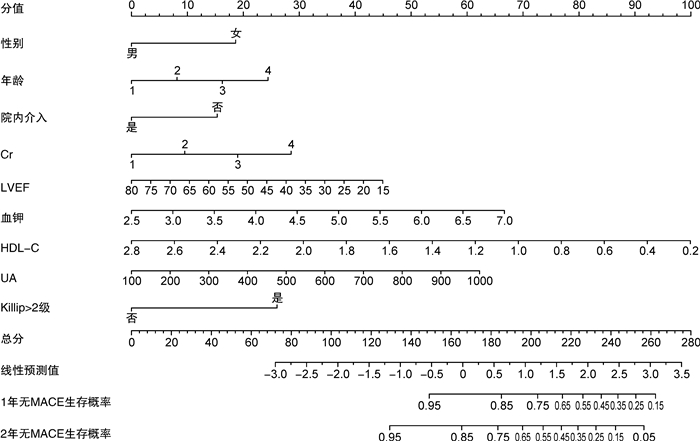
摘要: 目的 构建单中心急性非ST段抬高型心肌梗死(NSTEMI)患者预后评估模型。方法 收集2017年1月—2019年9月入院诊断为NSTEMI的患者497例为研究对象。随访(26.86±11.89)个月,终点为主要不良心血管事件(MACE)。分析NSTEMI患者院外MACE发生的危险因素,构建预测评分系统。结果 将研究人群分为训练集和外部验证集。以终点事件为因变量对训练集人群进行分析,显示性别、年龄、吸烟、Killip>2级、GRACE评分、GRACE评分高危及极高危、袢利尿剂、射血分数、白蛋白、尿酸、磷、血红蛋白、院内介入均为相关影响因素。通过单因素、多因素Cox分析等多种统计学方法得到NSTEMI患者1年、2年无MACE事件发生的9个影响因素,建立相应的列线图(C-index=0.711)。与GRACE评分相比,本预测模型的AUC 1年(0.719 vs.0.736)、2年(0.702 vs.0.743)均较高,C-index同样优于GRACE评分(0.582 vs.0.711)。结论 性别、年龄、院内介入、肌酐、射血分数、血钾、高密度脂蛋白、尿酸、Killip>2级是院外MACE事件的独立影响因素。基于上述9项影响因素,本研究建立的生存预测模型拥有较好的预测效能及一致性。列线图预测模型具有良好的区分度且较GRACE评分预测价值高,可为NSTEMI患者临床决策及预后预测提供个体化的有效预测工具。
-
关键词:
- 急性非ST段抬高型心肌梗死 /
- 预后 /
- 预测列线图
Abstract: Objective To build a single-center prognosis-predicting model of acute non ST-segment elevation myocardial infarction(NSTEMI), Methods A total of 497 patients who were definitely diagnosed with NSTEMI in our hospital from January 2017 to September 2019 were enrolled. The follow-up was(26.86±11.89) months, and the endpoints were major adverse cardiovascular events(MACE). The risk factors of out-of-hospital MACE in NSTEMI patients were analyzed, and a predictive scoring system was built.Results All included patients were divided into the training set and the external validation set. Taking the end-point event as the dependent variable, the analysis of patients in the training set showed that sex, age, smoking, Killip>2, GRACE score, high-risk and extremely high-risk, loop diuretics, ejection fraction, albumin, uric acid, phosphorus, hemoglobin, and in-hospital intervention were all relevant influencing factors. Nine influencing factors of NSTEMI patients without MACE in 1 year and 2 years were screened by univariate and multivariate Cox analysis, and the nomogram was established(C-index=0.711). Compared with GRACE score, the AUC of the nomogram was higher in 1 year(0.719 vs. 0.736) and 2 years(0.702 vs. 0.743), and the C-index was also better than GRACEscore(0.582 vs. 0.711).Conclusion Sex, age, in-hospital interventioni, creatinine, ejection fraction, serum potassium, high density lipoprotein, uric acid, and Killip>2 were independent influencing factors for out-of-hospital MACE. The survival prediction model based on the above nine factors has good prediction efficiency and consistency. The nomogram prediction model has good differentiation and higher prediction value than GRACE score, which can provide an individualized and effective prediction tool for clinical decision-making and prognosis in NSTEMI patients.-
Key words:
- acute non-ST-segment elevation myocardial infarction /
- outcome /
- nomogram
-

-
表 1 训练集与外部验证集特征比较
Table 1. Characteristics of the training set and external validation set
例(%), X±S 项目 训练集(398例) 外部验证集(99例) χ2/t值 P值 SMD值 性别 1.325 0.250 0.128 女 117(29.40) 35(35.35) 男 281(70.60) 64(64.65) 年龄 2.475 0.480 0.175 < 60岁 109(27.39) 30(30.30) 60~79岁 217(54.52) 46(46.46) 80~84岁 47(11.81) 16(16.16) ≥85岁 25(6.28) 7(7.07) 心肌梗死 81(20.35) 21(21.21) 0.036 0.850 0.021 PCI 30(7.54) 6(6.06) 0.257 0.612 0.059 糖尿病 147(36.93) 37(37.37) 0.007 0.935 0.009 慢性肾脏病 30(7.54) 10(10.1) 0.704 0.401 0.090 高脂血症 79(19.85) 21(21.21) 0.092 0.762 0.034 贫血 40(10.05) 12(12.12) 0.363 0.547 0.066 脑血管病 119(29.90) 31(31.31) 0.075 0.784 0.031 吸烟 179(44.97) 40(40.40) 0.672 0.412 0.093 饮酒 108(27.14) 24(24.24) 0.340 0.560 0.066 高血压≥2级 255(64.07) 71(71.72) 2.054 0.152 0.164 心率 0.099 0.343 < 50次/min 2(0.50) 1(1.01) 50~69次/min 127(31.91) 26(26.26) 70~89次/min 175(43.97) 42(42.42) 90~109次/min 60(15.08) 26(26.26) 110~149次/min 31(7.79) 4(4.04) 150~199次/min 3(0.75) 0(0) 收缩压 0.560 0.756 0.085 < 120 mmHg 87(21.86) 20(20.20) 120~139 mmHg 254(63.82) 67(67.68) ≥140 mmHg 57(14.32) 12(12.12) 休克指数 0.61±0.22 0.61±0.16 0.139 0.890 0.017 Killip>2级 25(6.28) 9(9.09) 0.982 0.322 0.106 GRACE评分 137.77±39.53 141.22±40.28 0.774 0.439 0.095 GRACE分级 0.905 0.636 0.107 < 109分 74(18.59) 18(18.18) 109~140分 159(39.95) 35(35.35) >140分 165(41.46) 46(46.46) GRACE评分高危及极高危 167(41.96) 49(49.49) 1.832 0.176 0.152 袢利尿剂 135(33.92) 34(34.34) 0.006 0.937 0.009 噻嗪类 33(8.29) 10(10.10) 0.328 0.567 0.063 LVEF/% 55.42±10.35 53.87±10.54 -1.327 0.185 0.148 ALB 0.628 0.197 ≥35.0 g/L 294(73.87) 78(78.79) 30.0~34.9 g/L 78(19.60) 14(14.14) 25.0~29.9 g/L 23(5.78) 7(7.07) < 25.0 g/L 3(0.75) 0(0) UA/(μmol·L-1) 361.89±109.80 366.10±141.99 0.321 0.749 0.033 Cr 2.777 0.427 0.188 0.40~0.79 mg/dL 82(20.60) 23(23.23) 0.80~1.19 mg/dL 231(58.04) 55(55.56) 1.20~1.59 mg/dL 49(12.31) 16(16.16) ≥1.60 mg/dL 36(9.05) 5(5.05) 血钾/(mmol·L-1) 4.01±0.48 3.99±0.40 -0.253 0.801 0.030 血磷/(mmol·L-1) 1.19±0.29 1.18±0.27 -0.302 0.763 0.034 FPG/(mmol·L-1) 6.83±3.00 6.90±3.05 0.201 0.841 0.022 TC/(mmol·L-1) 4.33±1.27 4.18±1.09 -1.019 0.309 0.119 HDL-C/(mmol·L-1) 1.01±0.28 0.99±0.24 -0.466 0.641 0.055 Hb 0.932 0.628 0.115 ≥120 g/L 281(70.60) 69(69.70) 90~119 g/L 102(25.63) 28(28.28) < 90 g/L 15(3.77) 2(2.02) WBC/(×109·L-1) 8.37±3.24 9.24±3.77 2.297 0.022 0.246 PLT/(×109·L-1) 219.6±60.16 229.93±63.39 1.512 0.131 0.167 NLR 5.22±5.36 5.50±5.80 0.447 0.655 0.049 院内介入 229(57.54) 62(62.63) 0.846 0.35 0.104 院内HF 68(17.09) 14(14.14) 0.499 0.480 0.081 院外MACE 70(17.59) 17(17.17) 0.010 0.922 0.053 随访时间/月 26.60±12.05 25.96±11.86 0.476 0.634 0.053 表 2 训练集中无MACE与MACE组患者基线资料比较
Table 2. Baseline characteristics of non-MACE group and MACE group in the training set
例(%), X±S 项目 无MACE组(328例) MACE组(70例) χ2/t值 P值 SMD值 性别 4.601 0.032 0.275 女 89(27.13) 28(40.00) 男 239(72.87) 42(60.00) 年龄 13.439 0.004 0.439 < 60岁 96(29.27) 13(18.57) 60~79岁 182(55.49) 35(50.00) 80~84岁 35(10.67) 12(17.14) ≥85岁 15(4.57) 10(14.29) 心肌梗死 65(19.82) 16(22.86) 0.329 0.566 0.074 PCI 26(7.93) 4(5.71) 0.405 0.524 0.088 糖尿病 118(35.98) 29(41.43) 0.736 0.391 0.112 慢性肾脏病 25(7.62) 5(7.14) 0.019 0.890 0.018 高脂血症 66(20.12) 13(18.57) 0.087 0.768 0.039 贫血 31(9.45) 9(12.86) 0.740 0.390 0.108 脑血管病 92(28.05) 27(38.57) 3.048 0.081 0.225 吸烟 155(47.26) 24(34.29) 3.922 0.048 0.266 饮酒 93(28.35) 15(21.43) 1.399 0.237 0.161 高血压≥2级 203(61.89) 52(74.29) 3.850 0.050 0.268 心率 0.858 0.188 < 50次/min 2(0.61) 0(0) 50~69次/min 106(32.32) 21(30.00) 70~89次/min 146(44.51) 29(41.43) 90~109次/min 48(14.63) 12(17.14) 110~149次/min 24(7.32) 7(10.00) 150~199次/min 2(0.61) 1(1.43) 收缩压 1.451 0.484 0.155 < 120 mmHg 68(20.73) 19(27.14) 120~139 mmHg 213(64.94) 41(58.57) ≥140 mmHg 47(14.33) 10(14.29) 休克指数 0.60±0.20 0.64±0.30 -0.977 0.331 0.144 Killip>2级 14(4.27) 11(15.71) 12.838 < 0.001 0.389 GRACE评分 135.64±38.40 147.76±43.32 -2.341 0.020 0.288 GRACE分级 4.142 0.126 0.272 < 109分 61(18.60) 13(18.57) 109~140分 138(42.07) 21(30.00) >140分 129(39.33) 36(51.43) GRACE评分高危及极高危 128(39.02) 39(55.71) 6.598 0.010 0.339 袢利尿剂 104(31.71) 31(44.29) 4.072 0.044 0.261 噻嗪类 25(7.62) 8(11.43) 1.099 0.294 0.130 LVEF/% 56.11±10.21 52.19±10.49 2.904 0.004 0.379 ALB 0.004 0.384 ≥35.0 g/L 248(75.61) 46(65.71) 30.0~34.9 g/L 65(19.82) 13(18.57) 25.0~29.9 g/L 14(4.27) 9(12.86) < 25.0 g/L 1(0.30) 2(2.86) UA/(μmol·L-1) 354.93±99.80 394.50±144.40 -2.184 0.032 0.319 Cr 2.010 0.570 0.178 0.40~0.79 mg/dL 69(21.04) 13(18.57) 0.80~1.19 mg/dL 193(58.84) 38(54.29) 1.20~1.59 mg/dL 39(11.89) 10(14.29) ≥1.60 mg/dL 27(8.23) 9(12.86) 血钾/(mmol·L-1) 3.99±0.47 4.10±0.52 -1.789 0.074 0.227 血磷/(mmol·L-1) 1.18±0.27 1.27±0.34 -2.396 0.017 0.292 FPG/(mmol·L-1) 6.80±3.04 7.00±2.84 -0.511 0.610 0.069 TC/(mmol·L-1) 4.37±1.30 4.12±1.11 1.490 0.137 0.206 HDL-C/(mmol·L-1) 1.02±0.28 0.97±0.25 1.312 0.190 0.180 Hb 9.862 0.007 0.379 ≥120 g/L 241(73.48) 40(57.14) 90~119 g/L 78(23.78) 24(34.29) < 90 g/L 9(2.74) 6(8.57) WBC/(×109·L-1) 8.26±3.10 8.88±3.81 -1.261 0.210 0.177 PLT/(×109·L-1) 218.88±57.41 222.97±72.06 -0.446 0.657 0.063 NLR 5.01±5.07 6.22±6.51 -1.713 0.088 0.207 院内介入 201(61.28) 28(40.00) 10.693 0.001 0.436 院内HF 51(15.55) 17(24.29) 3.108 0.078 0.220 表 3 训练集单因素和多因素Cox回归
Table 3. Univariate and multivariate Cox regression analysis of training set
因素 单因素分析 多因素AIC准则 HR(95%CI) P值 HR(95%CI) P值 性别 0.580(0.359~0.936) 0.026 0.553(0.327~0.935) 0.027 年龄 1.618(1.246~2.101) < 0.001 1.293(0.952~1.758) 0.100 Killip>2级 3.520(1.848~6.704) < 0.001 2.277(1.111~4.665) 0.025 LVEF 0.970(0.951~0.990) 0.003 0.978(0.956~1.001) 0.056 UA 1.003(1.001~1.005) 0.003 1.002(1.000~1.004) 0.055 Cr 1.200(0.985~1.415) 0.063 1.344(0.951~1.899) 0.093 血钾 1.515(0.971~2.364) 0.067 1.600(1.002~2.557) 0.049 HDL-C 0.516(0.168~0.864) 0.047 0.293(0.111~0.774) 0.013 院内介入 0.462(0.287~0.746) 0.002 0.612(0.351~1.067) 0.083 表 4 预测模型及GRACE评分的初步评价
Table 4. Preliminary evaluation of Nomogram and GRACE score
时间 项目 指标 训练集 外部验证集 1年 本次预测模型 AUC 0.736 0.744 灵敏度 0.743 0.754 特异度 0.659 0.669 GRACE评分 AUC 0.719 0.732 灵敏度 0.714 0.715 特异度 0.658 0.695 2年 本次预测模型 AUC 0.743 0.733 灵敏度 0.737 0.730 特异度 0.651 0.675 GRACE评分 AUC 0.702 0.701 灵敏度 0.679 0.675 特异度 0.702 0.685 -
[1] 李镒冲, 刘世炜, 曾新颖, 等. 1990~2016年中国及省级行政区心血管病疾病负担报告[J]. 中国循环杂志, 2019, 34(8): 729-740. doi: 10.3969/j.issn.1000-3614.2019.08.001
[2] 马丽媛, 吴亚哲, 陈伟伟. 《中国心血管病报告2018》要点介绍[J]. 中华高血压杂志, 2019, 27(8): 712-716. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGGZ201908007.htm
[3] 《中国心血管病报告2010》概要[J]. 护理管理杂志, 2012, 12(1): 14-15.
[4] 盛兆雪, 刘臣, 周鹏, 等. 急性心肌梗死合并心源性休克患者临床特征和预后变化的单中心结果[J]. 中华医学杂志, 2018, 98(39): 3208-3211. doi: 10.3760/cma.j.issn.0376-2491.2018.39.017
[5] Trantalis G, Aggeli K, Toutouzas K, et al. The prognostic value of CHA2DS2-VASc and GRACE risk scores in patients with ACS[J]. Hellenic J Cardiol, 2019, 60(5): 305-308. doi: 10.1016/j.hjc.2018.03.001
[6] Wilkinson C, Bebb O, Dondo TB, et al. Sex differences in quality indicator attainment for myocardial infarction: a nationwide cohort study[J]. Heart, 2019, 105(7): 516-523. doi: 10.1136/heartjnl-2018-313959
[7] Rodríguez-Padial L, Fernández-Pérez C, Bernal JL, et al. Differences in in-hospital mortality after STEMI versus NSTEMI by sex. Eleven-year trend in the Spanish National Health Service[J]. Rev Esp Cardiol (Engl Ed), 2021, 74(6): 510-517. doi: 10.1016/j.recesp.2020.04.031
[8] Keykhaei M, Ashraf H, Rashedi S, et al. Differences in the 2020 ESC Versus 2015 ESC and 2014 ACC/AHA Guidelines on the Management of Acute Coronary Syndromes in Patients Presenting Without Persistent ST-Segment Elevation[J]. Curr Atheroscler Rep, 2021, 23(12): 77. doi: 10.1007/s11883-021-00976-7
[9] Zhang Q, Zhao D, Xie W, et al. Recent Trends in Hospitalization for Acute Myocardial Infarction in Beijing: Increasing Overall Burden and a Transition From ST-Segment Elevation to Non-ST-Segment Elevation Myocardial Infarction in a Population-Based Study[J]. Medicine (Baltimore), 2016, 95(5): e2677. doi: 10.1097/MD.0000000000002677
[10] Zhao D, Liu J, Wang M, et al. Epidemiology of cardiovascular disease in China: current features and implications[J]. Nat Rev Cardiol, 2019, 16(4): 203-212. doi: 10.1038/s41569-018-0119-4
[11] Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines[J]. Circulation, 2014, 130(25): 2354-2394. doi: 10.1161/CIR.0000000000000133
[12] Sun Y, Feng L, Li X, et al. The sex difference in 6-month MACEs and its explaining variables in acute myocardial infarction survivors: Data from CPACS-3 study[J]. Int J Cardiol, 2020, 311: 1-6. doi: 10.1016/j.ijcard.2020.03.043
[13] Guo W, Du X, Gao Y, et al. Sex Differences in Characteristics, Treatments, and Outcomes Among Patients Hospitalized for Non-ST-Segment-Elevation Myocardial Infarction in China: 2006 to 2015[J]. Circ Cardiovasc Qual Outcomes, 2022, 15(6): e008535.
[14] 畅晓燕, 赵江峰. 经皮冠状动脉介入治疗慢性完全闭塞病变对患者心脏功能的影响[J]. 临床心血管病杂志, 2021, 37(3): 220-223. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXB202103007.htm
[15] Collet JP, Thiele H, Barbato E, et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation[J]. Eur Heart J, 2021, 42(14): 1289-1367. doi: 10.1093/eurheartj/ehaa575
[16] 侯宪庚, 谢翔, 杨毅, 等. 药物治疗和介入治疗对急性非ST段抬高型心肌梗死长期预后的影响[J]. 新疆医科大学学报, 2019, 42(3): 282-287. https://www.cnki.com.cn/Article/CJFDTOTAL-XJYY201903002.htm
[17] 苟春丽, 刘永铭, 薛丽丽, 等. 射血分数中间型心力衰竭患者的临床特征及心脏结构功能变化[J]. 临床心血管病杂志, 2021, 37(6): 541-546. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXB202106010.htm
[18] Hanada K, Sasaki S, Seno M, et al. Reduced Left Ventricular Ejection Fraction Is a Risk for Sudden Cardiac Death in the Early Period After Hospital Discharge in Patients With Acute Myocardial Infarction[J]. Circ J, 2022, 86(10): 1490-1498. doi: 10.1253/circj.CJ-21-0999
[19] Jiang Y, Boris AF, Zhu Y, et al. Incidence, Clinical Characteristics and Short-Term Prognosis in Patients With Cardiogenic Shock and Various Left Ventricular Ejection Fractions After Acute Myocardial Infarction[J]. Am J Cardiol, 2022, 167: 20-26. doi: 10.1016/j.amjcard.2021.11.040
[20] Berg DD, Odonoghue ML, Guo J, et al. Abstract 14083: Prognostic Significance of Left Ventricular Systolic Dysfunction at the Time of NSTEMI in Patients With No Prior History of Heart Failure[J]. Circulation, 2019, 140(Suppl_1 Suppl 1).
[21] 刘叶红, 靳天慧, 陈亮, 等. 血清甲状旁腺激素/HDL-C及LDL-C/HDL-C与冠状动脉病变严重程度的相关性[J]. 临床心血管病杂志, 2020, 36(11): 985-990. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXB202011004.htm
[22] 郭明秋, 殷晓捷, 刁殿琰, 等. 脂质代谢水平与冠状动脉粥样硬化病变的关系[J]. 中国动脉硬化杂志, 2021, 29(2): 149-155. https://www.cnki.com.cn/Article/CJFDTOTAL-KDYZ202102010.htm
[23] Lai J, Akindavyi G, Fu Q, et al. Research Progress on the Relationship between Coronary Artery Calcification and Chronic Renal Failure[J]. Chin Med J(Engl), 2018, 131(5): 608-614.
[24] Funatsu A, Kobayashi T, Mizobuchi M, et al. Clinical and angiographic outcomes of coronary dissection after paclitaxel-coated balloon angioplasty for small vessel coronary artery disease[J]. Cardiovasc Interv Ther, 2019, 34(4): 317-324.
[25] Dod R, Rajendran A, Kathrotia M, et al. Cardiovascular Disease in South Asian Immigrants: a Review of Dysfunctional HDL as a Potential Marker[J]. J Racial Ethn Health Disparities, 2022.
[26] Lappegård KT, Kjellmo CA, Hovland A. High-Density Lipoprotein Subfractions: Much Ado about Nothing or Clinically Important?[J]. Biomedicines, 2021, 9(7): 836..
[27] 郎勇, 冉迅, 屈模英. 单核细胞高密度脂蛋白比值、血清尿酸水平与冠心病患者冠脉狭窄程度的相关性[J]. 分子诊断与治疗杂志, 2020, 12(9): 1184-1186, 1191. https://www.cnki.com.cn/Article/CJFDTOTAL-YXYQ202009014.htm
[28] 徐萃, 刘宏斌, 王娟, 等. 血清尿酸水平与冠心病患者远期预后的分析[J]. 解放军医学院学报, 2018, 39(2): 102-105, 109. https://www.cnki.com.cn/Article/CJFDTOTAL-JYJX201802004.htm
[29] Yu W, Cheng JD. Uric Acid and Cardiovascular Disease: An Update From Molecular Mechanism to Clinical Perspective[J]. Front Pharmacol, 2020, 11: 582680.
[30] Pavlusova M, Jarkovsky J, Benesova K, et al. Hyperuricemia treatment in acute heart failure patients does not improve their long-term prognosis: A propensity score matched analysis from the AHEAD registry[J]. Clin Cardiol, 2019, 42(8): 720-727.
[31] Stamp LK, Frampton C, Drake J, et al. Associations of Gout and Baseline Serum Urate Level With Cardiovascular Outcomes: Analysis of the Coronary Disease Cohort Study[J]. Arthritis Rheumatol, 2019, 71(10): 1733-1738.
[32] Carnicelli AP, Clare R, Chiswell K, et al. Comparison of Characteristics and Outcomes of Patients With Heart Failure With Preserved Ejection Fraction With Versus Without Hyperuricemia or Gout[J]. Am J Cardiol, 2020, 127: 64-72.
[33] 伏蕊, 窦克非, 许海燕, 等. 中国非ST段抬高型心肌梗死患者随访24个月期间死亡的独立危险因素分析[J]. 中国循环杂志, 2020, 35(10): 985-989. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGXH202010008.htm
-




 下载:
下载: