Risk factors and predictive value of acute respiratory distress syndrome after cardiac surgery under cardiopulmonary bypass
-
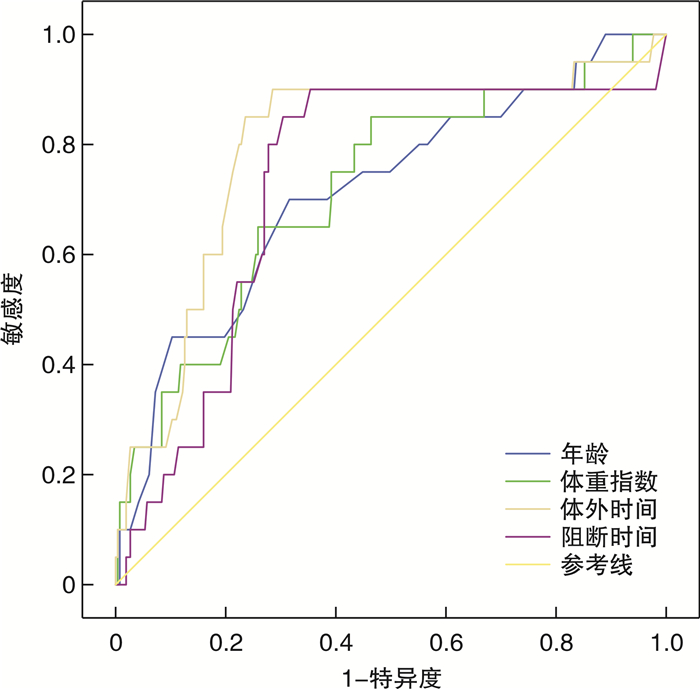
摘要: 目的 分析体外循环下心脏术后急性呼吸窘迫综合征(acute respiratory distress syndrome,ARDS)发生的危险因素及其预测价值。方法 选取2016年11月—2020年12月承德医学院附属医院行体外循环下心脏手术患者283例,依据术后是否发生ARDS分为ARDS组和非ARDS组,统计2组患者临床资料,采用多因素logistic回归分析探讨体外循环下心脏术后ARDS的危险因素,采用ROC曲线分析危险因素对ARDS的预测价值。结果 单因素logistic回归分析结果显示:年龄、体重指数、脑梗死、心功能等级、置换生物瓣、急行体外循环、体外循环时长、主动脉阻断时长、二次开胸与术后ARDS相关(P < 0.05)。多因素logistic回归分析显示年龄、体重指数、体外循环时长、主动脉阻断时长、心功能(NYHA分级)、二次开胸为术后ARDS发生的独立危险因素。ROC曲线分析ARDS发生效果最好的是体外循环时长(截断值为110.5 min,曲线下面积为0.794);其次是主动脉阻断时长;再次为体重指数。结论 年龄>60.5岁、体重指数>24.4 kg/m2、体外循环时间>110.5 min、主动脉阻断时间>74.5 min对体外循环下心脏术后发生ARDS有预测价值,多因素联合分析显示年龄+体重指数+体外时长预测敏感度达90%。Abstract: Objective To analyze the risk factors and predictive value of acute respiratory distress syndrome(ARDS) after cardiac surgery under cardiopulmonary bypass.Methods Two hundred and eighty-three patients who underwent cardiac surgery under cardiopulmonary bypass from November 2016 to December 2020 at the Affiliated Hospital of Chengde Medical College were divided into an ARDS group and a non ARDS group according to the occurrence of ARDS after the operation. The clinical data of the two groups were statistically analyzed. The risk factors of ARDS after cardiac surgery under cardiopulmonary bypass were analyzed by multivariate logistic regression analysis. The predictive value of risk factors for ARDS was analyzed by ROC curve.Results Univariate logistic regression analysis showed that age, body mass index, cerebral infarction, cardiac function grade, replacement of biological valve, urgent cardiopulmonary bypass, cardiopulmonary bypass time, aortic clamp time, and secondary thoracotomy were associated with postoperative ARDS (P < 0.05). Multivariate logistic regression analysis showed that age, body mass index, cardiopulmonary bypass time, aortic clamp time, cardiac function (NYHA grade) and secondary thoracotomy were independent risk factors for the occurrence of postoperative ARDS. ROC curve analysis showed that the best effect of ARDS was the cardiopulmonary bypass time (the cut-off value was 110.5 min, and the area under the curve was 0.794); The second is aortic clamp time; Body mass index.Conclusion Age>60.5 years old, body mass index>24.4 kg/m2, cardiopulmonary bypass time>110.5 min, aortic clamp time>74.5 min and secondary thoracotomy had predictive value for ARDS after cardiac surgery under cardiopulmonary bypass. The combined prediction of multiple factors showed that the sensitivity of age + body mass index + in vitro duration was 90%.
-

-
表 1 2组患者围术期临床资料分析结果
Table 1. The results of perioperative clinical data of two groups of patients
例(%), X±S 临床资料 ARDS组(20例) 非ARDS组(263例) t/χ2 P值 年龄 9.535 0.002 < 65岁 11(55.0) 223(84.8) ≥65岁 9(45.0) 40(15.2) 性别 0.460 0.831 男 10(50.0) 125(47.5) 女 10(50.0) 138(52.5) 体重指数 6.970 0.009 < 24 kg/m2 7(35.0) 170(64.6) ≥24 kg/m2 13(65.0) 93(35.4) 脑梗死 4.765 0.041 是 6(30.0) 33(12.5) 否 14(70.0) 230(87.5) 糖尿病 0.119 0.730 是 3(15.0) 26(9.9) 否 17(85.0) 237(90.1) 吸烟史 1.020 0.313 是 12(60.0) 127(48.3) 否 8(40.0) 136(51.7) COPD 0.067 0.796 是 1(5.0) 4(1.5) 否 19(95.0) 259(98.5) 术前房颤 2.226 0.136 是 4(20.0) 25(9.5) 否 16(80.0) 238(90.5) 心功能等级(NYHA分级) 21.794 < 0.001 Ⅱ级 3(15.0) 54(20.5) Ⅲ级 14(70.0) 207(78.7) Ⅳ级 3(15.0) 2(0.8) 肺动脉高压 0.138 0.711 是 2(10.0) 14(5.3) 否 18(90.0) 249(94.7) 同期行迷宫射频消融术 0.032 0.857 是 0 9(3.4) 否 20(100.0) 254(96.6) 置换生物瓣 4.076 0.044 是 2(10.0) 3(1.1) 否 18(90.0) 260(98.9) CPB时长/min 134.00±30.57 100.53±28.47 -5.042 < 0.001 主动脉阻断时长/min 83.85±32.66 68.04±26.19 -2.555 0.011 急行CPB 6.439 0.011 是 2(10.0) 4(1.5) 否 18(90.0) 259(98.5) 二次开胸 11.173 0.001 是 3(15.0) 3(1.1) 否 17(85.0) 260(98.9) 表 2 临床资料数据处理分类
Table 2. Classification of clinical data
变量 编号 变量赋值 性别 X1 1=男,2=女 年龄 X2 1=18~64岁,2=65~76岁 吸烟 X3 0=不吸或者戒烟,1=吸烟 COPD X4 0=否,1=是 房颤 X5 0=否,1=是 肺动脉高压 X6 0=否,1=是 脑梗死 X7 0=否,1=是 糖尿病 X8 0=否,1=是 心功能(NYHA分级) X9 1=Ⅰ级,2=Ⅱ级,3=Ⅲ级,4=Ⅳ级 急转体外 X10 0=否,1=是 射频消融 X11 0=否,1=是 生物瓣膜 X12 0=否,1=是 二次开胸 X13 0=否,1=是 ARDS Y 1=非ARDS组,2=ARDS组 表 3 2组患者围术期临床资料单因素logistic回归分析结果
Table 3. The results of univariate logistic regression analysis on perioperative clinical data of two groups of patients
临床资料 β P值 OR 95%CI 年龄 0.099 0.003 1.105 (1.034,1.180) 体重指数 0.505 0.001 1.657 (1.241,2.214) 吸烟 0.474 0.316 1.606 (0.636,4.058) COPD 1.226 0.283 3.408 (0.363,32.020) 房颤 0.867 0.147 2.380 (0.738,7.673) 肺动脉高压 0.681 0.391 1.976 (0.417,9.375) 脑梗死 1.094 0.036 2.987 (1.073,8.313) 糖尿病 0.475 0.471 1.609 (0.442,5.858) 心功能(NYHA分级) 3.296 0.002 27.000 (3.197,228.052) 急转体外 1.973 0.028 7.194 (1.234,41.957) CPB时长 0.036 < 0.001 1.037 (1.020,1.054) 主动脉阻断时长 0.022 0.012 1.022 (1.005,1.040) 射频消融 -18.661 0.999 0 (0,0) 生物瓣 2.265 0.017 9.630 (1.511,61.357) 二次开胸 2.727 < 0.001 15.294 (2.868,81.557) 表 4 2组患者围术期临床资料多因素logistic回归分析有意义结果
Table 4. The significant results of multivariate logistic regression analysis on perioperative clinical data of two groups of patients
临床资料 β P值 OR 95%CI 年龄 2.306 0.001 10.033 (2.496,40.321) 体重指数 0.542 0.005 1.720 (1.179,2.511) 心功能(NYHA分级) 3.761 0.004 42.972 (3.288,561.650) CPB时长 0.109 < 0.001 1.115 (1.063,1.170) 主动脉阻断时长 -0.092 0.001 0.912 (0.864,0.962) 二次开胸 4.427 0.003 83.081 (4.683,1495.430) 表 5 单因素预测CPB下心脏手术后发生ARDS的ROC曲线分析
Table 5. ROC curve analysis of single factor in predicting ARDS after cardiac surgery under CPB
变量 截断值 敏感度 特异度 约登指数 AUC及95%CI Z P值 年龄 60.5岁 0.700 0.684 0.384 0.713(0.590~0.837) -3.186 0.001 体重指数 24.4 kg/m2 0.650 0.741 0.391 0.717(0.595~0.840) -3.242 0.001 CPB时长 110.5 min 0.900 0.715 0.615 0.794(0.682~0.906) -4.387 < 0.001 主动脉阻断时长 74.5 min 0.850 0.696 0.546 0.728(0.610~0.846) -3.401 0.001 表 6 多因素联合预测CPB下心脏手术后发生ARDS的ROC曲线分析
Table 6. ROC curve analysis of multi-factor in predicting ARDS after cardiac surgery under CPB
变量 敏感度 特异度 约登指数 AUC及95%CI Z值 P值 年龄+体重指数 0.750 0.669 0.421 0.800(0.710~0.889) -4.289 < 0.001 年龄+体外时长 0.850 0.764 0.377 0.854(0.764~0.943) -3.634 < 0.001 年龄+阻断时长 0.650 0.684 0.353 0.785(0.670~0.900) -5.612 < 0.001 年龄+二次开胸 0.550 0.614 0.465 0.793(0.697~0.888) -4.012 < 0.001 体重指数+体外时长 0.850 0.627 0.579 0.812(0.707~0.917) -3.221 < 0.001 体重指数+阻断时长 0.500 0.549 0.629 0.737(0.610~0.865) -4.505 < 0.001 体重指数+二次开胸 0.600 0.588 0.378 0.763(0.642~0.884) -4.228 < 0.001 年龄+体重指数+体外时长 0.900 0.769 0.553 0.869(0.787~0.951) -4.332 < 0.001 年龄+体重指数+阻断时长 0.700 0.639 0.732 0.814(0.713~0.914) -3.523 < 0.001 年龄+体重指数+二次开胸 0.800 0.730 0.389 0.867(0.797~0.937) -3.687 < 0.001 体外时长+急转体外 0.850 0.772 0.642 0.866(0.816~0.915) -4.786 < 0.001 -
[1] 于洪波, 马大实, 王宝刚, 等. 胰石蛋白与体外循环心脏手术后患者早期感染的关系[J]. 实用医学杂志, 2019, 35(7): 1106-1109, 1115. https://www.cnki.com.cn/Article/CJFDTOTAL-SYYZ201907021.htm
[2] Song J, Yao L, Zhao L, et al. Changes in the concentrations of mediators in exhaled breath condensate during cardiac valve replacement under cardiopulmonary bypass and their relations with postoperative acute respiratory distress syndrome[J]. Medicine(Baltimore), 2020, 99(21): e20007.
[3] Fan E, Brodie D, Slutsky AS. Acute Respiratory Distress Syndrome: Advances in Diagnosis and Treatment[J]. JAMA, 2018, 319(7): 698-710. doi: 10.1001/jama.2017.21907
[4] Banavasi H, Nguyen P, Osman H, et al. Management of ARDS-What Works and What Does Not[J]. Am J Med Sci, 2021, 362(1): 13-23. doi: 10.1016/j.amjms.2020.12.019
[5] Tran MC, Crockett DC, Formenti F, et al. Lungheterogeneity and dead space volume in animals with acute respiratory distress syndrome using the inspired sinewave test[J]. Physiol Meas, 2020, 41(11): 10.
[6] Alghetaa H, Mohammed A, Zhou J, et al. Resveratrol-mediated attenuation of superantigen-driven acute respiratory distress syndrome is mediated by microbiota in the lungs and gut[J]. Pharmacol Res, 2021, 167: 105548. doi: 10.1016/j.phrs.2021.105548
[7] Yao MY, Zhang WH, Ma WT, et al. Long non-coding RNA MALAT1 exacerbates acute respiratory distress syndrome by upregulating ICAM-1 expression via microRNA-150-5p downregulation[J]. Aging(Albany NY), 2020, 12(8): 6570-6585.
[8] Wilson JG, Simpson LJ, Ferreira AM, et al. Cytokine profile in plasma of severe COVID-19 does not differ from ARDS and sepsis[J]. JCI Insight, 2020, 5(17): e140289. doi: 10.1172/jci.insight.140289
[9] Batah SS, Fabro AT. Pulmonary pathology of ARDS in COVID-19: A pathological review for clinicians[J]. Respir Med, 2021, 176: 106239. doi: 10.1016/j.rmed.2020.106239
[10] 兀瑞俭, 詹晓娟, 郭发瑞, 等. 俯卧位通气联合气道压力释放通气模式对中重度急性呼吸窘迫综合征患者的疗效观察[J]. 临床急诊杂志, 2021, 22(10): 667-672. doi: 10.13201/j.issn.1009-5918.2021.10.006
[11] Cheng ZB, Chen H. Higher incidence of acute respiratory distress syndrome in cardiac surgical patients with elevated serum procalcitonin concentration: a prospective cohort study[J]. Eur J Med Res, 2020, 25(1): 11. doi: 10.1186/s40001-020-00409-2
[12] 谢泸兰, 吴西强, 刘建, 等. 呼吸功能锻炼器在老年体外循环心脏手术患者围术期中的应用[J]. 中国体外循环杂志, 2022, 20(2): 103-106. doi: 10.13498/j.cnki.chin.j.ecc.2022.02.10
[13] Lagier D, Velly LJ, Guinard B, et al. Perioperative open-lung approach, regional ventilation, and lung injury in cardiac surgery[J]. Anesthesiology, 2020, 133(5): 1029-1045. doi: 10.1097/ALN.0000000000003539
[14] Bellani G, Pham T, Laffey JG. Missed or delayed diagnosis of ARDS: a common and serious problem[J]. Intensive Care Med, 2020, 46(6): 1180-1183. doi: 10.1007/s00134-020-06035-0
[15] Wu C, Chen X, Cai Y, et al. Risk Factors Associated With Acute Respiratory Distress Syndrome and Death in Patients With Coronavirus Disease 2019 Pneumonia in Wuhan, China[J]. JAMA Intern Med, 2020, 180(7): 934-943. doi: 10.1001/jamainternmed.2020.0994
[16] Schwede M, Lee RY, Zhuo H, et al. Clinician Recognition of the Acute Respiratory Distress Syndrome: Risk Factors for Under-Recognition and Trends Over Time[J]. Crit Care Med, 2020, 48(6): 830-837. doi: 10.1097/CCM.0000000000004328
[17] Sasannejad C, Ely EW, Lahiri S. Long-term cognitive impairment after acute respiratory distress syndrome: a review of clinical impact and pathophysiological mechanisms[J]. Crit Care, 2019, 23(1): 352. doi: 10.1186/s13054-019-2626-z
[18] Ying J, Zhou D, Gu T, et al. Endocan, a Risk Factor for Developing Acute Respiratory Distress Syndrome among Severe Pneumonia Patients[J]. Can Respir J, 2019, 2019: 2476845.
[19] Boiron L, Hopper K, Borchers A. Risk factors, characteristics, and outcomes of acute respiratory distress syndrome in dogs and cats: 54 cases[J]. J Vet Emerg Crit Care(San Antonio), 2019, 29(2): 173-179. doi: 10.1111/vec.12819
[20] Xiao CH, Wan J, Liu H, et al. Red blood cell distribution width is an independent risk factor in the prediction of acute respiratory distress syndrome after severe burns[J]. Burns, 2019, 45(5): 1158-1163. doi: 10.1016/j.burns.2019.01.006
[21] 胡岳秀, 苏云艳, 王哲芸, 等. 肥胖合并A型主动脉夹层患者术后急性肺损伤的肺康复护理[J]. 护士进修杂, 2022, 37(10): 943-946. https://www.cnki.com.cn/Article/CJFDTOTAL-FSJX202210016.htm
[22] Mali S, Haghaninejad H. Pulmonary complications following cardiac surgery[J]. Arch Med Sci Atheroscler Dis, 2019, 4: e280-e285. doi: 10.5114/amsad.2019.91432
[23] Lackner I, Weber B, Baur M, et al. Complement Activation and Organ Damage After Trauma-Differential Immune Response Based on Surgical Treatment Strategy[J]. Front Immunol, 2020, 11: 64. doi: 10.3389/fimmu.2020.00064
[24] 周任, 杨迪成, 施盛, 等. 瓣膜置换手术的非贫血患者术中异体血输注的影响因素分析[J]. 临床心血管病杂志, 2021, 37(4): 351-355. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXB202104012.htm
[25] 胡嫒, 陈唯韫, 黄宇光. 输血相关急性肺损伤发病机制及防治措施研究进展[J]. 中国医学科学院学报, 2020, 42(5): 674-680. https://www.cnki.com.cn/Article/CJFDTOTAL-ZYKX202005018.htm
[26] Semple JW, Rebetz J, Kapur R. Transfusion-associated circulatory overload and transfusion-related acute lung injury[J]. Blood, 2019, 133(17): 1840-1853. doi: 10.1182/blood-2018-10-860809
[27] 温姝钰, 乔韡华, 董念国. 加速康复外科在心脏大血管外科的应用及展望[J]. 临床心血管病杂志, 2021, 37(9): 787-790. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXB202109002.htm
-




 下载:
下载:
