Correlation between serum albumin-globulin ratio and short-term prognosis in patients with chronic heart failure
-
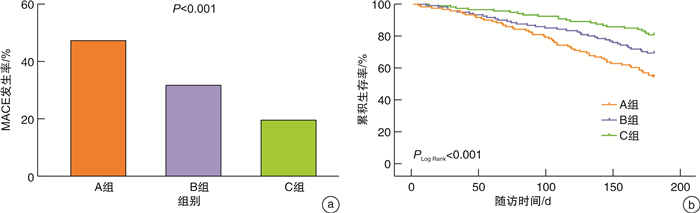
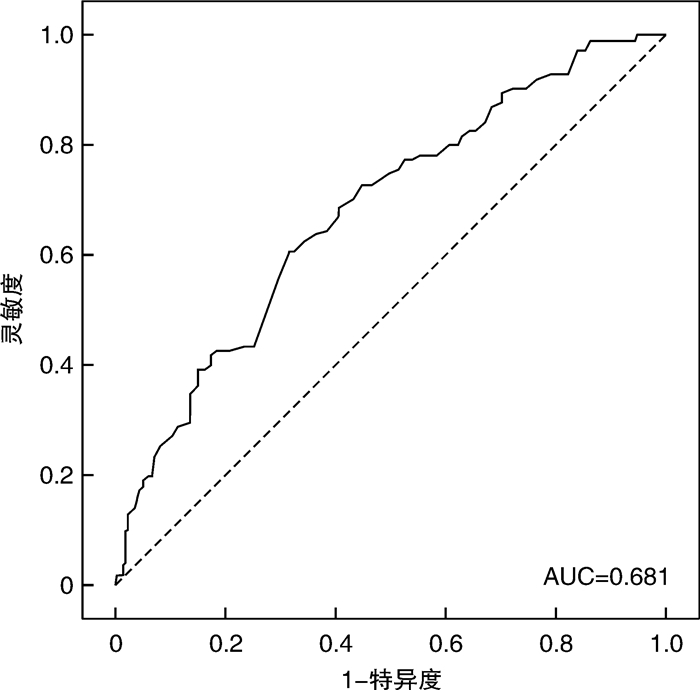
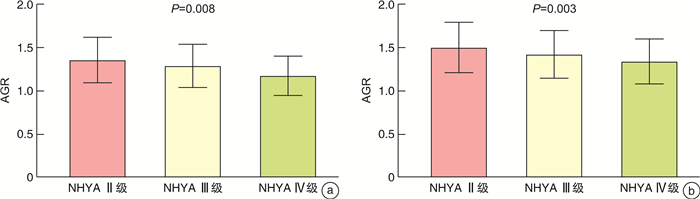
摘要: 目的 探索白蛋白及球蛋白比值(AGR)与慢性心力衰竭(心衰)患者近期内发生主要不良心血管事件(MACE)的相关性。方法 选取2021年3月—2022年3月河北省人民医院心血管内科住院的心衰患者362例,随访出院后6个月内是否发生MACE,分为MACE组115例和非MACE组247例。对MACE组与非MACE组临床资料进行统计分析。采用Log Rank检验分析不同AGR分组MACE累积生存率的差异。采用Cox比例风险回归模型分析MACE的风险因素。采用ROC曲线评估AGR对MACE的预测价值。结果 基线资料分析,与非MACE组比较,MACE组AGR水平明显低于非MACE组,差异有统计学意义[1.24(1.09,1.39) vs 1.39(1.23,1.59),P < 0.001]。AGR与心衰严重程度相关性分析中,整体心衰人群、MACE组及非MACE组分别发现AGR水平随着NHYA心功能分级的增加而降低,差异分别有统计学意义[P < 0.001,P=0.008,P=0.003]。Log Rank检验中,AGR低水平组MACE累积生存率明显低于高水平组(Wald χ2=19.593,PLog Rank < 0.001)。多因素Cox回归分析显示,AGR、尿酸、糖尿病、心房颤动是慢性心力衰竭患者近期MACE的独立预测因素[HR=0.171,95%CI(0.063~0.460),P < 0.001;HR=1.003,95%CI(1.001~1.004),P=0.001;HR=1.75,95%CI(1.189~2.575),P=0.005;HR=1.821,95%CI(1.222~2.715),P=0.003]。ROC曲线分析中,AGR诊断MACE的ROC曲线下面积为0.681[95%CI(0.623~0.740),P < 0.001],灵敏度及特异度分别为60.9%和68.8%。结论 AGR与慢性心衰患者近期预后相关,是慢性心衰近期MACE发生率的独立危险因素,对近期发生MACE有一定的预测价值。Abstract: Objective To investigate the correlation between albumin to globulin ratio(AGR) and recent major adverse cardiovascular events(MACE) in patients with chronic heart failure.Methods A total of 362 patients with heart failure admitted to the Department of Cardiovascular Medicine, Hebei General Hospital from March 2021 to March 2022 were selected to follow up whether they developed MACE within 6 months after discharge. They were divided into two groups, 115 patients in the MACE group and 247 patients in the non-MACE group. The clinical data of MACE group and non-MACE group were analyzed statistically. Log Rank test was used to analyze the difference of MACE cumulative survival in different AGR groups. Cox proportional hazard regression model was used to analyze the risk factors of MACE. The predictive value of AGR to MACE was evaluated by ROC curve.Results Based on baseline data analysis, AGR level in the MACE group was significantly lower than that in the non-MACE group, and the difference was statistically significant[1.24(1.09, 1.39) vs 1.39(1.23, 1.59), P < 0.001]. In the analysis of the correlation between AGR and severity of heart failure, it was found that the level of AGR decreased with the increase of NHYA cardiac function classification in the overall heart failure population, MACE group and non-MACE group, respectively, and the difference was statistically significant(P < 0.001, P=0.008, P=0.003). In Log Rank test, the MACE cumulative survival rate of the low AGR group was significantly lower than that of the high AGR group(Wald χ2=19.593, PLog Rank=P < 0.001). Multi-factor Cox regression analysis showed that AGR, uric acid, Diabetes Mellitus and Atrial Fibrillation were independent predictors of recent MACE in patients with chronic heart failure[HR=0.171, 95%CI(0.063-0.460), P < 0.001; HR=1.003, 95%CI(1.001-1.004), P=0.001; HR=1.75, 95%CI(1.189-2.575), P=0.005; HR=1.821, 95%CI(1.222-2.715), P=0.003]. In ROC curve analysis, the area under ROC curve for AGR diagnosis of MACE was 0.681[95%CI(0.623-0.740), P < 0.001], and the sensitivity and specificity were 60.9% and 68.8%, respectively.Conclusion AGR is associated with the short-term prognosis of patients with chronic heart failure, it is an independent risk factor for the recent incidence of MACE in chronic heart failure and has a certain value in predicting the recent occurrence of MACE.
-
Key words:
- heart failure /
- albumin /
- globulin /
- albumin to globulin ratio /
- prognosis
-

-
表 1 MACE组与非MACE组临床资料比较
Table 1. Comparison of clinical data between MACE group and non-MACE group
例(%), X±S, M(P25, P75) 项目 整体人群(362例) 非MACE组(247例) MACE组(115例) t/Z/χ2 P 男性 234(64.6) 166(67.2) 68(59.1) 2.239 0.135 年龄/岁 69.78±11.19 68.28±10.82 73.00±11.31 3.808 < 0.001 BMI/(kg/m2) 25.39(22.89,27.92) 25.61(23.00,28.05) 24.80(22.19,27.68) 0.809 0.418 收缩压/mmHg 131(114,152) 132(116,152) 129(112,145) 1.328 0.184 舒张压/mmHg 78(69,88) 79(70,89) 75(66,85) 2.498 0.012 心率/(次/min) 84(70,98) 84(72,98) 81(69,96) 1.415 0.157 NYHA Ⅲ/Ⅳ级 306(84.5) 207(83.8) 99(86.1) 0.312 0.576 冠心病 232(64.1) 152(61.5) 80(69.6) 2.197 0.138 高血压 228(64.1) 149(60.3) 79(68.7) 2.359 0.125 糖尿病 149(41.2) 88(35.6) 61(53.0) 9.827 0.002 心房颤动 136(37.6) 80(32.4) 56(48.7) 8.896 0.003 吸烟史 79(21.8) 46(18.6) 33(28.7) 4.666 0.031 饮酒史 40(11.0) 24(9.7) 16(13.9) 1.406 0.236 袢利尿剂 284(78.5) 198(80.2) 86(74.8) 1.343 0.246 醛固酮受体拮抗剂 291(80.4) 204(82.6) 87(75.7) 2.396 0.122 ACEI/ARB 44(12.2) 29(11.7) 15(13.0) 0.125 0.724 β-受体阻滞剂 255(70.4) 180(72.9) 75(65.2) 2.21 0.137 ANRI 189(52.2) 135(54.7) 54(47.0) 1.864 0.172 SGLT-2抑制剂 77(21.3) 52(21.1) 25(21.7) 0.022 0.882 LVEF/% 44(34,57) 41(34,56) 47(37,59) 2.172 0.030 NT-proBNP/(ng/L) 2 993(1 094,7 792) 2 704(1 123,7 081) 3 799(1 063,8 835) 1.381 0.167 CRP/(mg/L) 6.32(3.27,14.12) 5.39(2.65,12.01) 9.75(4.34,19.29) 3.378 0.001 WBC/(×109/L) 7.16(5.69,9.05) 7.35(5.82,9.01) 6.80(5.40,9.04) 0.953 0.341 Hb/(g/L) 128(113,139) 130(116,141) 122(104,135) 3.537 < 0.001 淋巴细胞计数/(×109/L) 1.36(0.96,1.86) 1.42(1.01,1.87) 1.20(0.89,1.78) 1.625 0.104 总蛋白/(g/L) 64.28±7.06 64.45±6.64 63.90±7.90 0.692 0.489 白蛋白/(g/L) 36.62±4.74 37.36±4.37 35.04±5.13 4.432 < 0.001 总胆红素/(μmol/L) 16.15(12.58,24.53) 16.00(13.10,24.10) 16.60(11.65,25.80) 0.045 0.964 空腹血糖/(mmol/L) 5.77(5.06,7.83) 5.60(5.03,7.46) 6.25(5.15,8.39) 1.685 0.092 TC/(mmol/L) 3.68(3.10,4.44) 3.73(3.16,4.42) 3.54(3.02,4.61) 1.391 0.164 LDL-C /(mmol/L) 2.28(1.81,2.92) 2.31(1.85,2.91) 2.18(1.68,2.91) 1.371 0.170 肌酐/(μmol/L) 85.80(71.10,112.63) 84.20(71.70,109.85) 93.80(69.80,120.50) 1.045 0.296 尿酸/(μmol/L) 400.35(315.30,481.53) 388.40(311.80,473.95) 421.20(329.25,506.25) 2.172 0.030 eGFR/(mL/min/1.73m2) 71.57(53.81,86.06) 72.90(57.74,87.69) 66.88(47.01,82.76) 2.513 0.012 AGR 1.35(1.17,1.53) 1.39(1.23,1.59) 1.24(1.09,1.39) 5.559 < 0.001 注:1 mmHg=0.133 kPa。 表 2 CHF患者近期发生MACE的单因素和多因素Cox比例风险回归分析
Table 2. Univariate and multivariate Cox proportional risk regression analysis of recent MACE in CHF patients
项目 单因素Cox分析 多因素Cox分析 P值 HR 95%CI P值 HR 95%CI 性别 0.141 1.322 0.912~1.918 0.264 0.775 0.495~1.212 年龄 < 0.001 1.033 1.016~1.051 0.178 1.013 0.994~1.033 舒张压 0.007 0.983 0.971~0.995 0.112 0.989 0.975~1.003 吸烟史 0.023 1.600 1.068~2.396 0.224 1.364 0.828~2.247 冠心病 0.115 1.377 0.925~2.048 0.695 1.094 0.698~1.713 高血压 0.111 1.378 0.929~2.043 0.172 1.350 0.877~2.079 糖尿病 0.001 1.854 1.285~2.674 0.005 1.750 1.189~2.575 心房颤动 0.003 1.730 1.200~2.495 0.003 1.821 1.222~2.715 eGFR 0.007 0.987 0.978~0.997 0.790 0.999 0.988~1.009 尿酸 0.016 1.568 1.087~2.261 0.001 1.003 1.001~1.004 NT-proBNP 0.055 1.000 1.000~1.000 0.691 1.000 1.000~1.000 CRP 0.002 1.011 1.004~1.018 0.529 1.002 0.995~1.010 白蛋白 < 0.001 0.907 0.872~0.943 0.083 0.955 0.906~1.006 AGR < 0.001 0.100 0.047~0.213 < 0.001 0.171 0.063~0.460 血红蛋白 < 0.001 0.985 0.977~0.993 0.853 0.999 0.990~1.009 LVEF 0.066 1.013 0.999~1.026 0.373 1.007 0.991~1.023 -
[1] Emmons-Bell S, Johnson C, Roth G. Prevalence, incidence and survival of heart failure: a systematic review[J]. Heart, 2022, 108(17): 1351-1360. doi: 10.1136/heartjnl-2021-320131
[2] 程敏, 廖玉华, 袁璟. 2022 ESC速递: 心力衰竭相关临床研究解读[J]. 临床心血管病杂志, 2022, 38(10): 774-776. https://lcxxg.whuhzzs.com/article/doi/10.13201/j.issn.1001-1439.2022.10.003
[3] Van der Pol A, van Gilst WH, Voor AA, et al. Treating oxidative stress in heart failure: past, present and future[J]. Eur J Heart Fail, 2019, 21(4): 425-435. doi: 10.1002/ejhf.1320
[4] Dick SA, Epelman S. Chronic Heart Failure and Inflammation: what do we really know[J]? Circ Res, 2016, 119(1): 159-176. doi: 10.1161/CIRCRESAHA.116.308030
[5] Sze S, Pellicori P, Zhang J, et al. Malnutrition, congestion and mortality in ambulatory patients with heart failure[J]. Heart, 2019, 105(4): 297-306. doi: 10.1136/heartjnl-2018-313312
[6] Lourenço BH, Vieira LP, Macedo A, et al. Nutritional status and adequacy of energy and nutrient intakes among heart failure patients[J]. Arq Bras Cardiol, 2009, 93(5): 541-548.
[7] Chi J, Xie Q, Jia J, et al. Prognostic value of albumin/globulin ratio in survival and lymph node metastasis in patients with cancer: a systematic review and meta-analysis[J]. J Cancer, 2018, 9(13): 2341-2348. doi: 10.7150/jca.24889
[8] Yuk HD, Ku JH. Role of systemic inflammatory response marker in urothelial carcinoma[J]. Front Oncol, 2020, 10: 1473. doi: 10.3389/fonc.2020.01473
[9] Wu PP, Hsieh YP, Kor CT, et al. Association between albumin-globulin ratio and mortality in patients with chronic kidney disease[J]. J Clin Med, 2019, 8(11): 1991. doi: 10.3390/jcm8111991
[10] Tsai CC, Hsieh YP, Tsai SM, et al. Superiority of albumin-globulin ratio over albumin to predict mortality in patients undergoing peritoneal dialysis[J]. Sci Rep, 2020, 10(1): 19764. doi: 10.1038/s41598-020-73629-5
[11] 中华医学会心血管病学分会心力衰竭学组, 中国医师协会心力衰竭专业委员会, 中华心血管病杂志编辑委员会. 中国心力衰竭诊断和治疗指南2018[J]. 中华心血管病杂志, 2018, 46(10): 760-789. doi: 10.3760/cma.j.issn.0253-3758.2018.10.004
[12] Gounden V, Vashisht R, Jialal I. Hypoalbuminemia[M]. In: StatPearls[Internet]. Treasure Island(FL): StatPearls Publishing, 2022.
[13] Kim S, McClave SA, Martindale RG, et al. Hypoalbuminemia and clinical outcomes: what is the mechanism behind the relationship?[J]. Am Surg, 2017, 83(11): 1220-1227. doi: 10.1177/000313481708301123
[14] Rahman A, Jafry S, Jeejeebhoy K, et al. Malnutrition and cachexia in heart failure[J]. JPEN J Parenter Enteral Nutr, 2016, 40(4): 475-486. doi: 10.1177/0148607114566854
[15] Zhang WJ, Frei B. Albumin selectively inhibits TNF alpha-induced expression of vascular cell adhesion molecule-1 in human aortic endothelial cells[J]. Cardiovasc Res, 2002, 55(4): 820-829. doi: 10.1016/S0008-6363(02)00492-3
[16] Bortoluzzi A, Ceolotto G, Gola E, et al. Positive cardiac inotropic effect of albumin infusion in rodents with cirrhosis and ascites: molecular mechanisms[J]. Hepatology, 2013, 57(1): 266-276. doi: 10.1002/hep.26021
[17] Taverna M, Marie AL, Mira JP, et al. Specific antioxidant properties of human serum albumin[J]. Ann Intensive Care, 2013, 3(1): 4. doi: 10.1186/2110-5820-3-4
[18] Cantin AM, Paquette B, Richter M, et al. Albumin-mediated regulation of cellular glutathione and nuclear factor kappa B activation[J]. Am J Respir Crit Care Med, 2000, 162(4 Pt 1): 1539-1546.
[19] Bal W, Sokołowska M, Kurowska E, et al. Binding of transition metal ions to albumin: sites, affinities and rates[J]. Biochim Biophys Acta. 2013, 1830(12): 5444-5455. doi: 10.1016/j.bbagen.2013.06.018
[20] Neuzil J, Stocker R. Free and albumin-bound bilirubin are efficient co-antioxidants for alpha-tocopherol, inhibiting plasma and low density lipoprotein lipid peroxidation[J]. J Biol Chem, 1994, 269(24): 16712-16719. doi: 10.1016/S0021-9258(19)89449-8
[21] Filippatos GS, Desai RV, Ahmed MI, et al. Hypoalbuminaemia and incident heart failure in older adults[J]. Eur J Heart Fail, 2011, 13(10): 1078-1086. doi: 10.1093/eurjhf/hfr088
[22] Bonilla-Palomas JL, Gámez-López AL, Moreno-Conde M, et al. Hypoalbuminemia in acute heart failure patients: causes and its impact on hospital and long-term mortality[J]. J Card Fail, 2014, 20(5): 350-358. doi: 10.1016/j.cardfail.2014.01.016
[23] Gopal DM, Kalogeropoulos AP, Georgiopoulou VV, et al. Serum albumin concentration and heart failure risk The Health, Aging, and Body Composition Study[J]. Am Heart J, 2010, 160(2): 279-285. doi: 10.1016/j.ahj.2010.05.022
[24] Pacca RL, Silva JB, Souza KC, et al. Autoimmune hemolytic anemia and hyperglobulinemia leading to the diagnosis of multiple myeloma[J]. Rev Bras Hematol Hemoter, 2017, 39(4): 357-359. doi: 10.1016/j.bjhh.2017.07.005
[25] Zhou Q, Cao H, Xu Z, et al. Baseline serum globulin as a predictor of the recurrence of lone atrial fibrillation after radiofrequency catheter ablation[J]. Anatol J Cardiol, 2017, 17(5): 381-385.
[26] Minami Y, Kajimoto K, Sato N, et al. Attend Study Investigators. C-reactive protein level on admission and time to and cause of death in patients hospitalized for acute heart failure[J]. Eur Heart J Qual Care Clin Outcomes, 2017, 3(2): 148-156.
[27] 石雨蒙. 中国H型高血压人群白蛋白-球蛋白比值与全因死亡和心血管死亡的关系[D]. 南昌: 南昌大学, 2021.
[28] Li K, Fu W, Bo Y, et al. Effect of albumin-globulin score and albumin to globulin ratio on survival in patients with heart failure: a retrospective cohort study in China[J]. BMJ Open, 2018, 8(7): e022960. doi: 10.1136/bmjopen-2018-022960
[29] Niedziela JT, Hudzik B, Szygula-Jurkiewicz B, et al. Albumin-to-globulin ratio as an independent predictor of mortality in chronic heart failure[J]. Biomark Med, 2018, 12(7): 749-757. doi: 10.2217/bmm-2017-0378
[30] Otaki Y, Shimizu M, Watanabe T, et al. Albumin-to-globulin ratio predicts clinical outcomes of heart failure with preserved ejection fraction in women[J]. Heart Vessels, 2022, 37(11): 1829-1840. doi: 10.1007/s00380-022-02087-y
[31] Azab B, Bibawy J, Harris K, et al. Value of albumin-globulin ratio as a predictor of all-cause mortality after non-ST elevation myocardial infarction[J]. Angiology, 2013, 64(2): 137-145. doi: 10.1177/0003319712436577
[32] Rajadurai M, Stanely M, Prince P. Preventive effect of naringin on lipid peroxides and antioxidants in isoproterenol-induced cardiotoxicity in Wistar rats: biochemical and histopathological evidences[J]. Toxicology, 2006, 228(2-3): 259-268. doi: 10.1016/j.tox.2006.09.005
[33] Cederholm T, Jensen GL, Correia MI, et al. GLIM criteria for the diagnosis of malnutrition-A consensus report from the global clinical nutrition community[J]. Clin Nutr, 2019, 38(1): 1-9. doi: 10.1016/j.clnu.2018.08.002
[34] Graterol Torres F, Molina M, Soler-Majoral J, et al. Evolving concepts on inflammatory biomarker and malnutrition in chronic kidney disease[J]. Nutrients, 2022, 14(20): 4297. doi: 10.3390/nu14204297
[35] Yin WH, Wei J, Huang WP, et al. Prognostic value of circulating adipokine levels and expressions of adipokines in the myocardium of patients with chronic heart failure[J]. Circ J, 2012, 76(9): 2139-2147. doi: 10.1253/circj.CJ-11-1549
[36] 蒋巧会, 柳芳美, 袁康正, 等. 中性粒细胞和淋巴细胞比值与不同类型心力衰竭患者近期预后关系[J]. 中华老年心脑血管病杂志, 2022, 24(7): 676-680. https://www.cnki.com.cn/Article/CJFDTOTAL-LNXG202207002.htm
[37] Nair N. Epidemiology and pathogenesis of heart failure with preserved ejection fraction[J]. Rev Cardiovasc Med, 2020, 21(4): 531-540. doi: 10.31083/j.rcm.2020.04.154
[38] Pfeffer MA, Shah AM, Borlaug BA. Heart failure with preserved ejection fraction in perspective[J]. Circ Res, 2019, 124(11): 1598-1617. doi: 10.1161/CIRCRESAHA.119.313572
[39] 张班, 刘晓刚, 胡立群. 射血分数保留的心力衰竭研究新进展[J]. 临床心血管病杂志, 2022, 38(4): 271-275. https://lcxxg.whuhzzs.com/article/doi/10.13201/j.issn.1001-1439.2022.04.004
[40] Vidan M T, Bueno H, Wang Y, et al. The relationship between systolic blood pressure on admission and mortality in older patients with heart failure[J]. Eur J Heart fail, 2010, 12(2): 148-155. doi: 10.1093/eurjhf/hfp195
[41] Moreno-González R, Formiga F, Lujan J MM, et al. Usefulness of systolic blood pressure combined with heart rate measured on admission to identify 1-year all-cause mortality risk in elderly patients firstly hospitalized due to acute heart failure[J]. Aging Clinical and Experimental Research, 2020, 32(1): 99-106. doi: 10.1007/s40520-019-01153-2
[42] McEvoy JW, Chen Y, Rawlings A, et al. Diastolic blood pressure, subclinical PH myocardial damage, and cardiac events: implications for blood pressure control[J]. JACC, 2016, 68(16): 1713-1722. doi: 10.1016/j.jacc.2016.07.754
[43] 夏晶晶, 胡辽平, 浦越, 等. 估测的血浆容量状态对心力衰竭患者临床结局的预测价值[J]. 临床心血管病杂志, 2022, 38(11): 895-903. doi: 10.13201/j.issn.1001-1439.2022.11.010 https://lcxxg.whuhzzs.com/article/doi/10.13201/j.issn.1001-1439.2022.11.010
[44] Miao L, Guo M, Pan D, et al. Serum uric acid and risk of chronic heart failure: a systematic review and meta-analysis[J]. Front Med(Lausanne), 2021, 8: 785327.
[45] Paolillo S, Scardovi AB, Campodonico J. Role of comorbidities in heart failure prognosis Part Ⅰ: Anaemia, iron deficiency, diabetes, atrial fibrillation[J]. Eur J Prev Cardiol, 2020, 27(2_suppl): 27-34. doi: 10.1177/2047487320960288
[46] Stegmann C, Hindricks G. Atrial fibrillation in heart failure-diagnostic, therapeutic, and prognostic relevance[J]. Curr Heart Fail Rep, 2019, 16(4): 108-115. doi: 10.1007/s11897-019-00430-5
-




 下载:
下载: