A computer simulation model based on preoperative CTA to investigate the effect of abnormal systolic sharp wave on graft flow and early and mid-term patency rate in off-pump coronary artery bypass grafting
-
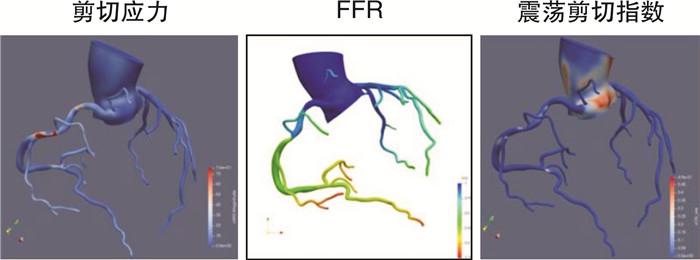
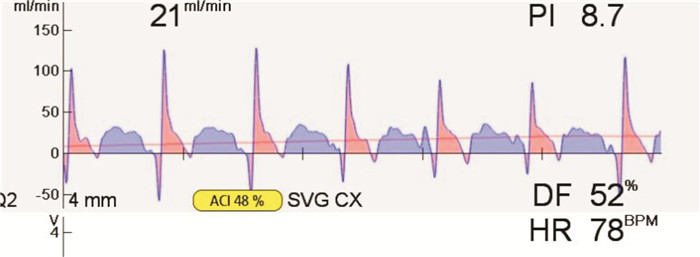
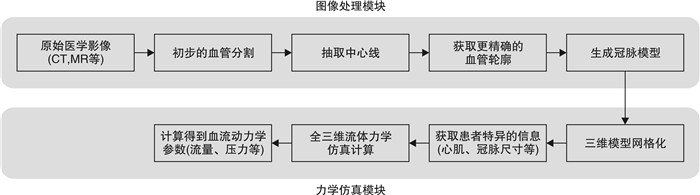
摘要: 目的 使用基于冠状动脉(冠脉)CT血管造影(CTA)图像构建的冠脉旁路移植(CABG)流体仿真模型,通过无创手段获得患者CABG术后桥血管血流动力学参数,并与术中实际测量瞬时桥流量参数进行对比,探讨异常尖波存在的临床意义。方法 选取2018年9月—2019年9月于我院心外科实施首次单纯非体外循环下CABG患者21例。术前完善冠脉CTA检查,术中移植后通过即时血流测量仪(transit time flow measurement,TTFM)完成桥血流测定并记录数据。对术前冠脉CTA资料进行计算机仿真处理,构建个体化模型,计算各个靶血管位点流体力学参数,并与实际手术方案桥流量进行对比。术后1周全部患者出院前完成冠脉CTA复查,术后1年完成冠脉CTA患者16例(76.2%),术后两年完成冠脉CTA复查患者9例(42.9%),术后3年完成冠脉CTA复查患者5例(23.8%)。结果 共11例患者13支桥血管存在异常尖波。通过计算机仿真模型模拟的桥血管流量与术中TTFM实测流量相比差异无统计学意义[(32.58±26.52) mL/min vs (26.66±20.94) mL/min,P=0.160]。按照有无异常尖波分组,异常尖波组中模拟流量明显高于实测流量[(17.91±15.58) mL/min vs(40.68±33.00) mL/min,P=0.006)]。异常尖波组术后冠脉CT提示桥血管狭窄甚至闭塞5例(38.46%),非尖波组存在狭窄3例(6.81%),两组狭窄发生率比较差异有统计学意义(P=0.011)。结论 TTFM中收缩早期的异常尖波很可能是一种非正常血流波形,可能对桥流量存在影响,并会加剧桥血流震荡,降低远期通畅率。Abstract: Objective To explore the clinical significance of abnormal sharp waves by using a fluid simulation model based on coronary CT angiography (CTA) images to obtain the hemodynamic parameters of the grafts by non-invasive Methods, and to compare with the actual instantaneous graft flow measured during the operation by transit time flow measurement (TTFM) in coronary artery bypass grafting (CABG).Methods A total of 21 patients who underwent the first off-pump CABG in the Department of Cardiology of our hospital from September 2018 to September 2019 were enrolled. Coronary CTA examination was completed before the operation, and the graft blood flow was measured and recorded by TTFM after CABG. The preoperative coronary CTA data were processed by computer simulation, and the individual model was constructed. The fluid dynamics parameters of each target site were calculated and compared with the actual surgical plan. All patients completed coronary CTA one week after the operation before discharge, 16 patients (76.2%) completed coronary CTA one year after the operation, 9 patients (42.9%) completed coronary CTA two years after the operation, and 5 patients (23.8%) completed coronary CTA three years after the operation.Results A total of 13 grafts from 11 patients had abnormal sharp waveforms. There was no significant difference between the flow measured by TTFM and the flow simulated by the computer model ([32.58±26.52]mL/min vs [26.66±20.94]mL/min, P=0.160). Grouped according to the presence or absence of abnormal sharp waveform, the simulated flow was significantly higher than the measured flow by TTFM in the abnormal sharp wave group ([40.68±33.0]mL/min vs [17.91±15.58]mL/min, P=0.006). There were 5 cases of graft stenosis or even occlusion in the abnormal sharp waveform group and 3 cases of graft stenosis in the non-sharp waveform group, the difference between the two groups was statistically significant (38.46% vs 6.81%, P=0.011).Conclusion The abnormal sharp waveform in the early systolic phase of TTFM is an abnormal blood flow waveform, which may affect graft flow and exacerbate graft blood flow turbulence, reducing long-term patency.
-

-
表 1 患者基线资料
Table 1. General data
例(%), X±S 项目 数值 年龄/岁 63.71±8.42 男性 16(76.2) 血管移植支数/支 3.10±0.831 BMI/(kg/m2) 25.52±3.73 术前射血分数/% 62.13±12.19 术前左室舒张末期内径/cm 5.10±0.51 糖尿病 9(42.9) 高血压 13(61.9) 高脂血症 9(42.9) 外周血管疾病 3(14.3) 既往脑血管意外 3(14.3) 慢性阻塞性肺疾病 1(4.8) NYHA分级 2.14±0.36 陈旧性心肌梗死 3(14.3) 既往经皮冠脉介入 3(14.3) 慢性肾功能不全 1(4.8) 围术期神经系统并发症 0 围术期CK-MB高于上限10倍a) 1(4.8) a)本中心近年弃用常规肌钙蛋白改为超敏肌钙蛋白,故使用CK-MB作为衡量标准。 表 2 术后随访冠脉CTA异常桥血管
Table 2. Postoperative abnormal vessels in coronary CTA
桥血管 组别 支数 TTFM是否存在异常尖波 术后1周冠脉CTA 术后1年冠脉CTA 术后2年冠脉CTA 术后3年冠脉CTA AO-SVG-RCA 1 1 是 O级 无 无 无 LIMA-LAD 1 1 是 通畅 无 无 无 AO-SVG-OM 2 1 是 A级 B级 无 B级 AO-SVG-CX 3 1 是 A级 B级 无 无 AO-SVG-PDA 4 1 是 通畅 B级 无 无 AO-SVG-CX 5 1 是 通畅 B级 无 无 LIMA-LAD 6 1 是 线样征 通畅 无 无 AO-SVG-PDA 6 1 是 通畅 通畅 无 无 LIMA-LAD 7 1 是 通畅 通畅 无 无 AO-SVG-PDA 8 1 是 通畅 无 无 无 AO-SVG-RCA-PDA 9 1 是 通畅 无 无 无 AO-SVG-Dx 10 1 是 通畅 无 无 无 RIMA-CX 11 1 是 通畅 无 无 无 AO-SVG-CX 12 1 否 通畅 通畅 A级 无 AO-SVG-Dx 13 1 否 通畅 A级 无 无 RIMA-RCA 14 1 否 线样征 无 无 无 AO-RA-CX 15 1 否 线样征 无 通畅a) 无 a)本例患者实施冠脉造影,提示桡动脉桥通畅无狭窄。其余桥血管术后冠脉CTA未见明显异常。LIMA:左侧乳内动脉;RIMA:右侧乳内动脉;RA:桡动脉;SVG:大隐静脉桥;LAD:前降支;RCA:右冠脉;PDA:后降支;OM:钝缘支;Dx:对角支;AO:升主动脉;CX:回旋支。 表 3 计算机模拟和术中TTFM流量对比
Table 3. The flow simulated by computer model and measured by TTFM
X±S 组别 流量/(mL/min) P 全部桥血管数(57支) 0.160 模拟流量 32.58±26.52 术中流量 26.66±20.94 异常尖波组(13支) 0.006 模拟流量 40.68±33.00 实际流量 17.91±15.58 非尖波组(4支) 0.603 模拟流量 29.70±21.58 实际流量 32.22±22.01 -
[1] Ishida M, Ishikawa H, Takami Y, et al. Relationship between fractional flow reserve and graft patency after coronary artery bypass grafting[J]. Gen Thorac Cardiovasc Surg, 2021, 69(11): 1453-1459. doi: 10.1007/s11748-021-01608-2
[2] Tran-Nguyen N, Condemi F, Yan A, et al. Wall Shear Stress Differences Between Arterial and Venous Coronary Artery Bypass Grafts One Month After Surgery[J]. Ann Biomed Eng, 2022, 50(12): 1882-1894. doi: 10.1007/s10439-022-03007-x
[3] Shuhaiber JH, Evans AN, Massad MG, et al. Mechanisms and future directions for prevention of vein graft failure in coronary bypass surgery[J]. Eur J Cardiothorac Surg, 2002, 22(3): 387-396. doi: 10.1016/S1010-7940(02)00253-1
[4] Neumann FJ, Sousa-Uva M, Ahlsson A, et al. 2018 ESC/EACTS Guidelines on myocardial revascularization[J]. Eur Heart J, 2019, 40(2): 87-165. doi: 10.1093/eurheartj/ehy394
[5] 赵舟, 韩增强, 范桄溥, 等. 微创左侧胸壁切口多支冠状动脉旁路移植术前降支平行侧侧吻合方式的尝试[J]. 临床心血管病杂志, 2022, 38(11): 921-925. doi: 10.13201/j.issn.1001-1439.2022.11.014 https://lcxxg.whuhzzs.com/article/doi/10.13201/j.issn.1001-1439.2022.11.014
[6] Dai N, Chen Z, Zhou F, et al. Association of Lipoprotein(a)With Coronary-Computed Tomography Angiography-Assessed High-Risk Coronary Disease Attributes and Cardiovascular Outcomes[J]. Circ Cardiovasc Imaging, 2022, 15(12): e014611.
[7] Lee SH, Hong D, Dai N, et al. Anatomic and Hemodynamic Plaque Characteristics for Subsequent Coronary Events[J]. Front Cardiovasc Med, 2022, 9: 871450. doi: 10.3389/fcvm.2022.871450
[8] Fitzgibbon GM, Kafka HP, Leach AJ, et al. Coronary bypass graft fate and patient outcome: angiographic follow-up of 5, 065 grafts related to survival and reoperation in 1, 388 patients during 25 years[J]. J Am Coll Cardiol, 1996, 28(3): 616-626. doi: 10.1016/0735-1097(96)00206-9
[9] Fan TT, Lu Y, Gao Y, et al. Hemodynamics of left internal mammary artery bypass graft: Effect of anastomotic geometry, coronary artery stenosis, and postoperative time[J]. J Biomech, 2016, 49(5): 645-652. doi: 10.1016/j.jbiomech.2016.01.031
[10] Sankaranarayanan M, Ghista DN, Poh CL, et al. Analysis of blood flow in an out-of-plane CABG model[J]. Am J Physiol Heart Circ Physiol, 2006, 291(1): H283-295. doi: 10.1152/ajpheart.01347.2005
[11] Pekkan K, Whited B, Kanter K, et al. Patient-specific surgical planning and hemodynamic computational fluid dynamics optimization through free-form haptic anatomy editing tool(SURGEM)[J]. Med Biol Eng Comput, 2008, 46(11): 1139-1152. doi: 10.1007/s11517-008-0377-0
[12] 邓欣, 沈雳, 王瑞, 等. 基于冠状动脉CT的血流储备分数在心肌缺血中的诊断应用价值: 一项单中心前瞻性研究[J]. 中国介入心脏病学杂志, 2021, 29(3): 138-142. doi: 10.3969/j.issn.1004-8812.2021.03.005
[13] Zeng Y, Wang X, Tang Z, et al. Diagnostic accuracy of CT-FFR with a new coarse-to-fine subpixel algorithm in detecting lesion-specific ischemia: a prospective multicenter study[J]. Rev Esp Cardiol (Engl Ed), 2023, S1885-5857(23)00196-2.
[14] Amin S, Werner RS, Madsen PL, et al. Intraoperative Bypass Graft Flow Measurement With Transit Time Flowmetry: A Clinical Assessment[J]. Ann Thorac Surg, 2018, 106(2): 532-538. doi: 10.1016/j.athoracsur.2018.02.067
[15] Niclauss L. Techniques and standards in intraoperative graft verification by transit time flow measurement after coronary artery bypass graft surgery: a critical review[J]. Eur J Cardiothorac Surg, 2017, 51(1): 26-33. doi: 10.1093/ejcts/ezw203
[16] Mao B, Feng Y, Wang W, et al. The influence of hemodynamics on graft patency prediction model based on support vector machine[J]. J Biomech, 2020, 98: 109426. doi: 10.1016/j.jbiomech.2019.109426
[17] Iida A, Sezai A, Orime Y, et al. An Experimental Study of the Effects of IABP on Coronary Artery Bypass Graft Flow Waveform[J]. Ann Thorac Cardiovasc Surg, 2021, 27(3): 176-184. doi: 10.5761/atcs.oa.20-00150
[18] Rezaeimoghaddam M, Oguz GN, Ates MS, et al. Patient-Specific Hemodynamics of New Coronary Artery Bypass Configurations[J]. Cardiovasc Eng Technol, 2020, 11(6): 663-678. doi: 10.1007/s13239-020-00493-9
[19] 李兰兰, 刘有军, 毛伯龑, 等. 不同冠脉后负荷下竞争流对左乳内动脉桥血流动力学影响[J]. 北京生物医学工程, 2016, 35(4): 331-338. doi: 10.3969/j.issn.1002-3208.2016.04.01
[20] Li B, Mao BY, Feng Y, et al. The Hemodynamic Mechanism of FFR-Guided Coronary Artery Bypass Grafting[J]. Front Physiol, 12: 503687.
-




 下载:
下载: