Correlation between the diagnosis-to-ablation time and the recurrence after atrial fibrillation ablation
-
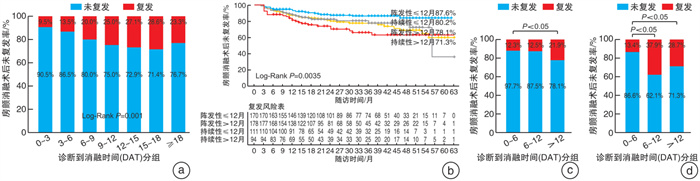
摘要: 目的 通过回顾性分析心房颤动(房颤)患者诊断到消融时间(DAT)与术后复发的相关性,探讨房颤患者诊断到消融的最佳时间。 方法 选取2017年1月—2022年1月于我院首次行射频消融术的房颤患者,出院后定期通过门诊或电话对其进行随访。针对术后复发的影响因素采用多因素logistic回归分析法;Kaplan-Meier生存曲线用于对房颤消融术后未复发率进行分析。 结果 共纳入553例房颤患者,其中持续性房颤占37.1%,女性占44.3%,年龄为(62.3±10.21)岁,DAT为12(3,48)个月,术后随访(26.7±16.36)个月,房颤消融术后总体未复发率为80.3%。logistic回归分析显示,DAT(OR=1.005,95%CI:1.0~1.011,P<0.05)、持续性房颤(OR=1.952,95%CI:1.160~3.385,P<0.05)和女性是术后复发的独立危险因素。Kaplan-Meier生存分析表明,房颤伴DAT≤12个月的患者消融术后未复发率明显高于DAT>12个月的患者(84.8% vs.75.7%,P<0.05),持续性房颤患者消融术后未复发率明显低于阵发性房颤患者(76.1% vs.82.8%,P<0.05),而房颤患者男女间消融术后未复发率差别无统计学意义。按照DAT每间隔6个月分成0~6个月组、6~12个月组和>12个月组:阵发性房颤患者3组间消融术后累积未复发率差异有统计学意义(P<0.05),DAT 0~6个月组和DAT 6~12个月组未复发率明显高于DAT>12个月组(P<0.05),前两组间差异无统计学意义;持续性房颤患者3组间消融术后的累积未复发率差异有统计学意义(P<0.05),DAT 0~6个月组明显高于DAT 6~12个月组和DAT>12个月组(P<0.05),后两组间差异无统计学意义。 结论 房颤患者尽早接受导管消融有较高的未复发率,阵发性房颤患者在DAT < 12个月内、持续性房颤患者在DAT < 6个月内接受导管消融有助于降低术后复发率。Abstract: Objective To analyze the correlation between the diagnosis-to-ablation time(DAT) and recurrence after atrial fibrillation(AF) ablation retrospectively, and explore the optimal time of DAT. Methods Patients with AF who underwent radiofrequency ablation for the first time at our hospital from January 2017 to January 2022 were selected for regular follow-up at an outpatient or by telephone after discharge. Multifactorial logistic regression was used to analyze factors influencing recurrence after AF ablation. The Kaplan-Meier survival curve was used to analyze the non-recurrence rate in AF patients after ablation. Results A total of 553 patients with AF were enrolled, including 37.1% persistent AF, 44.3% female, a mean age of(62.3±10.21) years, the DAT of 12(3, 48) months. After the mean follow-up time of(26.7±16.36) months, the non-recurrence rate of AF after ablation was 80.3%. Multivariate logistic regression analysis indicated that DAT(OR=1.005, 95%CI: 1.0-1.011, P < 0.05), persistent AF(OR=1.952, 95%CI: 1.160-3.385, P < 0.05) and female(OR=1.698, 95%CI: 1.056-2.731, P < 0.05) was an independent risk factor for recurrence after AF ablation. Kaplan-Meier survival analysis indicated that the non-recurrence rate in the patients with DAT≤12 months was significantly higher than that in the patients with DAT>12 months(84.8% vs. 75.7%, P < 0.05); The non-recurrence rate of persistent AF patients was significantly lower than that of paroxysmal AF patients(76.1% vs. 82.8%, P < 0.05). There was no significant difference between males and females in the non-recurrence rate of AF. Patients were divided into the 0-6 months group, 6-12 months group, and>12 months group according to the DAT interval. There was a significant difference in the cumulative non-recurrence rate after ablation among the three groups in patients with paroxysmal AF, and the non-recurrence rate was significantly higher in the DAT 0-6 months group and DAT 6-12 months groups than that in the DAT>12 months group(P < 0.05), whereas the difference between the former two groups was not statistically significant. In patients with persistent AF, there was a statistically significant difference in the cumulative non-recurrence rate after ablation among the three groups(P < 0.05), and the cumulative non-recurrence rate in the DAT 0-6 months group was significantly higher than that in the DAT 6-12 months group and the DAT>12 months group(P < 0.05), while there was no statistically significant difference between the latter two groups. Conclusion Patients with AF who undergo catheter ablation early have higher non-recurrence rates. Catheter ablation in patients with paroxysmal AF within 12 months of DAT and in patients with persistent AF within 6 months of DAT can help to reduce the recurrence rate.
-
Key words:
- atrial fibrillation /
- catheter ablation /
- recurrence /
- diagnosis-to-ablation time
-

-
表 1 患者临床基本资料
Table 1. General clinical data
例(%), X±S, M(P25, P75) 项目 总体(553例) 阵发性房颤组(348例) 持续性房颤(205例) P值 年龄/岁 62.3±10.2 62.1±10.8 62.6±9.2 0.542 女性 245(44.3) 160(46.0) 85(41.5) 0.302 BMI/(kg/m2) 25.1±3.4 24.9±3.3 25.6±3.6 0.022 CHA2DS2VASc评分 2(1,3) 2(1,3) 2(1,3) 0.356 DAT/月 12.0(3.0,48.0) 13.5(4.0,48.8) 12.0(3.0,36.0) 0.122 高血压 330(59.7) 208(59.8) 122(59.5) 0.952 糖尿病 77(13.9) 47(13.5) 30(14.6) 0.711 冠心病 58(10.5) 42(12.1) 16(7.8) 0.114 脑梗死 51(9.2) 37(10.6) 14(6.8) 0.135 心功能不全 89(16.1) 27(7.8) 62(30.2) <0.001 LAD/mm 43.7±5.9 41.5±5.0 47.3±5.5 <0.001 LVEDd/mm 49.3±4.9 48.8±4.5 50.0±5.5 0.008 LVEF/% 60.8±7.7 62.5±6.3 58.0±9.0 <0.001 表 2 复发组与未复发组临床基本资料的比较
Table 2. General clinical data in the recurrence group and non-recurrence group
例(%), X±S, M(P25, P75) 项目 未复发组(444例) 复发组(109例) t/z/χ2值 P值 年龄/岁 62.5±10.36 61.5±9.60 0.904 0.366 女性 190(42.8) 55(50.5) 2.084 0.149 持续性房颤 156(35.1) 49(45.0) 3.617 0.057 BMI/(kg/m2) 25.1±3.42 25.1±3.51 0.109 0.913 CHA2DS2VASc评分 2(1,3) 2(1,3) 0.594 0.552 DAT/月 12(3,48) 24(9,48) 2.810 0.005 高血压 260(58.6) 70(64.2) 1.166 0.280 糖尿病 66(14.9) 11(10.1) 1.664 0.197 冠心病 48(10.8) 10(9.2) 0.250 0.617 脑梗死 38(8.6) 13(11.9) 1.186 0.276 心功能不全 74(16.7) 15(13.8) 0.547 0.460 LAD/mm 43.6±5.77 44.0±6.43 0.556 0.579 LVEDd/mm 49.2±4.83 49.5±5.31 0.564 0.573 LVEF/% 60.7±7.53 61.3±8.34 0.744 0.457 PVI 305(68.7) 77(70.6) 0.156 0.693 表 3 消融术后复发危险因素的多因素logistic回归分析
Table 3. Risk factors for recurrence after ablation analyzed by multivariate logistic regression analysis
项目 OR(95%CI) P值 年龄 0.979(0.955~1.003) 0.080 女性 1.698(1.056~2.731) 0.029 持续性房颤 1.952(1.160~3.285) 0.012 BMI 0.991(0.925~1.061) 0.789 DAT 1.005(1.000~1.011) 0.049 高血压 1.410(0.881~2.258) 0.152 糖尿病 0.587(0.285~1.207) 0.147 冠心病 0.971(0.459~2.052) 0.938 脑梗死 1.750(0.868~3.527) 0.118 心功能不全 0.710(0.337~1.495) 0.367 LAD 0.994(0.949~1.041) 0.792 LVEDd 1.033(0.980~1.088) 0.225 LVEF 1.013(0.976~1.050) 0.501 -
[1] Hindricks G, Potpara T, Dagres N, et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery(EACTS): The Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology(ESC)Developed with the special contribution of the European Heart Rhythm Association(EHRA)of the ESC[J]. Eur Heart J, 2021, 42(5): 373-498. doi: 10.1093/eurheartj/ehaa612
[2] 周利慧, 王媛, 李书, 等. 1990—2019年中国居民房颤发病和死亡趋势分析及预测[J]. 中国慢性病预防与控制, 2022, 30(6): 410-414. https://www.cnki.com.cn/Article/CJFDTOTAL-ZMXB202206006.htm
[3] McCarthy PM, Cox JL, Kislitsina ON, et al. Surgery and Catheter Ablation for Atrial Fibrillation: History, Current Practice, and Future Directions[J]. J Clin Med, 2021, 11(1): 210. doi: 10.3390/jcm11010210
[4] Padfield GJ, Steinberg C, Swampillai J, et al. Progression of paroxysmal to persistent atrial fibrillation: 10-year follow-up in the Canadian Registry of Atrial Fibrillation[J]. Heart Rhythm, 2017, 14(6): 801-807. doi: 10.1016/j.hrthm.2017.01.038
[5] Kato T, Yamashita T, Sagara K, et al. Progressive nature of paroxysmal atrial fibrillation. Observations from a 14-year follow-up study[J]. Circ J, 2004, 68(6): 568-572. doi: 10.1253/circj.68.568
[6] Kuck KH, Lebedev DS, Mikhaylov EN, et al. Catheter ablation or medical therapy to delay progression of atrial fibrillation: the randomized controlled atrial fibrillation progression trial(ATTEST)[J]. Europace, 2021, 23(3): 362-369. doi: 10.1093/europace/euaa298
[7] Pranata R, Chintya V, Raharjo SB, et al. Longer diagnosis-to-ablation time is associated with recurrence of atrial fibrillation after catheter ablation-Systematic review and meta-analysis[J]. J Arrhythm, 2020, 36(2): 289-294. doi: 10.1002/joa3.12294
[8] Kawaji T, Shizuta S, Yamagami S, et al. Early choice for catheter ablation reduced readmission in management of atrial fibrillation: Impact of diagnosis-to-ablation time[J]. Int J Cardiol, 2019, 291: 69-76. doi: 10.1016/j.ijcard.2019.03.036
[9] 杨正凯, 徐明珠, 孙世坤, 等. ICE在消融指数指导的房颤消融术中实时监测食管位置的价值探讨[J]. 临床心血管病杂志, 2022, 38(8): 649-654. https://lcxxg.whuhzzs.com/article/doi/10.13201/j.issn.1001-1439.2022.08.010
[10] 王晓飞, 王温立, 胡铭晟, 等. VisiTag指导下心房颤动射频消融术后中期疗效和安全性[J]. 中国心脏起搏与心电生理杂志, 2021, 35(1): 28-32. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGXZ202101007.htm
[11] 王温立, 邹操, 李勋, 等. 消融指数指导心房颤动导管消融的短期疗效及安全性[J]. 中国心脏起搏与心电生理杂志, 2020, 34(4): 337-341. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGXZ202004005.htm
[12] Takigawa M, Takahashi A, Kuwahara T, et al. Long-term outcome after catheter ablation of paroxysmal atrial fibrillation: Impact of different atrial fibrillation foci[J]. Int J Cardiol, 2017, 227: 407-412. doi: 10.1016/j.ijcard.2016.11.028
[13] Voskoboinik A, Moskovitch JT, Harel N, et al. Revisiting pulmonary vein isolation alone for persistent atrial fibrillation: A systematic review and meta-analysis[J]. Heart Rhythm, 2017, 14(5): 661-667. doi: 10.1016/j.hrthm.2017.01.003
[14] Mohanty S, Della Rocca DG, Gianni C, et al. Predictors of recurrent atrial fibrillation following catheter ablation[J]. Expert Rev Cardiovasc Ther, 2021, 19(3): 237-246. doi: 10.1080/14779072.2021.1892490
[15] Hussein AA, Saliba WI, Barakat A, et al. Radiofrequency Ablation of Persistent Atrial Fibrillation: Diagnosis-to-Ablation Time, Markers of Pathways of Atrial Remodeling, and Outcomes[J]. Circ Arrhythm Electrophysiol, 2016, 9(1): e003669.
[16] Lycke M, Kyriakopoulou M, El Haddad M, et al. Predictors of recurrence after durable pulmonary vein isolation for paroxysmal atrial fibrillation[J]. Europace, 2021, 23(6): 861-867. doi: 10.1093/europace/euaa383
[17] Bisbal F, Alarcón F, Ferrero-De-Loma-Osorio A, et al. Diagnosis-to-ablation time in atrial fibrillation: A modifiable factor relevant to clinical outcome[J]. J Cardiovasc Electrophysiol, 2019, 30(9): 1483-1490. doi: 10.1111/jce.14000
[18] De Greef Y, Schwagten B, Chierchia GB, et al. Diagnosis-to-ablation time as a predictor of success: early choice for pulmonary vein isolation and long-term outcome in atrial fibrillation: results from the Middelheim-PVI Registry[J]. Europace, 2018, 20(4): 589-595. doi: 10.1093/europace/euw426
[19] Ausma J, Wijffels M, Thoné F, et al. Structural changes of atrial myocardium due to sustained atrial fibrillation in the goat[J]. Circulation, 1997, 96(9): 3157-3163. doi: 10.1161/01.CIR.96.9.3157
[20] 赵子明, 尹晓盟. 心房颤动射频导管消融术后复发的预测因素[J]. 心血管病学进展, 2016, 37(5): 541-545. https://www.cnki.com.cn/Article/CJFDTOTAL-XXGB201605022.htm
[21] 冯磊, 王文玉, 王中华, 等. 老年CHF合并不同类型心房颤动患者心脏结构及相关因素分析[J]. 中国现代药物应用, 2022, 16(9): 69-72. https://www.cnki.com.cn/Article/CJFDTOTAL-ZWYY202209019.htm
[22] Nattel S, Heijman J, Zhou L, et al. Molecular Basis of Atrial Fibrillation Pathophysiology and Therapy: A Translational Perspective[J]. Circ Res, 2020, 127(1): 51-72. doi: 10.1161/CIRCRESAHA.120.316363
[23] Bunch TJ, May HT, Bair TL, et al. Increasing time between first diagnosis of atrial fibrillation and catheter ablation adversely affects long-term outcomes[J]. Heart Rhythm, 2013, 10(9): 1257-1262. doi: 10.1016/j.hrthm.2013.05.013
[24] Takamiya T, Nitta J, Inaba O, et al. Impact of diagnosis-to-ablation time on non-pulmonary vein triggers and ablation outcomes in persistent atrial fibrillation[J]. J Cardiovasc Electrophysiol, 2021, 32(5): 1251-1258. doi: 10.1111/jce.15002
[25] Takigawa M, Takahashi A, Kuwahara T, et al. Long-term follow-up after catheter ablation of paroxysmal atrial fibrillation: the incidence of recurrence and progression of atrial fibrillation[J]. Circ Arrhythm Electrophysiol, 2014, 7(2): 267-273. doi: 10.1161/CIRCEP.113.000471
[26] Steinberg BA, Hellkamp AS, Lokhnygina Y, et al. Higher risk of death and stroke in patients with persistent vs. paroxysmal atrial fibrillation: results from the ROCKET-AF Trial[J]. Eur Heart J, 2015, 36(5): 288-296. doi: 10.1093/eurheartj/ehu359
[27] Camm AJ, Breithardt G, Crijns H, et al. Real-life observations of clinical outcomes with rhythm-and rate-control therapies for atrial fibrillation RECORDAF(Registry on Cardiac Rhythm Disorders Assessing the Control of Atrial Fibrillation)[J]. J Am Coll Cardiol, 2011, 58(5): 493-501.
-

计量
- 文章访问数: 246
- 施引文献: 0




 下载:
下载: