The value of the mC2HEST score in predicting the risk of prognosis after emergency PCI in patients with acute myocardial infarction
-
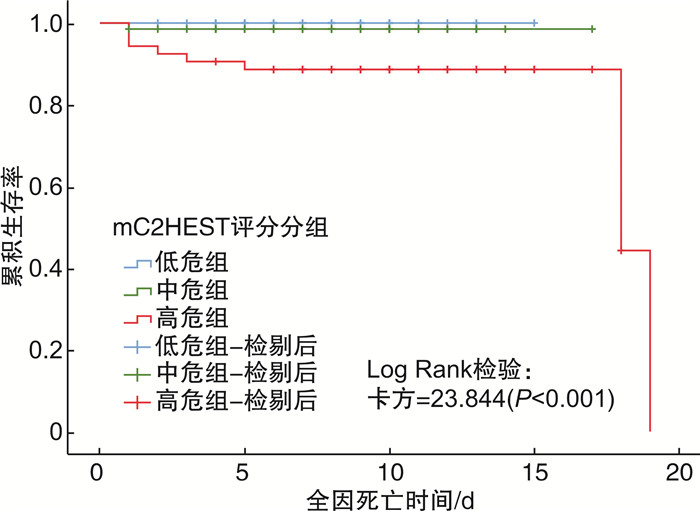
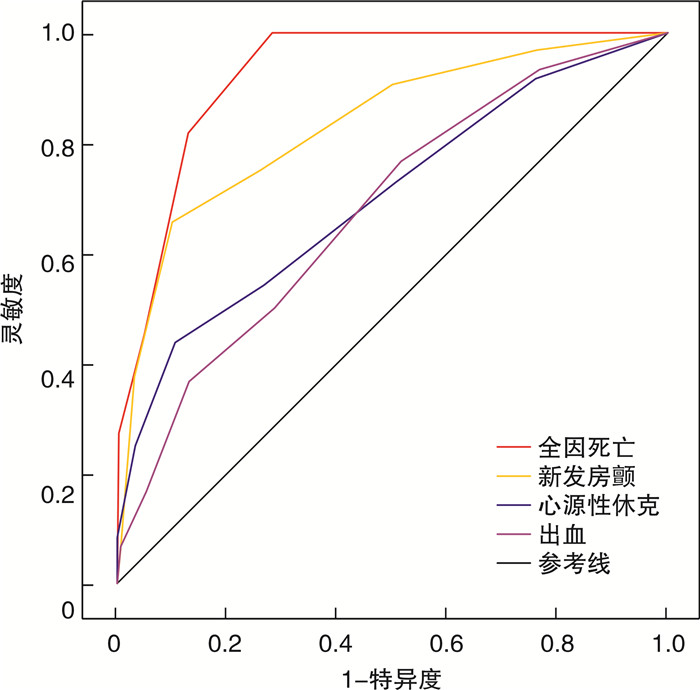
摘要: 目的 分析mC2HEST评分与急性心肌梗死(acute myocardial infarction,AMI)患者急诊经皮冠状动脉介入治疗(percutaneous coronary intervention,PCI)后住院期间预后的关系。方法 收集2020-01-01—2021-12-31在云南大学附属医院心内科住院诊断为AMI并于发病24 h内行急诊PCI术且术前无心房颤动(房颤)的患者,共352例。收集基线资料和院内终点事件(全因死亡、新发房颤、心源性休克、心脏骤停、缺血性卒中、出血),计算mC2HEST评分。比较mC2HEST评分各分数患者的预后事件发生率。使用logistic回归分析探讨mC2HEST评分与预后事件的关系。绘制ROC曲线评估mC2HEST评分预测预后事件的能力。根据mC2HEST评分,将患者分为低危组(1~2分)、中危组(3~4分)和高危组(≥5分),绘制3组患者院内全因死亡的Kaplan-Meier曲线,分析3组患者院内全因死亡的风险差异。结果 全因死亡、新发房颤、心源性休克、出血事件的发生率随着mC2HEST评分的增加而升高。mC2HEST评分是全因死亡(OR=3.993)、新发房颤(OR=3.025)、心源性休克(OR=1.375)、出血(OR=1.334)的独立危险因素。mC2HEST评分对全因死亡(AUC=0.925)、新发房颤(AUC=0.832)具有良好的预测价值,对心源性休克(AUC=0.700)和出血(AUC=0.678)也有一定预测价值。Kaplan-Meier生存曲线提示mC2HEST评分高危组的院内死亡累积风险较中危组、低危组显著升高(P < 0.05)。结论 mC2HEST评分是AMI患者急诊PCI术后住院期间全因死亡、新发房颤、心源性休克、出血的独立危险因素;相较于低危、中危患者,mC2HEST评分高危(≥5分)患者的院内全因死亡风险显著增加。但mC2HEST评分未表现出与心脏骤停和卒中的相关性。Abstract: Objective To analyze the relationship between mC2HEST score and hospitalization outcomes in patients with acute myocardial infarction(AMI) after emergency percutaneous coronary intervention(PCI).Methods Three hundred and fifty-two patients diagnosed with AMI in the Department of Cardiology at Affiliated Hospital of Yunnan University from January 1, 2020 to December 31, 2021 were enrolled. All patients underwent emergency PCI within 24 hours of onset and without preoperative atrial fibrillation. The baseline data and hospital endpoint events, including all-cause death, new-onset atrial fibrillation, cardiogenic shock, cardiac arrest, ischemic stroke, and bleeding, were collected, and the mC2HEST scores were calculated. The incidence of prognostic events among patients with different mC2HEST scores was compared. The logistic regression analysis was used to explore the relationship between mC2HEST score and prognostic events. The ROC curve was drawn to evaluate the ability of the mC2HEST score, and the Kaplan-Meier survival curve was drawn to evaluate the in-hospital all-cause death. Lastly, we analyzed the differences in the risk of in-hospital all-cause death.Results The incidence of all-cause death, new-onset atrial fibrillation, cardiogenic shock, and bleeding events increased with the increase of the mC2HEST score. The mC2HEST score was an independent risk factor for all-cause death(OR=3.993), new-onset atrial fibrillation(OR=3.025), cardiogenic shock(OR=1.375), and bleeding(OR=1.334). The mC2HEST score had good predictive value for all-cause death(AUC=0.925) and new-onset atrial fibrillation(AUC=0.832), as well as for cardiogenic shock(AUC=0.700) and bleeding(AUC=0.678). The Kaplan-Meier survival curve suggested that the cumulative risk of in-hospital death in the mC2HEST score high-risk group was significantly higher compared with the intermediate-risk and low-risk groups(P < 0.05).Conclusion The mC2HEST score is an independent risk factor for all-cause death, new-onset atrial fibrillation, cardiogenic shock, and bleeding during hospitalization in AMI patients after emergency PCI. Compared to low-risk and moderate-risk patients, those with high-risk(mC2HEST score≥5 points) have a significantly increased risk of in-hospital all-cause death. However, the mC2HEST score does not show a correlation with cardiac arrest or stroke.
-
Key words:
- acute myocardial infarction /
- mC2HEST score /
- prognosis /
- predictive value
-

-
表 1 mC2HEST和C2HEST评分系统
Table 1. The mC2HEST and C2HEST system
危险因素 C2HEST评分 mC2HEST评分 C 冠心病 1 1 慢性阻塞性肺病 1 1 H 高血压 1 1 E 年龄≥75岁 2 2 年龄65~74岁 1 S 心力衰竭 2 2 T 甲状腺功能亢进症 1 1 表 2 mC2HEST各评分患者预后事件的发生率
Table 2. Rate of prognostic events for each score of the mC2HEST
例(%) 预后事件 mC2HEST评分 P值 1分(77例) 2分(86例) 3分(82例) 4分(54例) 5分(31例) 6分(18例) 7分(4例) 全因死亡(11例) 0 0 0 2(3.70) 4(12.90) 2(11.10) 3(75.0) < 0.001 新发房颤(32例) 1(1.3) 2(2.3) 5(6.1) 3(5.6) 9(29.0) 10(55.6) 2(50.0) < 0.001 心源性休克(48例) 4(5.2) 9(10.5) 9(11.0) 5(9.3) 9(29.0) 8(44.4) 4(100.0) < 0.001 出血(30例) 2(2.6) 5(5.8) 8(9.8) 4(7.4) 6(19.4) 3(16.7) 2(50.0) 0.018 心脏骤停(8例) 2(2.6) 3(3.5) 1(1.2) 0 0 1(5.6) 1(25.0) 0.187 缺血性卒中(2例) 0 0 0 1(1.9) 0 1(5.6) 0 0.322 表 3 mC2HEST评分与预后事件的单因素logistic回归分析结果
Table 3. Results of univariate logistic regression analysis of the mC2HEST score and prognosis events
预后事件 β Wald OR(95%CI) P 全因死亡 1.319 20.135 3.739(2.102~6.653) < 0.001 新发房颤 0.924 38.890 2.518(1.884~3.367) < 0.001 心源性休克 0.547 26.727 1.727(1.404~2.125) < 0.001 出血 0.426 12.264 1.531(1.206~1.943) < 0.001 表 4 mC2HEST评分与预后事件的多因素logistic回归分析结果
Table 4. Results of multivariate logistic regression analysis of the mC2HEST score and prognosis events
预后事件 β Wald OR(95%CI) P 全因死亡 1.384 9.575 3.993(1.661~9.596) 0.002 新发房颤 1.107 26.614 3.025(1.987~4.607) < 0.001 心源性休克 0.319 4.247 1.375(1.016~1.862) 0.039 出血 0.288 2.485 1.334(0.932~1.907) 0.115 表 5 mC2HEST评分预测预后事件的ROC分析结果
Table 5. ROC analysis results of predicting prognostic events using the mC2HEST score
预后事件 截断值/分 灵敏度/% 特异度/% 约登指数 AUC P 95%CI 全因死亡 3.5 100.00 71.80 0.718 0.925 < 0.001 0.877~0.973 新发房颤 4.5 65.60 89.80 0.554 0.832 < 0.001 0.753~0.912 心源性休克 4.5 43.80 85.90 0.333 0.700 < 0.001 0.614~0.787 出血 2.5 76.70 48.40 0.251 0.678 < 0.001 0.579~0.777 -
[1] 季润青, 余苑, 李静, 等. 急性心肌梗死指南推荐治疗在我国应用现状[J]. 中国循证心血管医学杂志, 2020, 12(2): 250-252. doi: 10.3969/j.issn.1674-4055.2020.02.30
[2] 时之秀, 杜训松, 曹洁. 老年冠心病患者PCI术后主要心脑血管不良事件发生情况及影响因素分析[J]. 临床心血管病杂志, 2022, 38(2): 132-136. https://xueshu.baidu.com/usercenter/paper/show?paperid=144u00e0yr5u06k0j36q08m0ry196793&site=xueshu_se&hitarticle=1
[3] Kim KH, Kim W, Hwang SH, et al. The CHA2DS2VASc score can be used to stratify the prognosis of acute myocardial infarction patients irrespective of presence of atrial fibrillation[J]. J Cardiol, 2015, 65(2): 121-127. doi: 10.1016/j.jjcc.2014.04.011
[4] Li YG, Bai J, Zhou G, et al. Refining age stratum of the C2HEST score for predicting incident atrial fibrillation in a hospital-based Chinese population[J]. Eur J Int Med, 2021, 90: 37-42. doi: 10.1016/j.ejim.2021.04.014
[5] LI YG, Pastori D, Farcomeni A, et al. A Simple Clinical Risk Score(C2HEST)for Predicting Incident Atrial Fibrillation in Asian Subjects: Derivation in 471, 446 Chinese Subjects, With Internal Validation and External Application in 451, 199 Korean Subjects[J]. CHEST, 2019, 155(3): 510-518. doi: 10.1016/j.chest.2018.09.011
[6] Rola P, Doroszko A, Trocha M, et al. The Usefulness of the C2HEST Risk Score in Predicting Clinical Outcomes among Hospitalized Subjects with COVID-19 and Coronary Artery Disease[J]. Viruses, 2022, 14(8): 1771. doi: 10.3390/v14081771
[7] 中华医学会神经病学分会, 中华医学会神经病学分会脑血管病学组. 中国急性缺血性脑卒中诊疗指南2018[J]. 中华神经科杂志, 2018, 51(9): 666-682. doi: 10.3760/cma.j.issn.1006-7876.2018.09.004
[8] 黄从新, 张澍, 黄德嘉, 等. 心房颤动: 目前的认识和治疗的建议-2018[J]. 中国心脏起搏与心电生理杂志, 2018, 32(4): 315-368. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGXZ201905002.htm
[9] 中华医学会心血管病学分会心血管急重症学组, 中华心血管病杂志编辑委员会. 心源性休克诊断和治疗中国专家共识2018[J]. 中华心血管病杂志, 2019, 47(4): 265-277. doi: 10.3760/cma.j.issn.0253-3758.2019.04.003
[10] 中华医学会, 中华医学会临床药学分会, 中华医学会杂志社, 等. 心脏骤停基层合理用药指南[J]. 中华全科医师杂志, 2021, 20(3): 307-310.
[11] Wiviott SD, Antman EM, Gibson CM, et al. Evaluation of prasugrel compared with clopidogrel in patients with acute coronary syndromes: design and rationale for the TRial to assess Improvement in Therapeutic Outcomes by optimizing platelet InhibitioN with prasugrel Thrombolysis In Myocardial Infarction 38(TRITON-TIMI 38)[J]. Am Heart J, 2006, 152(4): 627-635. doi: 10.1016/j.ahj.2006.04.012
[12] Guo T, Xi Z, Qiu H, et al. Prognostic value of GRACE and CHA2DS2-VASc score among patients with atrial fibrillation undergoing percutaneous coronary intervention[J]. Ann Med, 2021, 53(1): 2215-2224.
[13] Chan MY, Shah BR, Gao F, et al. Recalibration of the Global Registry of Acute Coronary Events risk score in a multiethnic Asian population[J]. Am Heart J, 2011, 162(2): 291-299. doi: 10.1016/j.ahj.2011.05.016
[14] Zack CJ, Senecal C, Kinar Y, et al. Leveraging Machine Learning Techniques to Forecast Patient Prognosis After Percutaneous Coronary Intervention[J]. JACC Cardiovasc Interv, 2019, 12(14): 1304-1311. doi: 10.1016/j.jcin.2019.02.035
[15] 陈润真, 刘臣, 周鹏, 等. 急性心肌梗死患者经皮冠状动脉介入治疗术后心功能与长期预后的关系[J]. 中华心力衰竭和心肌病杂志, 2020, 4(3): 159-167.
[16] Hawkins N, Huang Z, Pieper KS, et al. Chronic obstructive pulmonary disease is an independent predictor of death but not atherosclerotic events in patients with myocardial infarction: analysis of the Valsartan in Acute Myocardial Infarction Trial(VALIANT)[J]. Eur J Heart Fail, 2009, 11(3): 292-298. doi: 10.1093/eurjhf/hfp001
[17] Rothnie KJ, Smeeth L, Pearce N, et al. Predicting mortality after acute coronary syndromes in people with chronic obstructive pulmonary disease[J]. Heart, 2016, 102(18): 1442-1448. doi: 10.1136/heartjnl-2016-309359
[18] Gustafsson F, KøBER L, Torp-pedersen C, et al. Long-term prognosis after acute myocardial infarction in patients with a history of arterial hypertension. TRACE study group[J]. Eur J Heart Fail, 1998, 19(4): 588-594. doi: 10.1053/euhj.1997.0822
[19] Li MF, Wei ZT, Li S, et al. Association of Mild Thyroid Dysfunction and Adverse Prognosis Among Chinese Patients With Acute ST Segment Elevation Myocardial Infarction[J]. Front Endocrinol, 2022, 13: 879443. doi: 10.3389/fendo.2022.879443
[20] Razvi S, Leng O, Jabbar A, et al. Sample Timing, Diagnosis of Subclinical Thyroid Dysfunction and Mortality in Acute Myocardial Infarction: ThyrAMI1 Study[J]. J Clin Endocrinol Metab, 2020;105(4): dgz143.
[21] Biccirè FG, Tanzilli G, Prati F, et al. Prediction of new onset atrial fibrillation in patients with acute coronary syndrome undergoing percutaneous coronary intervention using the C2HEST and mC2HEST scores: A report from the multicenter REALE-ACS registry[J]. Int J Cardiol, 2023, 386: 45-49. doi: 10.1016/j.ijcard.2023.05.023
[22] Khalfallah M, Elseikh A. Incidence, predictors, and outcomes of new-onset atrial fibrillation in patients with ST-elevation myocardial infarction[J]. Ann Noninvasive Electrocardiol, 2020, 25(4): e12746. doi: 10.1111/anec.12746
[23] Jin YY, Bai R, Ye M, et al. Risk factors and prognoses analysis of new-onset atrial fibrillation in patients with acute myocardial infarction[J]. Zhonghua Nei Ke Za Zhi, 2019, 58(2): 133-138.
[24] Wi J, Shin DH, Kim JS, et al. Transient New-Onset Atrial Fibrillation Is Associated With Poor Clinical Outcomes in Patients With Acute Myocardial Infarction[J]. Circ J, 2016, 80(7): 1615-1623. doi: 10.1253/circj.CJ-15-1250
[25] Redfors B, Angerås O, Råmunddal T, et al. 17-year trends in incidence and prognosis of cardiogenic shock in patients with acute myocardial infarction in western Sweden[J]. Int J Cardiol, 2015, 185: 256-262. doi: 10.1016/j.ijcard.2015.03.106
[26] 张志宇, 王世鹏, 刘俊倩, 等. 联合指标预测模型对心肌梗死后心源性休克患者院内死亡的预测价值[J]. 临床心血管病杂志, 2023, 39(7): 508-515. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXB202307005.htm
[27] Costa F, Tijssen JG, AriottiI S, et al. Incremental Value of the CRUSADE, ACUITY, and HAS-BLED Risk Scores for the Prediction of Hemorrhagic Events After Coronary Stent Implantation in Patients Undergoing Long or Short Duration of Dual Antiplatelet Therapy[J]. J Am Heart Assoc, 2015, 4(12): e002524. doi: 10.1161/JAHA.115.002524
[28] Rola P, Doroszko A, Trocha M, et al. Sex-Dependent Differences in Predictive Value of the C2HEST Score in Subjects with COVID-19-A Secondary Analysis of the COLOS Study[J]. Viruses, 2022, 14(3): 628.
-




 下载:
下载: