Family mutation of PKP2 gene and arrhythmogenic right ventricular cardiomyopathy phenotypic analysis: one case report
-
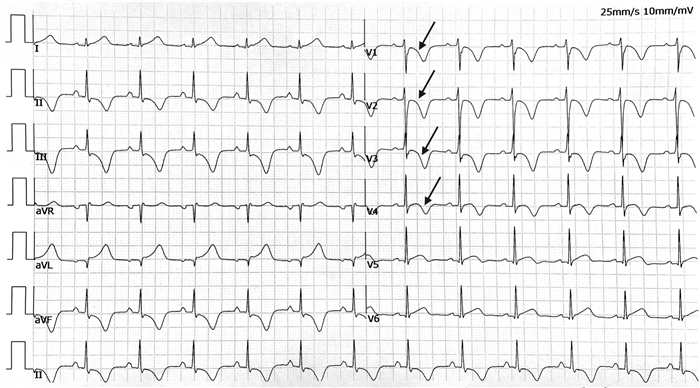
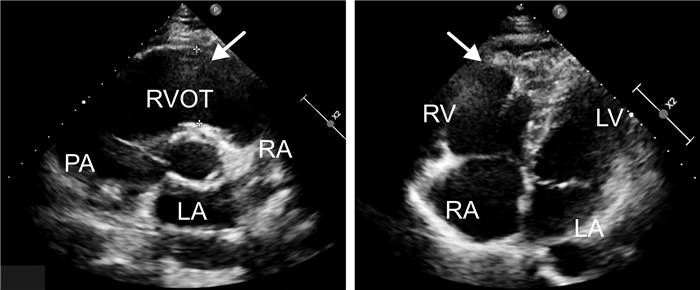
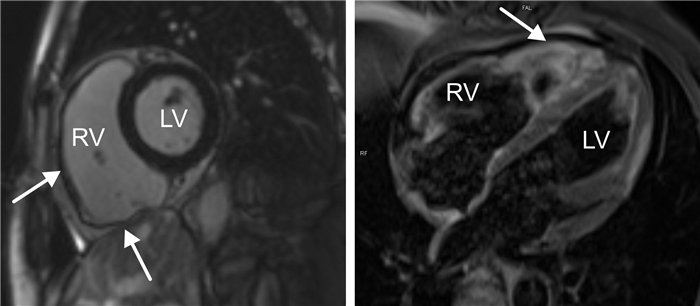
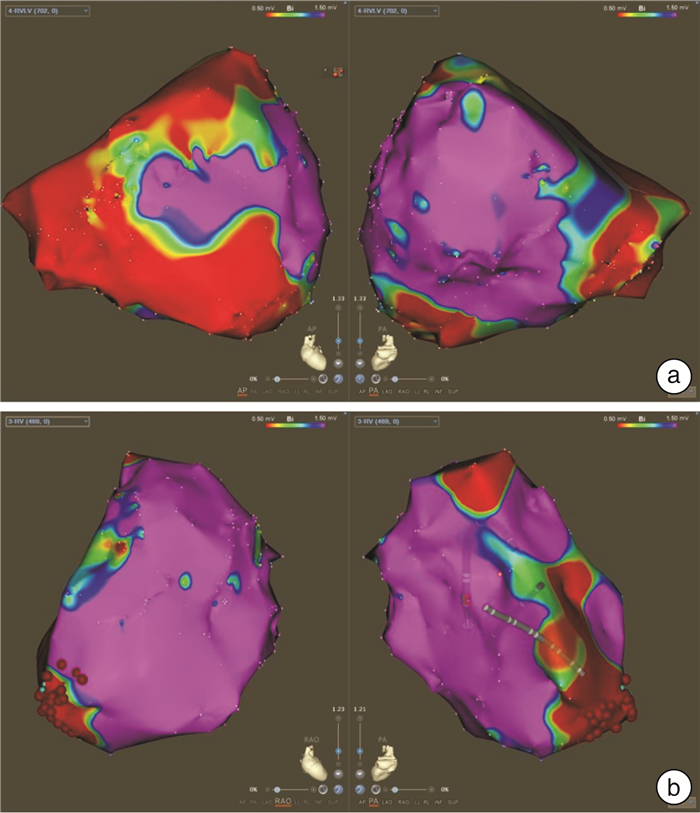
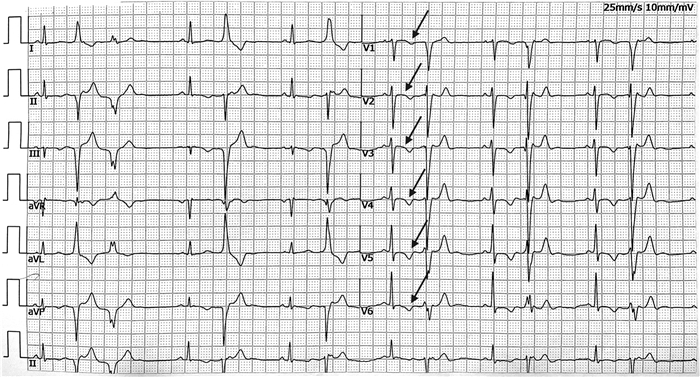
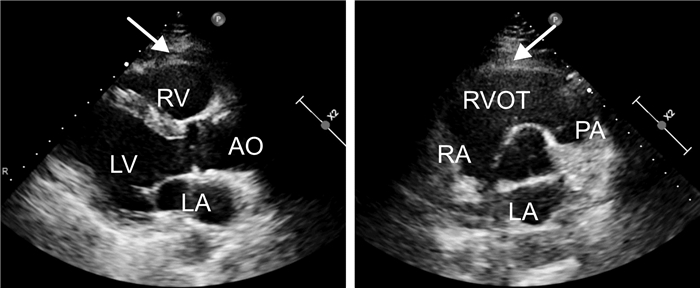
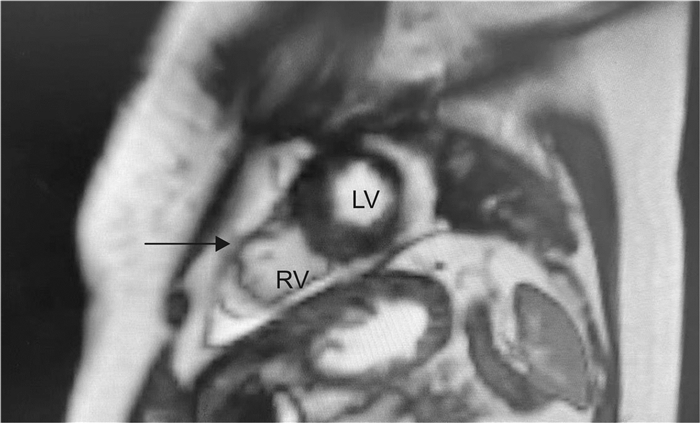
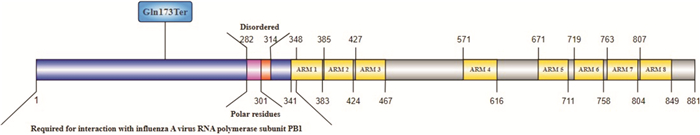
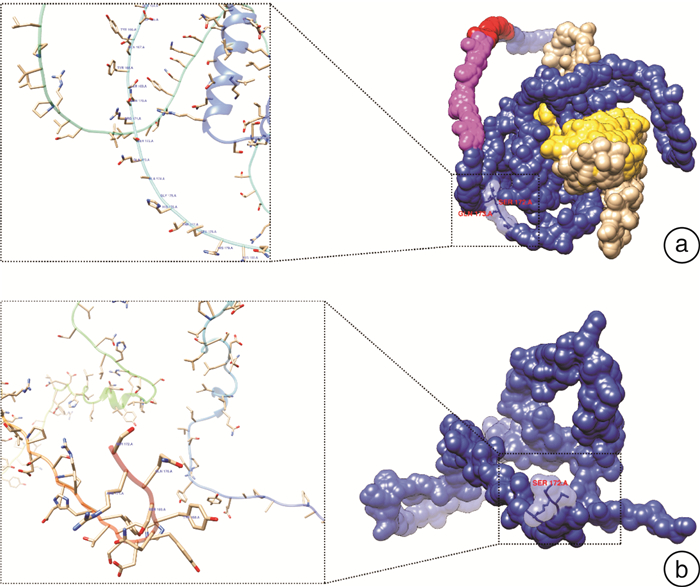
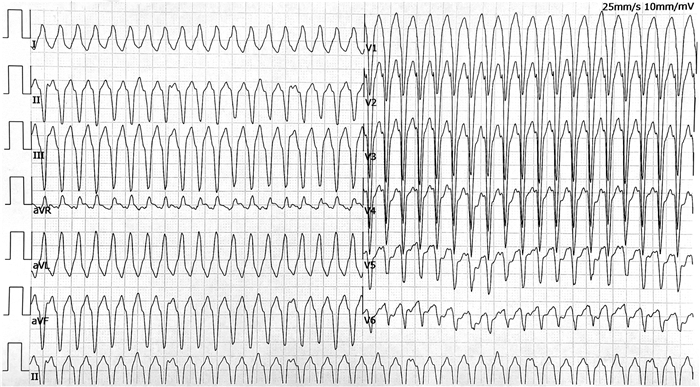
摘要: 1例青年男性患者经相关检查确诊为致心律失常性右室心肌病(ARVC)先证者后,收集先证者家系的临床资料,对先证者及发病家系成员进行全基因组测序,筛选可疑致病基因,并通过Sanger测序法进行验证。对该家系筛查发现先证者及其母亲均为PKP2基因c.517C>T杂合无义突变携带者,余家系成员及对照组均未携带该致病突变。本研究发现PKP2基因家系突变可能导致家族性遗传,其表型分析符合典型ARVC临床特点并且无左室功能受累。
-
关键词:
- 致心律失常性心肌病 /
- 致心律失常性右室心肌病 /
- PKP2基因 /
- 基因表型分析
Abstract: To perform pathogenic gene screening on the family members of a patient with arrhythmogenic right ventricular cardiomyopathy(ARVC) and analyze the correlation between their genotype and phenotype. The study focused on a young male admitted with a diagnosis of ventricular arrhythmia. After diagnosing the patient with ARVC, clinical data from both the patient and family members were collected and analyzed using whole genome sequencing. Suspected pathogenic genes were screened and verified through Sanger sequencing. Relevant genetic screening was conducted on other family members and the control group. The patient and his mother were diagnosed as carriers of the c. 517C>T heterozygous nonsense variation of the PKP2 gene mutation. This study indicates that a familial PKP2 gene mutation might lead to familial inheritance. The phenotypic analysis was consistent with the typical clinical features of ARVC without involving left ventricular function. -

-
[1] Goff ZD, Calkins H. Sudden death related cardiomyopathies-Arrhythmogenic right ventricular cardiomyopathy, arrhythmogenic cardiomyopathy, and exercise-induced cardiomyopathy[J]. Prog Cardiovasc Dis, 2019, 62(3): 217-226. doi: 10.1016/j.pcad.2019.04.002
[2] Marcus FI, McKenna WJ, Sherrill D, et al. Diagnosis of arrhythmogenic right ventricular cardiomyopathy/dysplasia: proposed modification of the Task Force Criteria[J]. Eur Heart J, 2010, 31(7): 806-814. doi: 10.1093/eurheartj/ehq025
[3] Wang W, Tichnell C, Murray BA, et al. Exercise restriction is protective for genotype-positive family members of arrhythmogenic right ventricular cardiomyopathy patients[J]. Europace, 2020, 22(8): 1270-1278. doi: 10.1093/europace/euaa105
[4] Bosman LP, Te Riele A. Arrhythmogenic right ventricular cardiomyopathy: a focused update on diagnosis and risk stratification[J]. Heart, 2022, 108(2): 90-97. doi: 10.1136/heartjnl-2021-319113
[5] Protonotarios A, Bariani R, Cappelletto C, et al. Importance of genotype for risk stratification in arrhythmogenic right ventricular cardiomyopathy using the 2019 ARVC risk calculator[J]. Eur Heart J, 2022, 43(32): 3053-3067. doi: 10.1093/eurheartj/ehac235
[6] Gandjbakhch E, Redheuil A, Pousset F, et al. Clinical Diagnosis, Imaging, and Genetics of Arrhythmogenic Right Ventricular Cardiomyopathy/Dysplasia: JACC State-of-the-Art Review[J]. J Am Coll Cardiol, 2018, 72(7): 784-804. doi: 10.1016/j.jacc.2018.05.065
[7] 中华医学会心血管病学分会精准心血管病学学组, 中国医疗保健国际交流促进会, 精准心血管病分会, 等. 单基因遗传性心血管疾病基因诊断指南[J]. 中华心血管病杂志, 2019, 47(3): 175-195. https://www.cnki.com.cn/Article/CJFDTOTAL-SYNK202004008.htm
[8] Bhonsale A, Groeneweg JA, James CA, et al. Impact of genotype on clinical course in arrhythmogenic right ventricular dysplasia/cardiomyopathy-associated mutation carriers[J]. Eur Heart J, 2015, 36(14): 847-855. doi: 10.1093/eurheartj/ehu509
[9] Hermida A, Fressart V, Hidden-Lucet F, et al. High risk of heart failure associated with desmoglein-2 mutations compared to plakophilin-2 mutations in arrhythmogenic right ventricular cardiomyopathy/dysplasia[J]. Eur J Heart Fail, 2019, 21(6): 792-800. doi: 10.1002/ejhf.1423
[10] Biernacka EK, Borowiec K, Franaszczyk M, et al. Pathogenic variants in plakophilin-2 gene(PKP2) are associated with better survival in arrhythmogenic right ventricular cardiomyopathy[J]. J Appl Genet, 2021, 62(4): 613-620. doi: 10.1007/s13353-021-00647-y
[11] Bhonsale A, Groeneweg JA, James CA, et al. Impact of genotype on clinical course in arrhythmogenic right ventricular dysplasia/cardiomyopathy-associated mutation carriers[J]. Eur Heart J, 2015, 36(14): 847-855. doi: 10.1093/eurheartj/ehu509
[12] Belhassen B, Laredo M, Roudijk RW, et al. The prevalence of left and right bundle branch block morphology ventricular tachycardia amongst patients with arrhythmogenic cardiomyopathy and sustained ventricular tachycardia: insights from the European Survey on Arrhythmogenic Cardiomyopathy[J]. Europace, 2022, 24(2): 285-295. doi: 10.1093/europace/euab190
[13] Austin KM, Trembley MA, Chandler SF, et al. Molecular mechanisms of arrhythmogenic cardiomyopathy[J]. Nat Rev Cardiol, 2019, 16(9): 519-537. doi: 10.1038/s41569-019-0200-7
[14] van Opbergen CJ, Delmar M, van Veen TA. Potential new mechanisms of pro-arrhythmia in arrhythmogenic cardiomyopathy: focus on calcium sensitive pathways[J]. Neth Heart J, 2017, 25(3): 157-169. doi: 10.1007/s12471-017-0946-7
[15] Cerrone M, Montnach J, Lin X, et al. Plakophilin-2 is required for transcription of genes that control calcium cycling and cardiac rhythm[J]. Nat Commun, 2017, 8(1): 106. doi: 10.1038/s41467-017-00127-0
[16] Franklin BA, Thompson PD, Al-Zaiti SS, et al. Exercise-related acute cardiovascular events and potential deleterious adaptations following long-term exercise training: placing the risks into perspective-an update: a scientific statement from the American Heart Association[J]. Circulation, 2020, 141(13): e705-e736.
[17] 中国医药卫生文化协会心血管健康与科学运动分会. 运动相关心血管事件风险的评估与监测中国专家共识[J]. 中国循环杂志, 2022, 37(7): 659-668. doi: 10.3969/j.issn.1000-3614.2022.07.002
[18] Bosman LP, Cadrin-Tourigny J, Bourfiss M, et al. Diagnosing arrhythmogenic right ventricular cardiomyopathy by 2010 Task Force Criteria: clinical performance and simplified practical implementation[J]. Europace, 2020, 22(5): 787-796. doi: 10.1093/europace/euaa039
[19] Andrews CM, Srinivasan NT, Rosmini S, et al. Electrical and Structural Substrate of Arrhythmogenic Right Ventricular Cardiomyopathy Determined Using Noninvasive Electrocardiographic Imaging and Late Gadolinium Magnetic Resonance Imaging[J]. Circ Arrhythm Electrophysiol, 2017, 10(10): 110.
[20] 梁晴, 陶琴. JPH2基因p. R616C突变与家族性扩张型心肌病的相关性分析[J]. 临床心血管病杂志, 2023, 39(4): 303-307. https://lcxxg.whuhzzs.com/article/doi/10.13201/j.issn.1001-1439.2023.04.013
[21] van Opbergen C, Bagwan N, Maurya SR, et al. Exercise causes arrhythmogenic remodeling of intracellular calcium dynamics in plakophilin-2-deficient hearts[J]. Circulation, 2022, 145(19): 1480-1496. doi: 10.1161/CIRCULATIONAHA.121.057757
[22] Cadrin-Tourigny J, Bosman LP, Nozza A, et al. A new prediction model for ventricular arrhythmias in arrhythmogenic right ventricular cardiomyopathy[J]. Eur Heart J, 2022, 43(32): e1-e9. doi: 10.1093/eurheartj/ehac180
-

计量
- 文章访问数: 173
- 施引文献: 0



 下载:
下载: