Research progress on the relationship between short-chain fatty acids and atherosclerosis
-
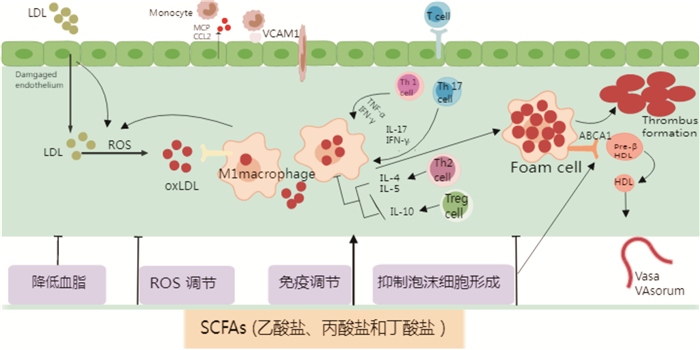
摘要: 动脉粥样硬化(AS)所导致的心脑血管疾病是一类严重危害人类健康的疾病。近年来研究发现,肠道菌群代谢物短链脂肪酸(SCFAs)通过抑制泡沫细胞活性、调节免疫细胞和炎症、抑制氧化应激在AS发病机制中起到重要作用。SCFAs对AS的具体影响及作用机制已得到越来越多的关注。本文就SCFAs的一般特性、SCFAs在AS发展中的作用、通过干预SCFAs防治AS的最新研究进展作一综述。Abstract: Ardio-cerebrovascular diseases caused by atherosclerosis(AS) are a class of diseases that seriously harm human health. Recent studies have found that intestinal flora metabolites short-chain fatty acids(SCFAs) play an important role in the pathogenesis of AS by inhibiting foam cell activity, regulating immune cells and inflammation, and inhibiting oxidative stress. More and more attention has been paid to the specific effects and mechanisms of SCFAs on AS. In this paper, the general characteristics of SCFAs, the role of SCFAs in the development of AS, and the latest research progress on the prevention and treatment of AS through SCFAs intervention are reviewed.
-
Key words:
- atherosclerosis /
- short-chain fatty acids /
- intestinal flora
-

-
[1] Kobiyama K, Ley K. Atherosclerosis[J]. Circ Res, 2018, 123(10): 1118-1120. doi: 10.1161/CIRCRESAHA.118.313816
[2] Lam V, Su J, Koprowski S, et al. Intestinal microbiota determine severity of myocardial infarction in rats[J]. FASEB J, 2012, 26(4): 1727-1735. doi: 10.1096/fj.11-197921
[3] 晏家升, 吕冰洁, 程翔. 肠道菌群调节免疫系统影响心血管疾病的研究进展[J]. 临床心血管病杂志, 2022, 38(8): 614-618. doi: 10.13201/j.issn.1001-1439.2022.08.004
[4] Chakaroun RM, Olsson LM, Bäckhed F. The potential of tailoring the gut microbiome to prevent and treat cardiometabolic disease[J]. Nat Rev Cardiol, 2023, 20(4): 217-235. doi: 10.1038/s41569-022-00771-0
[5] Kimura I, Ichimura A, Ohue-Kitano R, et al. Free fatty acid receptors in health and disease[J]. Physiol Rev, 2020, 100(1): 171-210. doi: 10.1152/physrev.00041.2018
[6] Koh A, De Vadder F, Kovatcheva-Datchary P, et al. From dietary fiber to host physiology: short-chain fatty acids as key bacterial metabolites[J]. Cell, 2016, 165(6): 1332-1345. doi: 10.1016/j.cell.2016.05.041
[7] van der Hee B, Wells JM. Microbial regulation of host physiology by short-chain fatty acids[J]. Trends Microbiol, 2021, 29(8): 700-712. doi: 10.1016/j.tim.2021.02.001
[8] Martin-Gallausiaux C, Marinelli L, Blottière HM, et al. SCFA: mechanisms and functional importance in the gut[J]. Proc Nutr Soc, 2021, 80(1): 37-49. doi: 10.1017/S0029665120006916
[9] Zhao P, Zhao S, Tian J, et al. Significance of gut microbiota and short-chain fatty acids in heart failure[J]. Nutrients, 2022, 14(18): 110.
[10] Chen Y, Xu C, Huang R, et al. Butyrate from pectin fermentation inhibits intestinal cholesterol absorption and attenuates atherosclerosis in apolipoprotein E-deficient mice[J]. J Nutr Biochem, 2018, 56: 175-182. doi: 10.1016/j.jnutbio.2018.02.011
[11] Aguilar EC, Leonel AJ, Teixeira LG, et al. Butyrate impairs atherogenesis by reducing plaque inflammation and vulnerability and decreasing NFκB activation[J]. Nutr Metab Cardiovasc Dis, 2014, 24(6): 606-613. doi: 10.1016/j.numecd.2014.01.002
[12] Lin XL, Xiao LL, Tang ZH, et al. Role of PCSK9 in lipid metabolism and atherosclerosis[J]. Biomed Pharmacother, 2018, 104: 36-44. doi: 10.1016/j.biopha.2018.05.024
[13] Finn AV, Nakano M, Polavarapu R, et al. Hemoglobin directs macrophage differentiation and prevents foam cell formation in human atherosclerotic plaques[J]. J Am Coll Cardiol, 2012, 59(2): 166-177. doi: 10.1016/j.jacc.2011.10.852
[14] Li M, van Esch B, Henricks P, et al. Time and concentration dependent effects of short chain fatty acids on lipopolysaccharide-or tumor necrosis factor α-induced endothelial activation[J]. Front Pharmacol, 2018, 9: 233. doi: 10.3389/fphar.2018.00233
[15] Du Y, Li X, Su C, et al. Butyrate protects against high-fat diet-induced atherosclerosis via up-regulating ABCA1 expression in apolipoprotein E-deficiency mice[J]. Br J Pharmacol, 2020, 177(8): 1754-1772. doi: 10.1111/bph.14933
[16] Li H, Gao Z, Zhang J, et al. Sodium butyrate stimulates expression of fibroblast growth factor 21 in liver by inhibition of histone deacetylase 3[J]. Diabetes, 2012, 61(4): 797-806. doi: 10.2337/db11-0846
[17] Kim MH, Kang SG, Park JH, et al. Short-chain fatty acids activate GPR41 and GPR43 on intestinal epithelial cells to promote inflammatory responses in mice[J]. Gastroenterology, 2013, 145(2): 396-406. e1-10. doi: 10.1053/j.gastro.2013.04.056
[18] Escárcega RO, Lipinski MJ, García-Carrasco M, et al. Inflammation and atherosclerosis: Cardiovascular evaluation in patients with autoimmune diseases[J]. Autoimmun Rev, 2018, 17(7): 703-708. doi: 10.1016/j.autrev.2018.01.021
[19] Tayyeb JZ, Popeijus HE, Mensink RP, et al. Short-Chain Fatty Acids(Except Hexanoic Acid)Lower NF-kB Transactivation, Which Rescues Inflammation-Induced Decreased Apolipoprotein A-I Transcription in HepG2 Cells[J]. Int J Mol Sci, 2020, 21(14): 110.
[20] Kasahara K, Krautkramer KA, Org E, et al. Interactions between Roseburia intestinalis and diet modulate atherogenesis in a murine model[J]. Nat Microbiol, 2018, 3(12): 1461-1471. doi: 10.1038/s41564-018-0272-x
[21] Al-Roub A, Akhter N, Al-Sayyar A, et al. Short chain fatty acid acetate increases TNFα-Induced MCP-1 production in monocytic cells via ACSL1/MAPK/NF-κB Axis[J]. Int J Mol Sci, 2021, 22(14): 110.
[22] Arpaia N, Campbell C, Fan X, et al. Metabolites produced by commensal bacteria promote peripheral regulatory T-cell generation[J]. Nature, 2013, 504(7480): 451-455. doi: 10.1038/nature12726
[23] van den Berg VJ, Vroegindewey MM, Kardys I, et al. Anti-Oxidized LDL antibodies and coronary artery disease: a systematic review[J]. Antioxidants(Basel), 2019, 8(10): 110.
[24] Aguilar EC, Santos LC, Leonel AJ, et al. Oral butyrate reduces oxidative stress in atherosclerotic lesion sites by a mechanism involving NADPH oxidase down-regulation in endothelial cells[J]. J Nutr Biochem, 2016, 34: 99-105. doi: 10.1016/j.jnutbio.2016.05.002
[25] Haghikia A, Zimmermann F, Schumann P, et al. Propionate attenuates atherosclerosis by immune-dependent regulation of intestinal cholesterol metabolism[J]. Eur Heart J, 2022, 43(6): 518-533. doi: 10.1093/eurheartj/ehab644
[26] Petrucci G, Rizzi A, Hatem D, et al. Role of oxidative stress in the pathogenesis of atherothrombotic diseases[J]. Antioxidants(Basel), 2022, 11(7): 110.
[27] Yuan X, Wang L, Bhat OM, et al. Differential effects of short chain fatty acids on endothelial Nlrp3 inflammasome activation and neointima formation: Antioxidant action of butyrate[J]. Redox Biol, 2018, 16: 21-31. doi: 10.1016/j.redox.2018.02.007
[28] Bartolomaeus H, Balogh A, Yakoub M, et al. Short-Chain fatty acid propionate protects from hypertensive cardiovascular damage[J]. Circulation, 2019, 139(11): 1407-1421. doi: 10.1161/CIRCULATIONAHA.118.036652
[29] Threapleton DE, Greenwood DC, Evans CE, et al. Dietary fibre intake and risk of cardiovascular disease: systematic review and meta-analysis[J]. BMJ, 2013, 347: f6879. doi: 10.1136/bmj.f6879
[30] Pagliai G, Russo E, Niccolai E, et al. Influence of a 3-month low-calorie Mediterranean diet compared to the vegetarian diet on human gut microbiota and SCFA: the CARDIVEG Study[J]. Eur J Nutr, 2020, 59(5): 2011-2024. doi: 10.1007/s00394-019-02050-0
[31] Wu H, Esteve E, Tremaroli V, et al. Metformin alters the gut microbiome of individuals with treatment-naive type 2 diabetes, contributing to the therapeutic effects of the drug[J]. Nat Med, 2017, 23(7): 850-858. doi: 10.1038/nm.4345
[32] Mueller NT, Differding MK, Zhang M, et al. Metformin affects gut microbiome composition and function and circulating short-chain fatty acids: a randomized trial[J]. Diabetes Care, 2021, 44(7): 1462-1471. doi: 10.2337/dc20-2257
[33] Yan N, Wang L, Li Y, et al. Metformin intervention ameliorates AS in ApoE-/- mice through restoring gut dysbiosis and anti-inflammation[J]. PLoS One, 2021, 16(7): e0254321. doi: 10.1371/journal.pone.0254321
[34] Chen Y, Shen X, Ma T, et al. Adjunctive Probio-X Treatment Enhances the Therapeutic Effect of a Conventional Drug in Managing Type 2 Diabetes Mellitus by Promoting Short-Chain Fatty Acid-Producing Bacteria and Bile Acid Pathways[J]. mSystems, 2023, 8(1): e0130022. doi: 10.1128/msystems.01300-22
[35] Liu J, Yue S, Yang Z, et al. Oral hydroxysafflor yellow A reduces obesity in mice by modulating the gut microbiota and serum metabolism[J]. Pharmacol Res, 2018, 134: 40-50. doi: 10.1016/j.phrs.2018.05.012
[36] Gao B, Wang R, Peng Y, et al. Effects of a homogeneous polysaccharide from Sijunzi decoction on human intestinal microbes and short chain fatty acids in vitro[J]. J Ethnopharmacol, 2018, 224: 465-473. doi: 10.1016/j.jep.2018.06.006
[37] Guo WL, Pan YY, Li L, et al. Ethanol extract of Ganoderma lucidum ameliorates lipid metabolic disorders and modulates the gut microbiota composition in high-fat diet fed rats[J]. Food Funct, 2018, 9(6): 3419-3431. doi: 10.1039/C8FO00836A
[38] Wei X, Tao J, Xiao S, et al. Xiexin Tang improves the symptom of type 2 diabetic rats by modulation of the gut microbiota[J]. Sci Rep, 2018, 8(1): 3685. doi: 10.1038/s41598-018-22094-2
[39] Kaye DM, Shihata WA, Jama HA, et al. Deficiency of prebiotic fiber and insufficient signaling through gut metabolite-sensing receptors leads to cardiovascular disease[J]. Circulation, 2020, 141(17): 1393-1403. doi: 10.1161/CIRCULATIONAHA.119.043081
[40] Ichim TE, Patel AN, Shafer KA. Experimental support for the effects of a probiotic/digestive enzyme supplement on serum cholesterol concentrations and the intestinal microbiome[J]. J Transl Med, 2016, 14(1): 184. doi: 10.1186/s12967-016-0945-2
[41] Wang Y, Dilidaxi D, Wu Y, et al. Composite probiotics alleviate type 2 diabetes by regulating intestinal microbiota and inducing GLP-1 secretion in db/db mice[J]. Biomed Pharmacother, 2020, 125: 109914. doi: 10.1016/j.biopha.2020.109914
[42] Malik M, Suboc TM, Tyagi S, et al. Lactobacillus plantarum 299v supplementation improves vascular endothelial function and reduces inflammatory biomarkers in men with stable coronary artery disease[J]. Circ Res, 2018, 123(9): 1091-1102. doi: 10.1161/CIRCRESAHA.118.313565
[43] Brandsma E, Kloosterhuis NJ, Koster M, et al. A proinflammatory gut microbiota increases systemic inflammation and accelerates atherosclerosis[J]. Circ Res, 2019, 124(1): 94-100. doi: 10.1161/CIRCRESAHA.118.313234
[44] Battson ML, Lee DM, Li Puma LC, et al. Gut microbiota regulates cardiac ischemic tolerance and aortic stiffness in obesity[J]. Am J Physiol Heart Circ Physiol, 2019, 317(6): H1210-H1220. doi: 10.1152/ajpheart.00346.2019
[45] Fang H, Fu L, Wang J. Protocol for fecal microbiota transplantation in inflammatory bowel disease: a systematic review and meta-analysis[J]. Biomed Res Int, 2018, 2018: 8941340.
-




 下载:
下载: