Imaging manifestations and research progress of radiotherapy-related cardiovascular injury
-
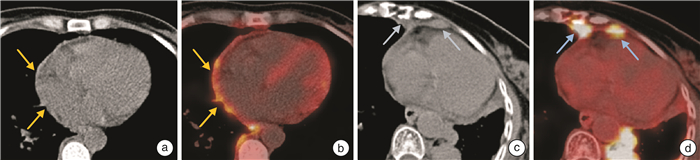
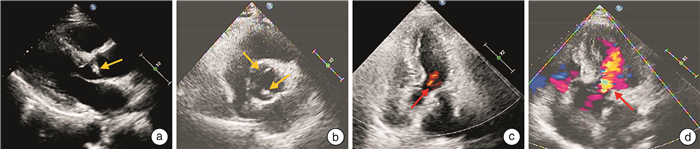
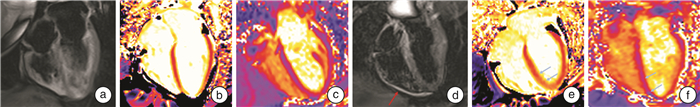
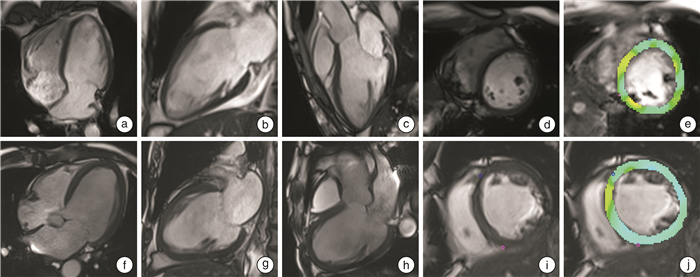
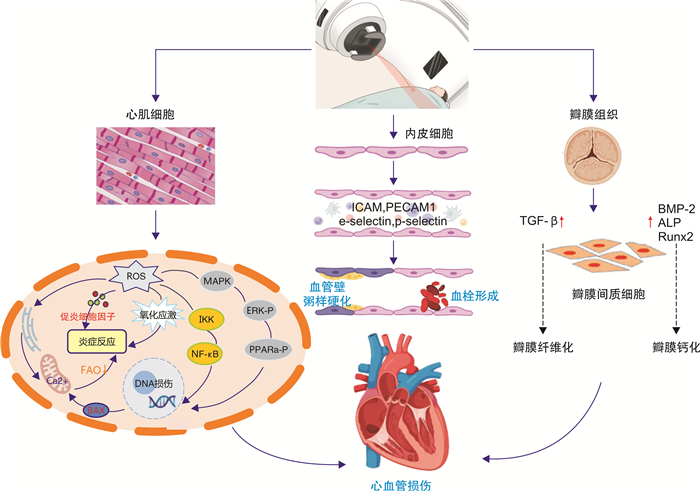
摘要: 放疗作为肿瘤的重要治疗手段,在控制肿瘤进展的同时,也可造成心血管损伤,增加患者远期预后不良的风险。放疗相关心血管损伤表现多样,包括冠心病、心包炎、心瓣膜疾病、心肌病、胸颈部大血管粥样硬化等。影像学检查在放疗相关心血管损伤的诊疗中占有重要地位,可为疾病诊断、病情随访、预后判断提供关键信息。本文针对放疗相关不同类型心血管损伤的影像特征及研究进展进行综述。Abstract: As a vital therapy for tumors, radiotherapy effectively controls the progression of cancer; however, radiotherapy also leads cardiovascular injury and increases the risk of poor long-term prognosis. There are various manifestations of radiotherapy-related cardiovascular injury, including coronary heart disease, pericarditis, valvular heart disease, cardiomyopathy, chest and neck vascular atherosclerosis. Imaging examination plays an important role in the diagnosis and treatment of radiotherapy-related cardiovascular diseases, which provides key information for clinical diagnosis, routine follow-up and prognosis prediction. Therefore, this article reviews the imaging characteristics and research progress according to the types of radiotherapy-related cardiovascular diseases.
-

-
表 1 放疗相关心血管损伤急慢性反应
Table 1. Acute and chronic reactions of radiation-related cardiovascular injuries
疾病类型 急性反应 慢性反应 冠心病 ·作用不明显(放疗6个月后可能出现心肌灌注缺损或心肌运动障碍) ·促进冠心病更早发病
·加重冠心病的严重程度
·放疗后10年以上才出现临床症状(年龄小于50岁的患者多于10年后发病,年龄更大的患者潜伏期更长)
·好发部位为冠脉开口和近段心包炎 ·急性渗出性心包炎相对罕见(多由于接受放疗的肿瘤靠近心脏)
·迟发性急性心包炎发生于放疗后数周内,可表现为有症状的心包炎或无症状的心包积液,心脏填塞较为罕见·慢性心包炎多发生于放疗后数周或者数年后,表现为心包泛增厚、粘连,以及心包积液
·缩窄性心包炎发生率4%~20%,与放疗剂量相关心脏瓣膜疾病 ·作用不明显 ·表现为瓣膜的增厚、纤维化、缩短和钙化
·瓣膜反流比瓣膜狭窄更为常见,好发于二尖瓣与主动脉瓣
·瓣膜狭窄好发于主动脉瓣
·发病率与辐射剂量呈正相关心肌病 ·急性心肌炎可导致心脏运动功能轻度减低或心电图异常 ·心肌纤维化可导致心脏舒张与收缩功能障碍、心律失常
·严重者可发展为限制心肌病甚至心力衰竭颈动脉、主动脉粥样硬化 ·作用不明显 ·血管壁粥样硬化斑块形成,多位于照射范围内
·相比原发性血管粥样硬化,放疗导致的粥样硬化病变长度更长、累及范围更广 -
[1] Zamorano JL, Lancellotti P, Rodriguez Muñoz D, et al. 2016 ESC Position Paper on cancer treatments and cardiovascular toxicity developed under the auspices of the ESC Committee for Practice Guidelines: The Task Force for cancer treatments and cardiovascular toxicity of the European Society of Cardiology(ESC)[J]. Eur Heart J, 2016, 37(36): 2768-2801. doi: 10.1093/eurheartj/ehw211
[2] Lancellotti P, Nkomo VT, Badano LP, et al. Expert consensus for multi-modality imaging evaluation of cardiovascular complications of radiotherapy in adults: a report from the European Association of Cardiovascular Imaging and the American Society of Echocardiography[J]. J Am Soc Echocardiogr, 2013, 26(9): 1013-1032. doi: 10.1016/j.echo.2013.07.005
[3] Atkins KM, Chaunzwa TL, Lamba N, et al. Association of left anterior descending coronary artery radiation dose with major adverse cardiac events and mortality in patients with non-small cell lung cancer[J]. JAMA Oncol, 2021, 7(2): 206-219. doi: 10.1001/jamaoncol.2020.6332
[4] Henson KE, McGale P, Darby SC, et al. Cardiac mortality after radiotherapy, chemotherapy and endocrine therapy for breast cancer: Cohort study of 2 million women from 57 cancer registries in 22 countries[J]. Int J Cancer, 2020, 147(5): 1437-1449. doi: 10.1002/ijc.32908
[5] Atkins KM, Rawal B, Chaunzwa TL, et al. Cardiac radiation dose, cardiac disease, and mortality in patients with lung cancer[J]. J Am Coll Cardiol, 2019, 73(23): 2976-2987. doi: 10.1016/j.jacc.2019.03.500
[6] Meattini I, Poortmans PM, Aznar MC, et al. Association of breast cancer irradiation with cardiac toxic effects: a narrative review[J]. JAMA Oncol, 2021, 7(6): 924-932. doi: 10.1001/jamaoncol.2020.7468
[7] Monte IP, Cameli M, Losi V, et al. Valvular damage[J]. J Cardiovasc Echogr, 2020, 30(Suppl 1): S26-S32.
[8] Wang H, Wei J, Zheng Q, et al. Radiation-induced heart disease: a review of classification, mechanism and prevention [J]. Int J Biol Sci, 2019, 15(10): 2128-2138. doi: 10.7150/ijbs.35460
[9] Levine GN, Bates ER, Blankenship JC, et al. 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions[J]Circulation, 2011, 124(23): e574-e651.
[10] Narula J, Chandrashekhar Y, Ahmadi A, et al. SCCT 2021 Expert Consensus Document on Coronary Computed Tomographic Angiography: A Report of the Society of Cardiovascular Computed Tomography[J]. J Cardiovasc Comput Tomogr, 2021, 15(3): 192-217. doi: 10.1016/j.jcct.2020.11.001
[11] Rosmini S, Aggarwal A, Chen DH, et al. Cardiac computed tomography in cardio-oncology: an update on recent clinical applications[J]. Eur Heart J Cardiovasc Imaging, 2021, 22(4): 397-405. doi: 10.1093/ehjci/jeaa351
[12] ÓHartaigh B, Gransar H, Callister T, et al. Development and validation of a simple-to-use nomogram for predicting 5-, 10-, and 15-year survival in asymptomatic adults undergoing coronary artery calcium scoring[J]JACC Cardiovasc Imaging, 2018, 11(3): 450-458. https://www.cnki.com.cn/Article/CJFDTOTAL-GJGD202405004.htm
[13] 曹丰, 孙婷. 无创影像及智能分析技术在老年冠心病诊疗中的应用[J]. 临床心血管病杂志, 2023, 39(10): 741-744. doi: 10.13201/j.issn.1001-1439.2023.10.001
[14] Tagami T, Almahariq MF, Balanescu DV, et al. Usefulness of coronary computed tomographic angiography to evaluate coronary artery disease in radiotherapy-treated breast cancer survivors[J]. Am J Cardiol, 2021, 143: 14-20. doi: 10.1016/j.amjcard.2020.12.038
[15] Gal R, van Velzen SGM, Hooning MJ, et al. Identification of risk of cardiovascular disease by automatic quantification of coronary artery calcifications on radiotherapy planning CT scans in patients with breast cancer[J]. JAMA Oncol, 2021, 7(7): 1024-1032. doi: 10.1001/jamaoncol.2021.1144
[16] Milgrom SA, Varghese B, Gladish GW, et al. Coronary artery dose-volume parameters predict risk of calcification after radiation therapy[J]. J Cardiovasc Imaging, 2019, 27(4): 268-279. doi: 10.4250/jcvi.2019.27.e38
[17] Yakupovich A, Davison MA, Kharouta MZ, et al. Heart dose and coronary artery calcification in patients receiving thoracic irradiation for lung cancer[J]. J Thorac Dis, 2020, 12(3): 223-231. doi: 10.21037/jtd.2020.01.52
[18] Fu H, Wang X, Diao K, et al. CT compared to MRI for functional evaluation of the right ventricle: a systematic review and meta-analysis[J]Eur Radiol. 2019;29(12): 6816-6828. doi: 10.1007/s00330-019-06228-2
[19] Takx R, Celeng C, Schoepf UJ. CT myocardial perfusion imaging: ready for prime time?[J]. Eur Radiol, 2018, 28(3): 1253-1256. doi: 10.1007/s00330-017-5057-8
[20] Lopez-Mattei JC, Yang EH, Ferencik M, et al. Cardiac computed tomography in cardio-oncology: JACC: CardioOncology Primer[J]. JACC Cardio Oncol, 2021, 3(5): 635-649. doi: 10.1016/j.jaccao.2021.09.010
[21] Tanabe Y, Kido T, Kurata A, et al. Late iodine enhancement computed tomography with image subtraction for assessment of myocardial infarction[J]. Eur Radiol, 2018, 28(3): 1285-1292. doi: 10.1007/s00330-017-5048-9
[22] Wang R, Liu X, Schoepf UJ, et al. Extracellular volume quantitation using dual-energy CT in patients with heart failure: Comparison with 3T cardiac MR[J]. Int J Cardiol, 2018, 268: 236-240. doi: 10.1016/j.ijcard.2018.05.027
[23] Cuomo JR, Javaheri SP, Sharma GK, et al. How to prevent and manage radiation-induced coronary artery disease[J]. Heart, 2018, 104(20): 1647-1653. doi: 10.1136/heartjnl-2017-312123
[24] Pak S, Hawash AA, Linares J, et al. Myocardial damage on SPECT imaging among patients treated with radiotherapy for left-sided breast cancer: Systematic review with meta-analysis and narrative synthesis[J]. J BUON, 2018, 23(4): 910-918.
[25] Edvardsen T, Asch FM, Davidson B, et al. Non-Invasive Imaging in Coronary Syndromes: Recommendations of The European Association of Cardiovascular Imaging and the American Society of Echocardiography, in Collaboration with The American Society of Nuclear Cardiology, Society of Cardiovascular Computed Tomography, and Society for Cardiovascular Magnetic Resonance[J]. J Am Soc Echocardiogr, 2022, 35(4): 329-354. doi: 10.1016/j.echo.2021.12.012
[26] Hendel RC, Friedrich MG, Schulz-Menger J, et al. CMR first-pass perfusion for suspected inducible myocardial ischemia[J], JACC Cardiovasc Imaging, 2016, 9: 1338-1348. doi: 10.1016/j.jcmg.2016.09.010
[27] Machann W, Beer M, Breunig M, et al. Cardiac magnetic resonance imaging findings in 20-year survivors of mediastinal radiotherapy for Hodgkin's disease[J]. Int J Radiat Oncol Biol Phys, 2011, 79(4): 1117-1123. doi: 10.1016/j.ijrobp.2009.12.054
[28] Hsu LY, Jacobs M, Benovoy M, et al. Diagnostic performance of fully automated pixel-wise quantitative myocardial perfusion imaging by cardiovascular magnetic resonance[J]. JACC Cardiovasc Imaging, 2018, 11(5): 697-707. doi: 10.1016/j.jcmg.2018.01.005
[29] Mygind ND, Michelsen MM, Pena A, et al. Coronary microvascular function and myocardial fibrosis in women with angina pectoris and no obstructive coronary artery disease: the iPOWER study[J]. J Cardiovasc Magn Reson, 2016, 18(1): 76. doi: 10.1186/s12968-016-0295-5
[30] El Aidi H, Adams A, Moons KG, et al. Cardiac magnetic resonance imaging findings and the risk of cardiovascular events in patients with recent myocardial infarction or suspected or known coronary artery disease: a systematic review of prognostic studies[J]. J Am CollCardiol, 2014, 63(11): 1031-1045. doi: 10.1016/j.jacc.2013.11.048
[31] Hajhosseiny R, Bustin A, Munoz C, et al. Coronary magnetic resonance angiography: technical innovations leading us to the promised land?[J]. JACC Cardiovasc Imaging, 2020, 13(12): 2653-2672. doi: 10.1016/j.jcmg.2020.01.006
[32] van der Velde N, Janus CPM, Bowen DJ, et al. Detection of subclinical cardiovascular disease by cardiovascular magnetic resonance in lymphoma survivors[J]. JACC Cardio Oncol, 2021, 3(5): 695-706. doi: 10.1016/j.jaccao.2021.09.015
[33] Umezawa R, Ota H, Takanami K, et al. MRI findings of radiation-induced myocardial damage in patients with oesophageal cancer[J]. Clin Radiol, 2014, 69(12): 1273-1279. doi: 10.1016/j.crad.2014.08.010
[34] Burke AM, Yeh C, Kim S, et al. A prospective study of early radiation associated cardiac toxicity following neoadjuvant chemoradiation for distal esophageal cancer[J]. Front Oncol, 2020, 10: 1169. doi: 10.3389/fonc.2020.01169
[35] Lyon AR, López-Fernández T, Couch LS, et al. 2022 ESC Guidelines on cardio-oncology developed in collaboration with the European Hematology Association(EHA), the European Society for Therapeutic Radiology and Oncology(ESTRO)and the International Cardio-Oncology Society(IC-OS)[J]. Eur Heart J, 2022, 43(41): 4229-4361. doi: 10.1093/eurheartj/ehac244
[36] 黄勇. 放射性心血管疾病的研究进展[J]. 中国辐射卫生, 2018, 27(4): 349-353. https://www.cnki.com.cn/Article/CJFDTOTAL-REDI201804017.htm
[37] Alter P, Figiel JH, Rupp TP, et al. MR, CT, and PET imaging in pericardial disease[J]. Heart Fail Rev, 2013, 18(3): 289-306. doi: 10.1007/s10741-012-9309-z
[38] Shim HK, Kim MR, Lee H. Fluorodeoxyglucose positron emission tomography/computed tomography identifying pericardial metastasis from early-stage p16-positive oropharyngeal cancer[J]. Clin Case Rep, 2020, 8(7): 1261-1264. doi: 10.1002/ccr3.2672
[39] Wang H, Wei J, Zheng Q, et al. Radiation-induced heart disease: a review of classification, mechanism and prevention [J]. Int J Biol Sci, 2019, 15(10): 2128-2138. doi: 10.7150/ijbs.35460
[40] Poltavskaya MG, Emelina EI, Avdeev YV, et al. Heart valve injury due to radiation therapy[J]. Kardiologiia, 2019, 59(2S): 56-68. doi: 10.18087/cardio.2656
[41] Shah DJ. 4D Flow CMR: The final frontier in valvular heart disease?[J]. JACC Cardiovasc Imaging, 2021, 14(7): 1367-1368. doi: 10.1016/j.jcmg.2021.03.011
[42] Corrias G, Cocco D, Suri JS, et al. Heart applications of 4D flow[J]. Cardiovasc Diagn Ther, 2020, 10(4): 1140-1149. doi: 10.21037/cdt.2020.02.08
[43] Francone M, Budde RPJ, Bremerich J, et al. CT and MR imaging prior to transcatheter aortic valve implantation: standardisation of scanning protocols, measurements and reporting-a consensus document by the European Society of Cardiovascular Radiology(ESCR)[J]. Eur Radiol, 2020, 30(5): 2627-2650. doi: 10.1007/s00330-019-06357-8
[44] Plana JC, Thavendiranathan P, Bucciarelli-Ducci C, et al. Multi-Modality Imaging in the Assessment of Cardiovascular Toxicity in the Cancer Patient[J]. JACC Cardiovasc Imaging, 2018, 11(8): 1173-1186. doi: 10.1016/j.jcmg.2018.06.003
[45] Ricco A, Slade A, Canada JM, et al. Cardiac MRI utilizing late gadolinium enhancement(LGE)and T1 mapping in the detection of radiation induced heart disease[J]. Cardiooncology, 2020, 6: 6.
[46] Umezawa R, Ota H, Takanami K, et al. MRI findings of radiation-induced myocardial damage in patients with oesophageal cancer[J]. Clin Radiol, 2014, 69(12): 1273-1279. doi: 10.1016/j.crad.2014.08.010
[47] Takagi H, Ota H, Umezawa R, et al. Left Ventricular T1 mapping during chemotherapy-radiation therapy: serial assessment of participants with esophageal cancer[J]. Radiology, 2018, 289(2): 347-354. doi: 10.1148/radiol.2018172076
[48] Tahir E, Azar M, Shihada S, et al. Myocardial injury detected by T1 and T2 mapping on CMR predicts subsequent cancer therapy-related cardiac dysfunction in patients with breast cancer treated by epirubicin-based chemotherapy or left-sided RT[J]. Eur Radiol, 2022, 32(3): 1853-1865. doi: 10.1007/s00330-021-08260-7
[49] 李新立, 郑旭辉, 唐愿. 心脏磁共振成像在心力衰竭中的应用[J]. 临床心血管病杂志, 2023, 39(4): 251-254. doi: 10.13201/j.issn.1001-1439.2023.04.003
[50] Gavara J, Rodriguez-Palomares JF, Valente F, et al. Prognostic value of strain by tissue tracking cardiac magnetic resonance after ST-segment elevation myocardial infarction[J]. JACC Cardiovasc Imaging, 2018, 11(10): 1448-1457. doi: 10.1016/j.jcmg.2017.09.017
[51] Merkx R, Leerink JM, Feijen E, et al. Echocardiography protocol for early detection of cardiac dysfunction in childhood cancer survivors in the multicenter DCCSS LATER 2 CARD study: Design, feasibility, and reproducibility[J]. Echocardiography, 2021, 38(6): 951-963. doi: 10.1111/echo.15081
[52] Lo Q, Hee L, Batumalai V, et al. Subclinical cardiac dysfunction detected by strain imaging during breast irradiation with persistent changes 6 weeks after treatment[J]. Int J Radiat Oncol Biol Phys, 2015, 92(2): 268-276. doi: 10.1016/j.ijrobp.2014.11.016
[53] Nagueh SF. left ventricular diastolic function: understanding pathophysiology, diagnosis, and prognosis with echocardiography[J]. JACC Cardiovasc Imaging, 2020, 13(1 Pt 2): 228-244.
[54] Strüder D, Hellwig S, Rennau H, et al. Screening for irradiation vasculopathy by intima-media thickness sonography in head and neck cancer patients[J]. Eur Arch Otorhinolaryngol, 2021, 278(6): 2017-2026. doi: 10.1007/s00405-020-06301-3
[55] Fernández-Alvarez V, López F, Suárez C, et al. Radiation-induced carotid artery lesions[J]. Strahlenther Onkol, 2018, 194(8): 699-710. doi: 10.1007/s00066-018-1304-4
[56] Li Y, Kwong DL, Wu VW, et al. Computer-assisted ultrasound assessment of plaque characteristics in radiation-induced and non-radiation-induced carotid atherosclerosis[J]. Quant Imaging Med Surg, 2021, 11(6): 2292-2306. doi: 10.21037/qims-20-1012
[57] Jurcut R, Ector J, Erven K, et al. Radiotherapy effects on systolic myocardial function detected by strain rate imaging in a left-breast cancer patient[J]. Eur Heart J, 2007, 28(24): 2966. doi: 10.1093/eurheartj/ehm311
[58] Cheng YJ, Nie XY, Ji CC, et al. Long-term cardiovascular risk after radiotherapy in women with breast cancer[J]. J Am Heart Assoc, 2017, 6(5): e005633. doi: 10.1161/JAHA.117.005633
-




 下载:
下载: