Quantitative evaluation of mitral valve geometry with moderate or severe mitral regurgitation by real-time three-dimensional transesophageal echocardiography
-
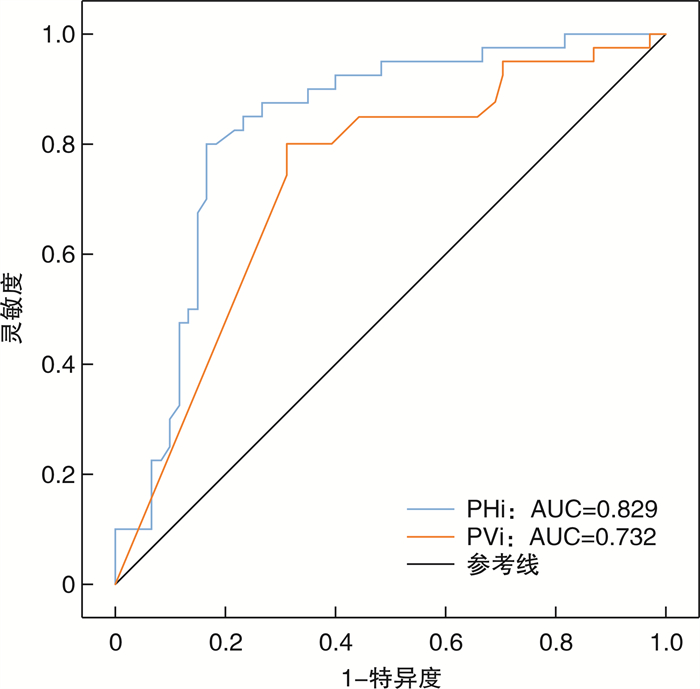
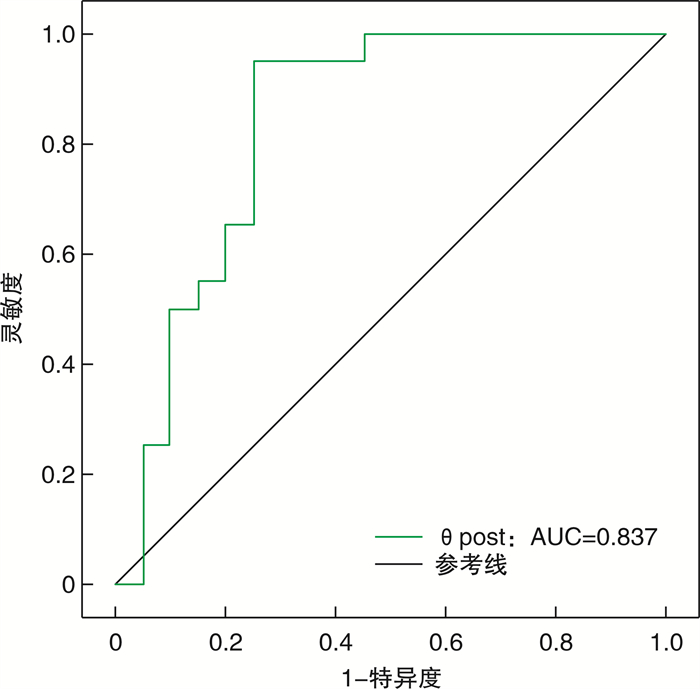
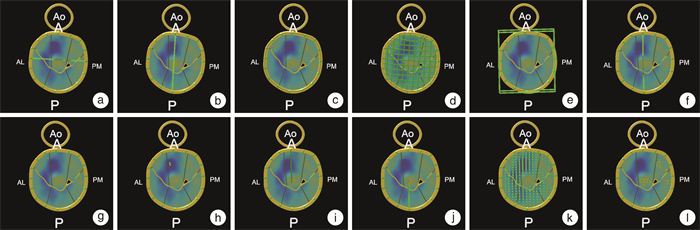
摘要: 目的 探讨实时三维经食管超声心动图(RT-3D-TEE)定量评价不同病因及病理生理机制下慢性中重度二尖瓣反流(MR)的二尖瓣几何结构。方法 回顾性分析2021年5月—2024年4月于四川省人民医院行经胸超声心动图(TTE)和RT-3D-TEE检查的60例中重度退行性二尖瓣反流患者(DMR组)、20例中重度心室功能性二尖瓣反流患者(V-FMR组)、20例中重度心房功能性二尖瓣反流患者(A-FMR组),18例经TTE及RT-3D-TEE检查未发现心脏病变患者为对照组,应用Qlab 13.0 MVN软件脱机分析获得以下二尖瓣装置几何结构参数:瓣环前后径(APd)、瓣环前外后内侧径(ALPMd)、瓣环面积(AA)、瓣环周长(AC)、瓣环高度(AH)、瓣环非平面角(NPA)、主动脉瓣口-二尖瓣环夹角(θa-m)、瓣叶总面积(TLA)、瓣叶脱垂高度(PH)、瓣叶脱垂体积(PV)、瓣叶穹窿高度(TH)、瓣叶穹窿体积(TV)、前叶角(θant)、后叶角(θpost),其中PH、PV、TH、TV经体表面积标化得到瓣叶脱垂高度指数(PHi)、瓣叶脱垂体积指数(PVi)、瓣叶穹窿高度指数(THi)、瓣叶穹窿体积指数(TVi),计算瓣环高度与连合宽度比值(AH/CW)、瓣叶与瓣环面积比值(TLA/AA),比较4组间二尖瓣几何结构差异,分析二尖瓣参数区分不同病因中重度MR的效能。结果 与对照组相比,中重度MR组APd、AC、AA、TLA、NPA、THi、TVi均显著增大,其中DMR组PHi、PVi显著增大,DMR组与A-FMR组ALPMd显著增大,AH、AH/CW显著减小(P < 0.05);与V-FMR相比,A-FMR组AH、AH/CW、θpost、THi、TVi显著减小,PHi、PVi显著增大(P < 0.05)。多因素logistic回归分析显示PHi、PVi有助于区分中重度DMR与FMR,其中PHi(截断值为0.918 mm/m2)所对应的ROC曲线下面积最大,为0.829,灵敏度为82.0%,特异度为82.5%;θpost(截断值为29.5°)有助于区分中重度V-FMR与A-FMR,曲线下面积为0.837,灵敏度为95%,特异度为75%。结论 RT-3D-TEE可以评价不同病因及病理生理机制下慢性中重度MR患者的二尖瓣几何结构差异,其中PHi、PVi有助于区分中重度DMR和FMR,θpost有助于区分中重度V-FMR和A-FMR,为临床MR诊断和个体化治疗方案的选择提供影像学依据。Abstract: Objective This study aims to evaluate mitral valve geometry in patients with chronic moderate and severe mitral regurgitation(MR) of varying etiologies and pathophysiological mechanisms using real-time three-dimensional transesophageal echocardiography(RT-3D-TEE).Methods A retrospective study was performed for 60 patients with moderate and severe degenerative mitral regurgitation(DMR group), 20 patients with moderate and severe ventricular functional mitral regurgitation(V-FMR group), 20 patients with moderate and severe atrial functional mitral regurgitation(A-FMR group), and 18 patients with no cardiac lesions, all examined using TTE examination at Sichuan Provincial People's Hospital between May 2021 and April 2024. The mitral valve geometry parameters were obtained through offline analysis of QLAB 13.0 MVN software. The parameters measured included anterior-posterior diameter(APd), anterolateral posteriormedial diameter(ALPMd), annular area(AA), annular circumference(AC), annular height(AH), non-planarity angle(NPA), aortic-mitral angle(θa-m), total leaflet area(TLA), leaflet prolapse height(PH), leaflet prolapse volume(PV), leaflet tenting height(TH), leaflet tenting volume(TV). PH, PV, TH, and TV were standardized by body surface area to obtain leaflet prolapse height index(PHi), leaflet prolapse volume index(PVi), leaflet tenting height index(THi) and leaflet tenting volume index(TVi). Computing annular height/ commissural width(AH/CW), total leaflet area/ annular area(TLA/AA). The differences in mitral valve geometry among the four groups were compared, and the efficacy of mitral valve parameters in distinguishing moderate to severe MR of different etiologies and pathophysiological mechanisms was analyzed.Results Compared with the control group, APd, AC, AA, TLA, NPA, THi and TVi were significantly increased in moderate and severe MR Group(P < 0.05). In the DMR group, PHi and PVi were significantly increased, and ALPMd was significantly increased in both the DMR group and A-FMR group, while AH and AH/CW were decreased significantly(P < 0.05). Compared with the V-FMR group, AH, AH/CW, θpost, THi and TVi were significantly reduced, while PHi and PVi were significantly increased in the A-FMR group(P < 0.05). Multivariate logistic regression analysis indicated that PHi and PVi were effective in distinguishing moderate and severe DMR from FMR, with PHi(cut-off value was 0.918 mm/m2) having the largest area under the ROC curve of 0.829, with a sensitivity of 82.0% and a specificity of 82.5%. θpost(cut-off value 29.5) was effective in distinguish moderate and severe V-FMR from A-FMR, with an area under the ROC curve of 0.837 with a sensitivity of 95% and a specificity of 75%.Conclusion RT-3D-TEE effectively evaluates difference in mitral valve geometry among patients with chronic moderate and severe mitral regurgitation of different causes and different etiologies and pathophysiological mechanisms. PHi and PVi are helpful for distinguishing moderate and severe DMR and FMR, while θpost is useful for distinguishing between moderate and severe V-FMR and A-FMR, thus providing imaging basis for clinic MR diagnosis and treatment planning.
-

-
表 1 4组临床基本资料及TTE基本参数比较
Table 1. The clinical baseline data and basic parameters of TTE
X±S, M(P25, P75) 项目 对照组(18例) DMR(60例) V-FMR(20例) A-FMR(20例) F/Z P 年龄/岁 53.42±11.94 70.28±8.941) 65.15±9.791)2) 72.80±7.081)3) 18.675 < 0.001 身高/cm 163.74±7.63 158.43±9.26 162.60±5.52 159.45±9.34 2.548 0.059 体重/kg 62.11±8.27 55.90±10.57 59.10±8.42 54.40±10.47 2.685 0.050 BMI/(kg/m2) 23.19±2.93 22.13±2.90 22.27±2.35 21.28±2.80 1.530 0.211 BSA/m2 1.64±0.13 1.53±0.18 1.59±0.13 1.52±0.18 1.315 0.192 LAAPd/mm 33.32±8.42 48.51±11.461) 47.75±8.751) 55.00±12.711)2)3) 14.096 < 0.001 LALRd/mm 34.11±12.12 50.77±12.001) 45.30±11.081) 55.90±17.411)3) 11.066 < 0.001 LAUDd/mm 48.95±11.76 64.84±13.141) 59.45±14.591) 70.00±13.971)3) 9.624 < 0.001 LVEDd/mm 44.05±6.92 49.34±10.551) 61.65±9.121)2) 49.45±10.181)3) 11.777 < 0.001 LVESd/mm 35.63±6.86 38.97±8.80 53.40±9.731)2) 41.10±9.413) 16.674 < 0.001 RALRd/mm 32.26±5.83 40.07±10.271) 40.10±8.611) 46.50±11.051)2)3) 7.179 < 0.001 RAUDd/mm 44.00(38.00,47.00) 49.00(43.00,57.00)1) 52.5.00(49.25,58.75)1) 59.00(53.00,67.50)1)2) 25.360 < 0.001 RVAPd/mm 25.26±3.59 25.38±2.20 22.05±3.46 23.80±4.36 0.287 0.835 AV/(m/s) 1.20±0.26 1.30±0.40 1.27±0.37 1.15±0.38 0.958 0.415 MV E/(m/s) 0.82(0.68,0.86) 1.47(1.03,1.80)1) 1.12(0.98,1.46)1)2) 1.17(1.01,1.53)1) 36.597 < 0.001 MV A/(m/s) 0.61(0.56,0.69) 0.77(0.62,1.03)1) 0.75(0.62,0.83) 0.56(0.44,0.80)2) 15.773 0.001 MV E/A 1.36(1.20,1.51) 1.79(1.41,2.35)1) 1.73(1.27,1.99)1) 2.15(1.68,2.86)1)2)3) 17.861 < 0.001 MV e’average /(m/s) 0.11±0.03 0.09±0.031) 0.07±0.021)2) 0.10±0.043) 7.114 < 0.001 MV a average /(m/s) 0.08(0.06,0.08) 0.08(0.06,0.08) 0.05(0.04,0.07)1)2) 0.05(0.03,0.05)1)2) 29.309 < 0.001 MV E/e’ 6.92(5.93,9.06) 16.87(12.38,22.11)1) 17.42(13.13,20.30)1) 14.43(11.01,16.61)1)2) 38.492 < 0.001 MVAlrd /mm 28.00(26.00,31.00) 32.00(29.00,37.00)1) 34.00(32.50,36.50)1) 36.50(32.50,39.50)1)2) 23.986 < 0.001 VCW/cm 0.59±0.19 0.66±0.16 0.57±0.17 1.360 0.261 EROA/cm2 0.62±0.33 0.51±0.33 0.41±0.232) 3.981 0.022 RVol/mL 88.82±37.42 76.15±45.99 61.85±30.602) 3.666 0.029 LVEF/% 0.61±0.07 0.61±0.11 0.36±0.121)2) 0.51±0.141)2)3) 26.836 < 0.001 BMI:体重指数;BSA:体表面积;MV E:舒张早期二尖瓣前向血流E峰;MV A:舒张晚期二尖瓣前向血流A峰;MV e’average:二尖瓣瓣环侧壁和室间隔e’峰均值;MV a average:二尖瓣瓣环侧壁和室间隔a峰均值;VCW:缩流颈宽度;EROA:有效反流口面积;RVol:反流容积。与对照组比较,1)P < 0.05;与DMR组比较,2)P < 0.05;与V-FMR组比较,3)P < 0.05。 表 2 对照组、DMR、V-FMR与A-FMR组二尖瓣结构参数比较
Table 2. Comparison of mitral valve structural parameters in control group, DMR, V-FMR and A-FMR group
X±S, M(P25, P75) 二尖瓣参数 对照组(18例) DMR(60例) V-FMR(20例) A-FMR(20例) F/Z值 P值 ALPMd/mm 32.86±2.59 36.17±5.021) 34.70±6.11 36.86±4.671) 3.076 0.030 APd/mm 27.76±3.53 32.87±5.131) 32.08±5.291) 34.61±5.961) 6.663 < 0.001 AH/mm 6.99±1.81 5.46±1.791) 6.57±1.822) 5.37±1.641)3) 5.245 0.002 AC/mm 102.80 (97.65,102.80) 112.70 (104.70,112.70)1) 115.80 (104.85,115.85)1) 118.30 (113.70,118.35)1) 16.644 0.001 AA/mm2 789.56±123.55 1011.29±267.901) 1028.49±295.301) 1109.41±295.131) 5.400 0.002 AH/CW/% 22.90±7.19 18.25±5.621) 22.67±6.342) 17.02±5.831)3) 5.838 < 0.001 NPA/° 113.37±12.58 133.27±21.421) 132.30±16.061) 135.01±21.201) 6.003 < 0.001 TLA/mm2 852.36±145.06 1141.51±313.091) 1166.06±349.591) 1175.74±309.891) 5.457 0.002 θant/° 19.43±6.75 18.32±8.94 20.95±6.34 17.32±8.67 0.780 0.507 θpost/° 27.70±11.04 30.40±19.62 45.69±9.531)2) 28.34±14.333) 5.655 0.001 θa-m/° 127.99±10.59 128.24±13.23 135.57±12.141) 127.68±15.14 1.848 0.142 THi/(mm/m2) 2.57±1.25 4.23±2.231) 5.43±1.681)2) 3.29±2.491)3) 6.561 < 0.001 TVi/(mL/m2) 0.65±0.44 1.11±1.051) 1.92±1.191)2) 0.97±0.731)3) 8.643 < 0.001 PHi/(mm/m2) 0.48±0.45 2.52±1.791) 0.37±0.282) 1.07±1.072)3) 19.658 < 0.001 PVi/(mL/m2) 0.02±0.05 0.25±0.351) 0.00±0.012) 0.15±0.303) 5.754 0.001 TLA/AA/% 135.99±17.06 142.65±28.98 151.62±44.14 134.98±30.72 1.240 0.299 THi:瓣叶穹窿高度指数;TVi:瓣叶穹窿体积指数;PHi:瓣叶脱垂高度指数;PVi:瓣叶脱垂体积指数。与对照组比较,1)P < 0.05;与DMR组比较,2)P < 0.05;与V-FMR组比较,3)P < 0.05。 表 3 区分中重度MR的二元logistic回归分析
Table 3. Binary logistic regression analysis to distinguish between moderate to severe MR
类型 二尖瓣参数 单因素 多因素 β OR(95%CI) P β OR(95%CI) P DMR/FMR NPA 0.021 1.021(1.001~1.042) 0.039 TVi -0.645 0.524(0.325~0.845) 0.008 PHi 1.140 3.126(1.860~5.253) < 0.001 2.221 9.220(3.457~24.591) < 0.001 PVi 2.842 17.149(1.644~178.850) 0.018 -6.235 0.002(0.000~0.081) 0.003 V-FMR/A-FMR AH -0.541 0.582(3.383~0.885) 0.011 AH/CW -16.310 0.001(0.000~0.031) 0.013 θpost -0.112 0.757(0.531~0.080) 0.001 -0.278 0.894(0.836~0.956) < 0.001 NPA 0.069 1.071(1.024~1.120) 0.003 THi -0.399 0.671(0.477~0.944) 0.022 TVi -0.741 0.477(0.234~0.970) 0.041 PHi 2.265 9.635(1.339~69.311) 0.024 表 4 观察者内和观察者间的可重复性
Table 4. Intra-and inter-observer reproducibility
项目 ICC(95%CI) 观察者间 观察者内 PHi 0.853(0.376~0.964) 0.793(0.245~0.927) PVi 0.773(0.350~0.937) 0.868(0.482~0.967) θpost 0.895(0.600~0.954) 0.738(0.382~0.866) -
[1] 潘文志, 周达新, 葛均波. 中国二尖瓣反流患者人群数量的估测[J]. 中国胸心血管外科临床杂志, 2021, 28(5): 495-498.
[2] Tang Z, Fan YT, Wang Y, et al. Mitral annular and left ventricular dynamics in atrial functional mitral regurgitation: a three-dimensional and speckle-tracking echocardiographic study[J]. J Am Soc Echocardiogr, 2019, 32(4): 503-513. doi: 10.1016/j.echo.2018.11.009
[3] 陈宇娇, 刘昕. 经胸实时三维超声心动图评价不同程度缺血性二尖瓣反流患者的二尖瓣构型[J]. 中国循证心血管医学杂志, 2021, 13(2): 178-181, 185.
[4] Cimino S, Guarracino F, Valenti V, et al. Echocardiography and correction of mitral regurgitation: an unbreakable link[J]. Cardiology, 2020, 145(2): 110-120. doi: 10.1159/000504248
[5] Mesi O, Gad MM, Crane AD, et al. Severe atrial functional mitral regurgitation: clinical and echocardiographic characteristics, management and outcomes[J]. JACC Cardiovasc Imaging, 2021, 14(4): 797-808. doi: 10.1016/j.jcmg.2021.02.008
[6] 中国医师协会超声分会超声心动图专业委员会, 中华医学会超声医学分会超声心动图学组, 中华医学会心血管病分会结构性心脏病学组, 等. 二尖瓣反流介入治疗的超声心动图评价中国专家共识[J]. 中国介入心脏病学杂志, 2019, 27(1): 6-12.
[7] Uno G, Omori T, Shimada S, et al. Differences in mitral valve geometry between atrial and ventricular functional mitral regurgitation in patients with atrial fibrillation: a 3D transoesophageal echocardiography study[J]. Eur Heart J Cardiovasc Imaging, 2021, 22(10): 1106-1116. doi: 10.1093/ehjci/jeab130
[8] Bai WJ, Chen Y, Zhong Y, et al. Assessment of mitral valve geometry in nonvalvular atrial fibrillation patients with or without ventricular dysfunction: insights from high volume rate three-dimensional transesophageal echocardiography[J]. Int J Cardiovasc Imaging, 2023, 39(12): 2427-2436. doi: 10.1007/s10554-023-02940-9
[9] Essayagh B, Mantovani F, Benfari G, et al. Mitral annular disjunction of degenerative mitral regurgitation: three-dimensional evaluation and implications for mitral repair[J]. J Am Soc Echocardiogr, 2022, 35(2): 165-175. doi: 10.1016/j.echo.2021.09.004
[10] Antoine C, Mantovani F, Benfari G, et al. Pathophysiology of degenerative mitral regurgitation: new 3-dimensional imaging insights[J]. Circ Cardiovasc Imaging, 2018, 11(1): e005971. doi: 10.1161/CIRCIMAGING.116.005971
[11] Kim DH, Heo R, Handschumacher MD, et al. Mitral valve adaptation to isolated annular dilation: insights into the mechanism of atrial functional mitral regurgitation[J]. JACC Cardiovasc Imaging, 2019, 12(4): 665-677. doi: 10.1016/j.jcmg.2017.09.013
[12] 王柳青, 宋宏宁, 曹省, 等. 实时三维超声定量评估功能性二尖瓣反流二尖瓣装置形态学及动力学的临床研究[J]. 中华超声影像学杂志, 2023, 32(8): 656-663.
[13] 赵苗, 骆志玲, 沈艳, 等. 三维超声心动图定量评价退行性二尖瓣反流瓣环动态变化[J]. 中华超声影像学杂志, 2022, 31(1): 19-24.
[14] van Wijngaarden SE, Kamperidis V, Regeer MV, et al. Three-dimensional assessment of mitral valve annulus dynamics and impact on quantification of mitral regurgitation[J]. Eur Heart J Cardiovasc Imaging, 2018, 19(2): 176-184. doi: 10.1093/ehjci/jex001
[15] Ronco D, Buttiglione G, Garatti A, et al. Biology of mitral valve prolapse: from general mechanisms to advanced molecular patterns-a narrative review[J]. Front Cardiovasc Med, 2023, 10: 1128195. doi: 10.3389/fcvm.2023.1128195
[16] 耿佳琪, 王岳恒, 张佳美, 等. 实时三维经食管超声心动图对二尖瓣脱垂瓣器结构与反流程度的定量研究[J]. 分子影像学杂志, 2022, 45(4): 526-532.
[17] Mantegazza V, Gripari P, Tamborini G, et al. 3D echocardiography in mitral valve prolapse[J]. Front Cardiovasc Med, 2022, 9: 1050476.
[18] Viani GM, Leo LA, Borruso MG, et al. Mitral annulus morphometry in degenerative mitral regurgitation phenotypes[J]. Echocardiography, 2020, 37(4): 612-619. doi: 10.1111/echo.14647
[19] Morningstar JE, Gensemer C, Moore R, et al. Mitral valve prolapse induces regionalized myocardial fibrosis[J]. J Am Heart Assoc, 2021, 10(24): e022332. doi: 10.1161/JAHA.121.022332
[20] 赵丹清, 张付涛, 刘晓洁, 等. 心房颤动合并中重度功能性二尖瓣反流: 导管消融或药物治疗临床疗效的对比研究[J]. 临床心血管病杂志, 2021, 37(10): 925-930. https://lcxxg.whuhzzs.com/article/doi/10.13201/j.issn.1001-1439.2021.10.011
[21] 赵丹清, 张付涛, 刘晓洁, 等. 心房颤动合并功能性二尖瓣反流的危险因素分析及导管消融的影响[J]. 临床心血管病杂志, 2022, 38(5): 368-372. https://lcxxg.whuhzzs.com/article/doi/10.13201/j.issn.1001-1439.2022.05.007
[22] Deferm S, Bertrand PB, Verhaert D, et al. Mitral annular dynamics in AF versus sinus rhythm: novel insights into the mechanism of AFMR[J]. JACC Cardiovasc Imaging, 2022, 15(1): 1-13. doi: 10.1016/j.jcmg.2021.05.019
-




 下载:
下载: