Evaluation of left ventricular systolic function in amateur Marathon runners through ECG mode combined with two-dimensional speckle tracking technique
-
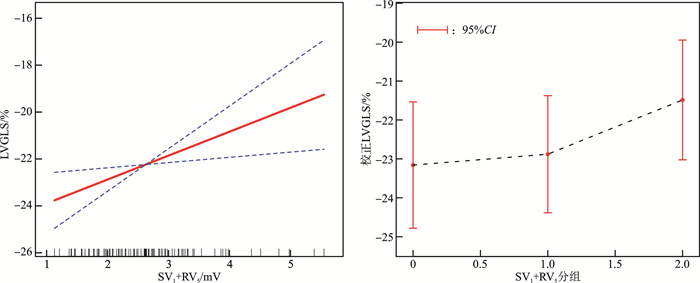
摘要: 目的 探讨业余马拉松跑者心电图SV1+RV5水平与左心室整体纵向应变(global longitudinal strain,GLS)的相关性,评价业余马拉松跑者早期左心室收缩功能。方法 选取2022年9月—2023年9月于常州市第一人民医院超声心动室检查的102位业余马拉松跑者,收集及记录临床资料,采集心电图检查资料,记录受检者SV1+RV5、RaVL+SV3,获取室间隔厚度(interventricular septal thickness,IVST)、左心室舒张末期内径(left ventricular end-diastolic diameter,LVEDD)、左心室后壁厚度(left ventricular posterior wall thickness,LVPWT)、左心室质量指数(left ventricular mass index,LVMI)、左心室射血分数(left ventricular ejection fraction,LVEF)。应用二维斑点追踪成像(two-dimensional speckle tracking imaging,2D-STI)技术获取所有受检者的左心室整体纵向应变值(global longitudinal strain,GLS)。102位业余马拉松跑者按心电图SV1+RV5值的从小到大排列,再按入组人数三分位分组,其中低位组34例、中位组33例、高位组35例。比较各组一般临床资料。采用线性回归分析各参数与GLS的关系。使用广义相加模型(generalized additive model,GAM)分析SV1+RV5与GLS的关系。结果 3组间性别、吸烟史、饮酒史、高血压史、体表面积(body surface area,BSA)、LVMI、SV1+RV5、LVEDD、IVST、LVPWT、GLS均差异有统计学意义(均P < 0.05)。线性回归分析显示,SV1+RV5与GLS独立相关,且随着SV1+RV5的升高,GLS也逐渐升高(P < 0.05)。曲线拟合显示SV1+RV5与GLS呈现正相关。结论 马拉松跑者的左心室GLS与SV1+RV5独立相关,且随着SV1+RV5的升高,GLS也逐渐升高。将两者结合可早期发现左心室收缩功能的异常,这对于预防不良心血管病事件的发生有积极的作用。Abstract: Objective To investigate the correlation between the level of SV1+RV5 in electrocardiogram and the global longitudinal strain(GLS) of left ventricle, and evaluate early left ventricular systolic function in amateur Marathon runners.Methods A total of 102 amateur Marathon runners were selected for echocardiography examination in The First People's Hospital of Changzhou from December 2019 to December 2022. Clinical data were collected and recorded, ECG data were collected, and the value of SV1+RV5, RaVL+SV3 of the subjects were recorded. Interventricular septal thickness(IVST), left ventricular end-diastolic diameter(LVEDD), left ventricular posterior wall thickness(LVPWT), left ventricular mass index(LVMI), left ventricular ejection fraction(LVEF). Two-dimensional speckle tracking imaging(2D-STI) technique was applied to obtain global longitudinal strain(GLS). Divide the 102 amateur marathon runners into tertiles based on the ECG SV1+RV5 value from the smallest to the largest, and then according to the number of participants, with low group of 34, middle group of 33, high group of 35. General data among the three groups were compared. The relationship between each parameter and GLS was analyzed by linear regression. Generalized additive model(GAM) was used to analyze the relationship between GLS and SV1+RV5.Results There were statistically significant differences among the three groups in gender, total horse participation times, best half-horse performance, smoking history, drinking history, hypertension history, systolic blood pressure, BSA, LVMI, SV1+RV5, LVEDD, IVST, LVPWT, and GLS(all P < 0.05). Linear regression analysis showed that there was an independent correlation between SV1+RV5 and GLS, and with the increase of SV1+RV5, the GLS value also gradually increased(P < 0.05). Curve fitting showed that SV1+RV5 was positively correlated with GLS.Conclusion The left ventricular GLS of Marathon runners is independently correlated with SV1+RV5, and with the increase of SV1+RV5, the GLS value also gradually increases. The combination of the two can detect the abnormal left ventricular systolic function early, which is crucial for preventing the occurrence of adverse cardiovascular events.
-

-
表 1 3组临床资料比较
Table 1. Comparison of clinical data among the three groups
例(%), X±S 项目 低位组(34例) 中位组(33例) 高位组(35例) P SV1+RV5/mV < 2.190 2.190~2.760 >2.760 年龄/岁 46.412±7.165 45.152±8.348 48.229±7.413 0.253 男性 10(29.412) 23(69.697) 28(80.000) < 0.001 跑龄 0.867 < 1年 2(5.882) 1(3.125) 1(2.857) ≥1~ < 3年 16(47.059) 11(34.375) 14(40.000) ≥3~ < 6年 10(29.412) 15(46.875) 14(40.000) ≥6年 6(17.647) 5(15.625) 6(17.143) 平均月跑量 0.138 < 100 km 14(41.176) 8(24.242) 4(11.429) ≥100~ < 200 km 10(29.412) 12(36.364) 17(48.571) ≥200~ < 300 km 9(26.471) 12(36.364) 11(31.429) ≥300 km 1(2.941) 1(3.030) 3(8.571) 吸烟史 1(2.941) 9(27.273) 7(20.000) 0.023 饮酒史 4(11.765) 7(21.212) 14(40.000) 0.021 高血压史 5(14.706) 2(6.061) 11(31.429) 0.020 糖尿病史 1(2.941) 0 1(2.857) 0.614 BSA/m2 1.643±0.170 1.743±0.172 1.728±0.150 0.029 LVMI/(g/m2) 83.002±10.727 89.038±17.963 99.336±20.637 < 0.001 BMI/(kg/m2) 22.321±2.246 23.530±2.512 22.852±2.312 0.115 LVEDD/mm 47.676±3.273 49.212±3.655 50.200±4.050 0.019 IVST/mm 8.529±0.706 8.970±0.883 9.571±1.357 < 0.001 LVPWT/mm 8.471±0.662 8.909±0.805 9.314±1.157 < 0.001 LVEF/% 64.735±1.814 64.697±2.756 64.171±2.728 0.572 GLS/% -23.000±1.934 -22.400±2.281 -21.026±2.475 0.001 SV1+RV5/mV 1.765±0.285 2.517±0.176 3.597±0.797 < 0.001 RaVL+SV3/mV 0.860±0.465 0.888±0.486 1.019±0.645 0.431 注:1 mmHg=0.133 kPa。 表 2 各参数与左心室GLS的线性回归分析
Table 2. Parameters and left ventricular GLS analyzed by linear regression analysis
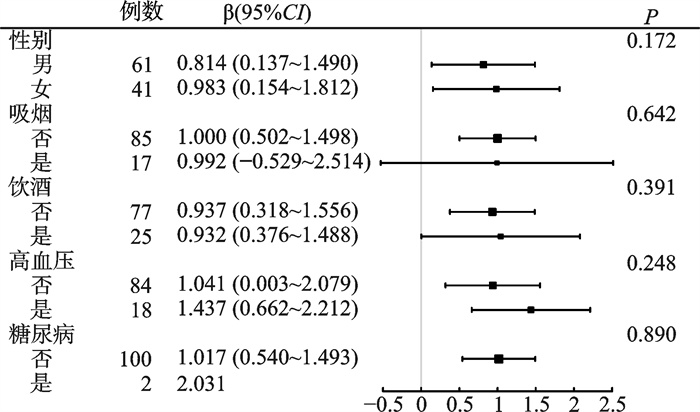
自变量 β(95%CI) P 年龄 0.02(-0.03~0.08) 0.400 性别(男性) -1.39(-2.29~-0.48) 0.003 LVMI 0.09(-0.01~0.03) 0.438 LVEDD 0.03(-0.08~0.15) 0.603 IVST 0.41(0.02~0.79) 0.041 LVPWT 0.51(0.03~0.99) 0.031 LVEF -0.11(-0.29~0.06) 0.062 SV1+RV5 1.03(0.56~1.43) < 0.001 RaVL+SV3 0.27(-0.53~1.08) 0.508 表 3 SV1+RV5与GLS的相关性分析
Table 3. Correlation analysis between SV1+RV5 and GLS
模型1 模型2 模型3 β(95%CI) P β(95%CI) P β(95%CI) P SV1+RV5 0.998(0.562~1.433) < 0.000 1 0.891(0.424~1.357) < 0.000 1 0.873(0.332~1.413) 0.002 SV1+RV5分组 低位组 参考 参考 参考 中位组 1.364(0.369~2.358) 0.008 1.227(0.202~2.252) 0.021 1.081(0.007~2.155) 0.051 高位组 1.974(0.994~2.954) < 0.000 1 1.720(0.706~2.733) 0.001 1.595(0.454~2.735) 0.007 -
[1] 张承铎, 徐顺霖, 高炜. 马拉松运动的心脏安全性与风险防范[J]. 中华心血管病杂志, 2020, 48(2): 100-103.
[2] Predel H. Marathon run: cardiovascular adaptation and cardiovascular risk[J]. Eur Heart J, 2014, 35(44): 3091-3098. doi: 10.1093/eurheartj/eht502
[3] 盛小花, 游江军, 李琳. 心室舒张末期直径比在高海拔汉族、藏族、回族成人先天性心脏病相关肺动脉高压中的研究[J]. 临床心血管病杂志, 2022, 38(4): 323-327. doi: 10.13201/j.issn.1001-1439.2022.04.014
[4] 肖克凡, 董广新. 我国马拉松赛选手猝死事件调查研究[J]. 体育成人教育学刊, 2016, 32(5): 18-21.
[5] 许臻晔, 廖育鲲, 黄文婵, 等. 马拉松相关心脏骤停与气象因素的相关性分析[J]. 中国运动医学杂志, 2018, 37(5): 427-431.
[6] 杨盼, 江姝, 葛志祥, 等. 心电图SV3+RV5/V6标准在诊断马拉松跑者左心室肥厚中的价值[J]. 临床心血管病杂志, 2024, 40(1): 57-63. doi: 10.13201/j.issn.1001-1439.2024.01.011
[7] Claessen G, La Gerche A. Exercise-induced cardiac fatigue: the need for speed[J]. J Physiol, 2016, 594(11): 2781-2782. doi: 10.1113/JP272168
[8] 张贺彬, 郑哲岚, 高枫, 等. 二维斑点追踪技术对业余马拉松运动员左心室收缩功能的研究[J]. 中华超声影像学杂志, 2021, 30(1): 31-36.
[9] Minciunǎ I, Hilda Orǎşan O, Minciunǎ I, et al. Assessment of subclinical diabetic cardiomyopathy by speckle-tracking imaging[J]. Eur J Clin Invest, 2021, 51(4): e13475.
[10] 中国医师协会超声医师分会心脏超声专业委员会. 二维斑点追踪超声心动图心肌纵向应变规范化检查中国专家共识(2023版)[J]. 中华超声影像学杂志, 2023, 32(4): 277-287.
[11] 凌小莉, 刘承宏, 赵凯跃, 等. 心脏MR特征追踪技术对业余马拉松运动员双心室心肌应变的研究[J]. 中华放射学杂志, 2023, 57(12): 1278-1283.
[12] 中华医学会超声医学分会超声心动图学组. 中国成年人超声心动图检查测量指南[J]. 中华超声影像学杂志, 2016, 25(8): 645-666.
[13] 《心电图测量技术指南》编写专家组. 心电图测量技术指南[J]. 实用心电学杂志, 2019, 28(2): 77-86.
[14] Kim Y, Park K. Effects of Super-ultramarathon Running on Cardiac Structure and Function in Middle-aged Men[J]. J Cardiovasc Imaging, 2020, 28(3): 202-210.
[15] 温燕, 赵莉莉, 陈菁, 等. 马拉松赛对运动员心脏电生理相关指标的影响[J]. 中华急诊医学杂志, 2018, 27(8): 854-858.
[16] Trivax J, McCullough P. Phidippides cardiomyopathy: a review and case illustration[J]. Clin Cardiol, 2012, 35(2): 69-73.
[17] Prior D, La Gerche A. The athlete's heart[J]. Heart, 2012, 98(12): 947-955.
[18] Herm J, Töpper A, Wutzler A, et al. Frequency of exercise-induced ST-T-segment deviations and cardiac arrhythmias in recreational endurance athletes during a marathon race: results of the prospective observational Berlin Beat of Running study[J]. BMJ Open, 2017, 7(8): e015798.
[19] Lasocka Z, Dąbrowska-Kugacka A, Kaleta A, et al. Electrocardiographic Changes in Male and Female Amateur Marathon Runners: A Comparison Study[J]. Int J Sports Med, 2021, 42(10): 936-944.
[20] Baggish A, Battle R, Beaver T, et al. Recommendations on the Use of Multimodality Cardiovascular Imaging in Young Adult Competitive Athletes: A Report from the American Society of Echocardiography in Collaboration with the Society of Cardiovascular Computed Tomography and the Society for Cardiovascular Magnetic Resonance[J]. J Am Soc Echocardiogr, 2020, 33(5): 523-549.
[21] Knechtle B, Nikolaidis P. Physiology and Pathophysiology in Ultra-Marathon Running[J]. Front Physiol, 2018, 9: 634.
[22] Lewicka-Potocka Z, Dąbrowska-Kugacka A, Lewicka E, et al. The "athlete's heart" features in amateur male marathon runners[J]. Cardiol J, 2021, 28(5): 707-715.
[23] 张贺彬, 高枫, 杨寸芯, 等. 三维斑点追踪技术评价业余马拉松运动员左心室结构与收缩功能的早期改变[J]. 中华超声影像学杂志, 2022, 31(8): 705-711.
[24] 李真, 滑少华, 李莉锦, 等. 超声分层应变技术对青年男性力量型运动员左心室收缩功能的研究[J]. 中华超声影像学杂志, 2020, 29(5): 394-398.
[25] Slivnick J, Lampert BC. Hypertension and Heart Failure[J]. Heart Fail Clin, 2019, 15(4): 531-541.
[26] 李苏雷, 智光, 穆洋. 心电图与超声心动图诊断原发性高血压导致左室肥厚的对比研究[J]. 中华保健医学杂志, 2017, 19(2): 118-121.
[27] Bogdanović J, Ašanin M, Krljanac G, et al. Impact of acute hyperglycemia on layer-specific left ventricular strain in asymptomatic diabetic patients: an analysis based on two-dimensional speckle tracking echocardiography[J]. Cardiovasc Diabetol, 2019, 18(1): 68.
[28] Tops LF, Delgado V, Marsan NA, et al. Myocardial strain to detect subtle left ventricular systolic dysfunction[J]. Eur J Heart Fail, 2016, 19(3): 307-313.
[29] Gabrielli L, Sitges M, Chiong M, et al. Potential adverse cardiac remodelling in highly trained athletes: still unknown clinical significance[J]. Eur J Sport Sci, 2018, 18(9): 1288-1297.
[30] Tarascio M, Leo L, Klersy C, et al. Speckle-Tracking Layer-Specific Analysis of Myocardial Deformation and Evaluation of Scar Transmurality in Chronic Ischemic Heart Disease[J]. J Am Soc Echocardiogr, 2017, 30(7): 667-675.
[31] 滑少华, 李莉锦, 孙希瑶, 等. 三维斑点追踪技术对青年男性力量型运动员左心室收缩功能的研究[J]. 中华超声影像学杂志, 2017, 26(8): 657-660.
[32] 吕诗佳, 袁建军, 朱好辉, 等. 应用分层应变及跨壁阶差评价高血压患者左心室收缩功能改变[J]. 中华超声影像学杂志, 2019, 28(5): 392-396.
-

计量
- 文章访问数: 315
- 施引文献: 0



 下载:
下载: