Interpretation of the Guidelines for standardized screening of Fabry disease by echocardiography in China(2024 edition)
-
摘要: 2024年中国超声心动图学会联合中华医学会超声医学分会和山东省医学会超声医学分会,结合国内外相关文献和指南,根据法布雷病临床表现、病理生理学改变以及超声心动图特征,撰写了《中国法布雷病超声心动图规范化筛查指南(2024版)》。该指南为法布雷病心脏受累患者早期筛查提供了超声心动图特征和鉴别诊断等方面的具体建议,旨在进一步推动法布雷病的超声心动图规范化检查和早期识别。为更好地指导临床应用超声心动图规范化筛查法布雷病心脏受累患者,本文就该指南的基本内容进行解读,并建立了疑似法布雷病心脏受累患者的超声心动图结构化报告。Abstract: In 2024, the Chinese Society of Echocardiography, together with the Chinese Society of Ultrasound in Medicine and the Ultrasonic Medicine Branch of Shandong Medical Association, combined relevant literature and guidelines from both China and abroad to write the Guidelines for standardized screening of Fabry disease by echocardiography in China(2024 edition) , based on the clinical manifestations, pathophysiological changes, and echocardiographic characteristics of Fabry disease. This guideline provides specific recommendations on echocardiographic features and differential diagnosis for the early screening of patients with heart involvement in Fabry disease, aiming to further promote the standardization of echocardiography and early identification of Fabry disease. In order to better guide the clinical application of echocardiography in the standardized screening of patients with suspected cardiac involvement in Fabry disease, this article interprets the basic content of the guidelines and establishes a structured echocardiographic report for patients with suspected Fabry disease cardiac involvement.
-
Key words:
- Fabry disease /
- echocardiography /
- screening /
- guidelines /
- interpretation
-

-
表 1 法布雷病心脏受累超声心动图筛查要点与推荐建议(表格来源[5])
Table 1. Key points and recommendations for echocardiographic screening of cardiac involvement in Fabry disease(Table source[5])
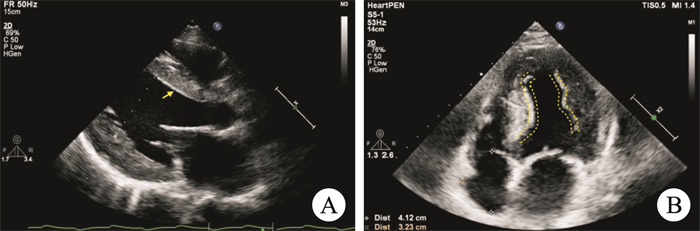
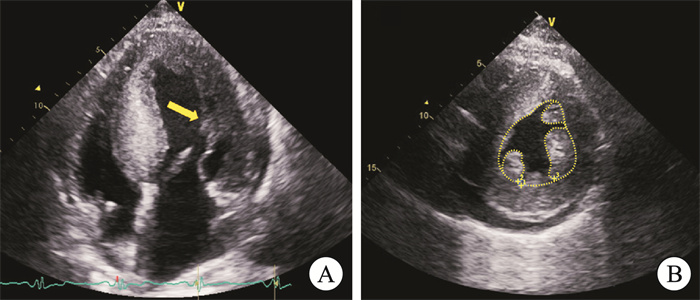
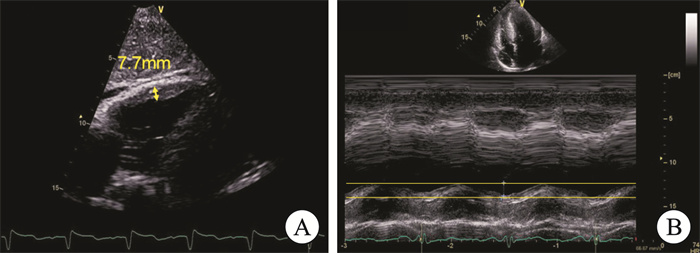
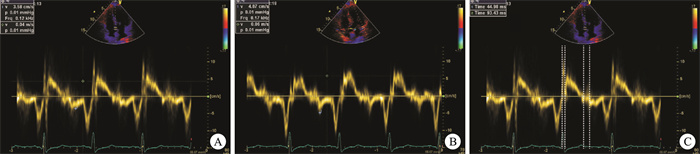
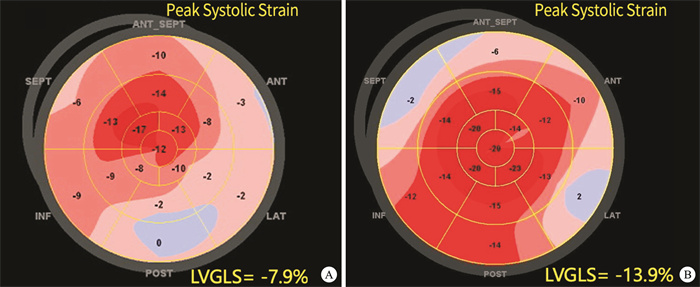
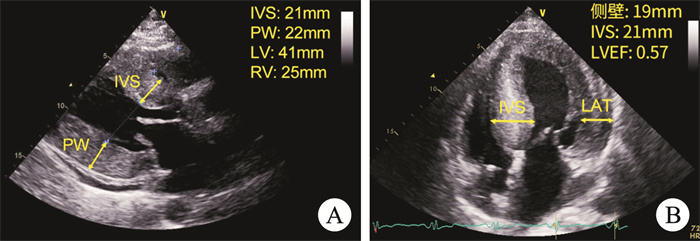
特征 推荐意见 推荐类别 证据水平 对于疑似或诊断为法布雷病的患者,推荐采用超声心动图进行心脏受累情况的初始评估。 Ⅰ A 左心室向心性肥厚 左心室肥厚是法布雷病心脏受累最常见和主要的超声心动图特征,主要表现为向心性肥厚。 Ⅰ A “双边征” “双边征”是法布雷病心脏受累的一个标志性特点,在左心室肥厚患者中更常见,以室间隔最为明显。因其特异度高而灵敏度较低,故仅依靠“双边征”诊断法布雷病受到限制。 Ⅱa B 乳头肌肥大 乳头肌不成比例肥大,是法布雷病心脏受累较为特异的表现。联合乳头肌面积>3.6 cm2和乳头肌与左心室横截面积比值>0.18诊断法布雷病具有较好的灵敏度和特异度。 Ⅰ B 右心室肥厚 右心室肥厚较常见,通常与左心室肥厚并存,很少单独发生,其程度与并存的左心室肥厚程度相关。右心室肥厚对收缩功能没有显著影响,右心室收缩功能障碍非常罕见。 Ⅱa B 左心舒张功能障碍 左心功能障碍主要表现为舒张功能障碍,多为中度,左心室肥厚患者中更常见;LVEF多可保留至疾病晚期。 Ⅱa C 心肌收缩和舒张速度降低 组织多普勒特征表现为心肌收缩和舒张速度降低,联合IVCT≤105 ms和e' < 10 cm/s有助于法布雷病心肌肥厚与其他原因所致的心肌肥厚的鉴别诊断。 Ⅱa C 纵向应变降低 斑点追踪显像特征性表现为纵向应变降低,尤以左心室下外侧壁基底段降低最为明显,左室下外侧壁基底段纵向应变降低至≥-13%。 Ⅰ B 右心室斑点追踪显像应变降低。 Ⅱb B LVEF:左心室射血分数;IVCT:等容收缩时间;e':二尖瓣环间隔处心肌舒张早期运动速度。 表 2 疑似法布雷病心脏受累患者超声心动图结构化报告
Table 2. Structured echocardiographic report for patients with suspected cardiac involvement in Fabry disease
超声心动图检查报告 基本信息 姓名: 性别: 年龄: 门诊号: 临床诊断 此处描述临床诊断结果 心脏测值 左心房前后径(LA-APD) ____mm 左心房容积指数(LAVI) ____mL/m2 左心室前后径(LV-APD) ____mm 室间隔厚度(IVST) ____mm 左心室后壁厚度(LVPWT) ____mm 左心室最大室壁厚度 ____mm 左心室最大室壁位置(节段) ____节段 左心室流出道内径(LVOTD) ____mm 左心室舒张末期容积(LVEDV) ____mL 左心室收缩末期容积(LVESV) ____mL 左心室纵向应变(LV GLS) ____% 左心室射血分数(LVEF) ____% 肺动脉主干内径(MPAD) ____mm 升主动脉内径(AOD) ____mm 右心房内径(RAD) ____mm 右心室前后径(RVAPD) ____mm 右心室游离壁厚度(RVFWT) ____mm 右室分数面积变化(RVFAC) ____% 二尖瓣:E峰 ____cm/s 二尖瓣:A峰 ____cm/s 二尖瓣:E/A ____ 二尖瓣:e' ____cm/s 等容收缩时间(IVCT) ____ms 三尖瓣环收缩期运动幅度(TAPSE) ____mm 二尖瓣反流速度(MR) ____cm/s 三尖瓣反流速度(TR) ____cm/s 超声描述 二维及M型超声 各房室内径大小:□正常□异常
主动脉、肺动脉内径:□正常□异常各心室壁厚度:□正常□异常
各瓣膜形态:□未见明显异常□异常疑似法布雷病心脏受累相关特征 是否存在左心室肥厚:□是□否
是则报告左心室肥厚类型:□左心室向心性肥厚
□左心室非对称性肥厚□左心室心尖肥厚是否存在右心室肥厚:□是□否
是否存在有乳头肌肥大:□是□否
是否存在“双边征”:□是□否彩色及组织多普勒 各瓣膜功能:□正常□异常;是否存在返流:□是□否 心肌收缩和舒张速度降低:□是□否 斑点追踪超声心动图 左心室纵向应变降低:□是□否
是则报告左心室纵向应变显著降低部位:□基底段下外侧□基底段近前壁、间隔壁□基底段和中间段而心尖段保留□整体□基底段间隔壁和大部分基底区域超声提示 1:当临床提示为肥厚性心肌病,而超声心动图发现左心室肥厚类型为向心性、对称性肥厚时,应在报告中提示“疑似法布雷病”。2:当超声心动图发现左心室肥厚,合并以下其中一项时,包括乳头肌肥大、右心室肥厚、“双边征”、或斑点追踪超声显示左心室下外侧壁基底段纵向应变降低,应在报告中提示“疑似法布雷病”。 诊断建议 根据超声心动图报告提示怀疑法布雷病,请结合临床进一步明确诊断。 表 3 法布雷病与其他左心室肥厚相关疾病的鉴别诊断
Table 3. Differential diagnosis of Fabry disease and other diseases associated with left ventricular hypertrophy
影像学技术 特征表现 法布雷病心肌病* 肥厚型心肌病 淀粉样变性 主动脉瓣狭窄 高血压性心脏病 常规超声心动图 向心性(对称性)左心室肥厚[26] √ × √ √ √ 双边征[31] √ × × × × 乳头肌肥大[26, 32] √ 可能有 × 可能有 可能有 右心室肥厚[33-34] √ 可能有 可能有 × × 室间隔或左室后壁厚度[5] ≥15 mm多见 ≥15 mm >15 mm多见 一般≤15 mm 一般≤15 mm 斑点追踪超声心动图 左心室纵向应变减低[26, 29] 基底段下外侧区纵向应变减低 基底段近前壁、间隔壁纵向应变减低 基底段和中间段纵向应变减低,而心尖段保留 基底段纵向应变减低 肥厚区纵向应变减低(通常是室间隔基底段) 心电图 左心室高电压[27] √ √ × √ √ PR间期缩短[27, 30] √ × × × × 心脏磁共振 初始T1值[29] 减低 升高 升高 升高 正常或轻度升高 钆延迟强化[29] 左心室前外侧和下外侧壁基底段和中段的肌层内LGE 室壁明显肥厚处以及室间隔与右心室交界处、肌间LGE 弥漫性,心内膜下或肌间LGE 非特异性斑片模式、肌间LGE 非特异性斑片模式、肌间LGE 注:LGE:钆延迟强化;*代表不同的法布雷心肌病患者可能会存在表中列举的其中一种征象,也可能同时存在一种以上征象。 -
[1] Pieroni M, Namdar M, Olivotto I, et al. Anderson-fabry disease management: role of the cardiologist [J]. Eur Heart J, 2024, 45(16): 1395-1409. doi: 10.1093/eurheartj/ehae148
[2] Beck M, Ramaswami U, Hernberg-Ståhl E, et al. Twenty years of the fabry outcome survey(FOS): insights, achievements, and lessons learned from a global patient registry [J]. Orphanet J Rare Dis, 2022, 17(1): 238. doi: 10.1186/s13023-022-02392-9
[3] Pieroni M, Moon JC, Arbustini E, et al. Cardiac involvement in fabry disease: JACC review topic of the week [J]. J Am Coll Cardiol, 2021, 77(7): 922-936. doi: 10.1016/j.jacc.2020.12.024
[4] Perry R, Shah R, Saiedi M, et al. The role of cardiac imaging in the diagnosis and management of Anderson-fabry disease [J]. JACC Cardiovasc Imaging, 2019, 12(7 Pt 1): 1230-1242.
[5] 中国超声心动图学会, 中华医学会超声医学分会, 山东省医学会超声医学分会. 中国法布雷病超声心动图规范化筛查指南(2024版) [J]. 中华超声影像学杂志, 2024, 33(4): 277-287.
[6] Hongo K. Cardiac involvement in Fabry disease-A non-invasive assessment and the role of specific therapies [J]. Mol Genet Metab, 2022, 137(1-2): 179-186. doi: 10.1016/j.ymgme.2022.08.006
[7] Wu JC, Ho CY, Skali H, et al. Cardiovascular manifestations of fabry disease: relationships between left ventricular hypertrophy, disease severity, and alpha-galactosidase A activity [J]. Eur Heart J, 2010, 31(9): 1088-1097. doi: 10.1093/eurheartj/ehp588
[8] Shanks M, Thompson RB, Paterson ID, et al. Systolic and diastolic function assessment in fabry disease patients using speckle-tracking imaging and comparison with conventional echocardiographic measurements [J]. J Am Soc Echocardiogr, 2013, 26(12): 1407-1414. doi: 10.1016/j.echo.2013.09.005
[9] 胡艺川, 尹立雪, 王志刚. 超声心动图在法布里病早期诊断中的应用[J]. 中华超声影像学杂志, 2013, 22(7): 626-629.
[10] Koskenvuo JW, Engblom E, Kantola IM, et al. Echocardiography in Fabry disease: diagnostic value of endocardial border binary appearance [J]. Clin Physiol Funct Imaging, 2009, 29(3): 177-180. doi: 10.1111/j.1475-097X.2008.00851.x
[11] Kounas S, Demetrescu C, Pantazis AA, et al. The binary endocardial appearance is a poor discriminator of Anderson-Fabry disease from familial hypertrophic cardiomyopathy [J]. J Am Coll Cardiol, 2008, 51(21): 2058-2061. doi: 10.1016/j.jacc.2008.02.046
[12] Mundigler G, Gaggl M, Heinze G, et al. The endocardial binary appearance('binary sign')is an unreliable marker for echocardiographic detection of Fabry disease in patients with left ventricular hypertrophy [J]. Eur J Echocardiogr, 2011, 12(10): 744-749. doi: 10.1093/ejechocard/jer112
[13] Yeung DF, Sirrs S, Tsang MYC, et al. Echocardiographic assessment of patients with fabry disease [J]. J Am Soc Echocardiogr, 2018, 31(6): 639-649. e2.
[14] Cianciulli TF, Saccheri MC, Llobera MN, et al. Prevalence of papillary muscle hypertrophy in fabry disease [J]. BMC Cardiovasc Disord, 2023, 23(1): 424. doi: 10.1186/s12872-023-03463-w
[15] Graziani F, Lillo R, Panaioli E, et al. Prognostic significance of right ventricular hypertrophy and systolic function in Anderson-Fabry disease [J]. ESC Heart Fail, 2020, 7(4): 1605-1614. doi: 10.1002/ehf2.12712
[16] Niemann M, Breunig F, Beer M, et al. The right ventricle in fabry disease: natural history and impact of enzyme replacement therapy [J]. Heart, 2010, 96(23): 1915-1919.
[17] Morris DA, Blaschke D, Canaan-Kühl S, et al. Global cardiac alterations detected by speckle-tracking echocardiography in Fabry disease: left ventricular, right ventricular, and left atrial dysfunction are common and linked to worse symptomatic status [J]. Int J Cardiovasc Imaging, 2015, 31(2): 301-313.
[18] Militaru S, Jurcu R, Adam R, et al. Echocardiographic features of Fabry cardiomyopathy-Comparison with hypertrophy-matched sarcomeric hypertrophic cardiomyopathy [J]. Echocardiography, 2019, 36(11): 2041-2049.
[19] Steudel T, Barzen G, Frumkin D, et al. Diagnostic value of left ventricular layer strain and specific regional strain patterns in cardiac amyloidosis and Fabry disease [J]. Eur Heart J Open, 2024, 4(3): oeae041.
[20] Mattig I, Steudel T, Barzen G, et al. Diagnostic value of papillary muscle hypertrophy and mitral valve thickness to discriminate cardiac amyloidosis and Fabry disease [J]. Int J Cardiol, 2024, 397: 131629.
[21] 薛超, 何怡华, 韩建成, 等. 主动脉瓣下隔膜的超声心动图表现及临床特点分析[J]. 医学影像学杂志, 2019, 29(3): 378-380.
[22] 卓宇, 龙湘党, 敖琨, 等. 分层应变技术评估主动脉瓣狭窄患者左室心肌收缩功能的价值[J]. 中国医师杂志, 2022, 24(11): 1665-1669.
[23] Ferkh A, Tjahjadi C, Stefani L, et al. Cardiac"hypertrophy"phenotyping: differentiating aetiologies with increased left ventricular wall thickness on echocardiography [J]. Front Cardiovasc Med, 2023, 10: 1183485.
[24] Tanaka H. Efficacy of echocardiography for differential diagnosis of left ventricular hypertrophy: special focus on speckle-tracking longitudinal strain [J]. J Echocardiogr, 2021, 19(2): 71-79.
[25] Iorio A, Lucà F, Pozzi A, et al. Anderson-fabry disease: red flags for early diagnosis of cardiac involvement [J]. Diagnostics(Basel), 2024, 14(2): 208.
[26] Fuertes Kenneally L, García-Álvarez MI, Rey EF, et al. Fabry disease cardiomyopathy: a review of the role of cardiac imaging from diagnosis to treatment [J]. Rev Cardiovasc Med, 2022, 23(6): 192.
[27] 董吁钢, 杨杰孚. 左心室肥厚诊断和治疗临床路径中国专家共识2023 [J]. 中国循环杂志, 2024, 39(1): 17-28.
[28] Tower-Rader A, Jaber WA. Multimodality imaging assessment of fabry disease [J]. Circ Cardiovasc Imaging, 2019, 12(11): e009013.
[29] 中华医学会心血管病学分会, 中华心血管病杂志编辑委员会. 成人法布雷病心肌病诊断与治疗中国专家共识[J]. 中华心血管病杂志, 2024, 52(2): 128-136.
[30] Linhart A, Germain DP, Olivotto I, et al. An expert consensus document on the management of cardiovascular manifestations of Fabry disease [J]. Eur J Heart Fail, 2020, 22(7): 1076-1096.
[31] Pieroni M, Chimenti C, De Cobelli F, et al. Fabry's disease cardiomyopathy: echocardiographic detection of endomyocardial glycosphingolipid compartmentalization [J]. J Am Coll Cardiol, 2006, 47(8): 1663-1671.
[32] Niemann M, Liu D, Hu K, et al. Prominent papillary muscles in fabry disease: a diagnostic marker? [J]. Ultrasound Med Biol, 2011, 37(1): 37-43.
[33] 刘丽文, 王静. 肥厚型心肌病超声心动图检查规范专家共识[J]. 中华医学超声杂志(电子版), 2020, 17(5): 394-408.
[34] 中国医师协会超声医师分会心脏超声专业委员会. 心脏淀粉样变超声心动图规范化检查中国专家共识(2023版) [J]. 中华超声影像学杂志, 2023, 32(12): 1021-1029.
-

计量
- 文章访问数: 227
- 施引文献: 0



 下载:
下载: