Correlation between visceral adiposity index and early morning hypertension in patients with hypertension
-
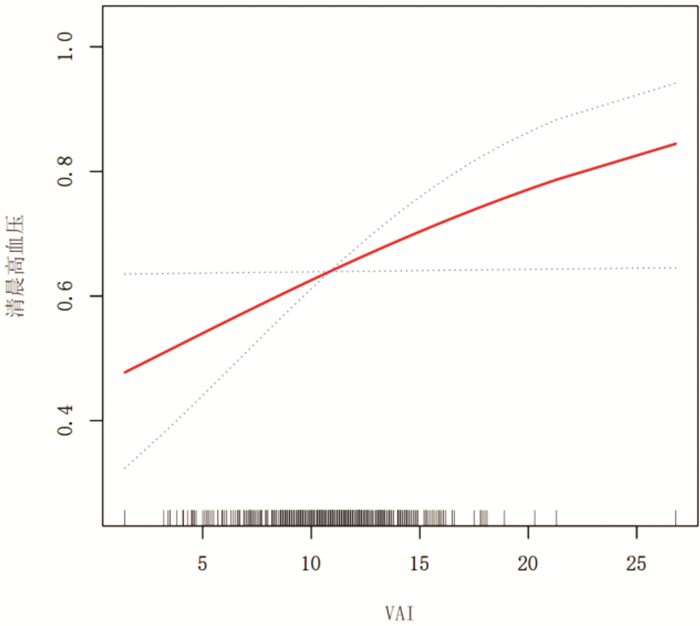
摘要: 目的 探讨内脏脂肪指数(VAI)与晨峰高血压发生之间的关系。方法 选取2018年10月—2021年11月在承德医学院附属医院老年病科及全科医疗科住院的高血压病患者539例。行24 h动态血压监测,依据晨间血压水平分为晨峰高血压组342例和非晨峰高血压组197例,应用生物电阻抗法(BIA)测量内脏脂肪,同时收集患者的一般资料,进一步分析VAI与晨峰高血压之间的相关性。结果 ① 晨峰高血压组VAI高于非晨峰高血压组,差异有统计学意义[(11.10±3.07) vs (10.53±2.97),P < 0.05];②晨峰高血压组24 h平均收缩压及舒张压、日平均收缩压及舒张压、夜平均收缩压及舒张压均高于非晨峰高血压组,差异有统计学意义(P < 0.05),而两组24 h收缩压及舒张压变异系数、日收缩压及舒张压变异系数、夜收缩压及舒张压变异系数比较,差异无统计学意义;③多因素logistic回归分析评估VAI是晨峰高血压的独立危险因素(OR=1.07,95%CI 1.00~1.15);④在平滑曲线拟合中显示,VAI与晨峰高血压呈线性正相关。结论 在原发性高血压人群中,晨峰高血压发病率较高,且VAI是晨峰高血压发生的危险因素,VAI与晨峰高血压呈线性正相关。Abstract: Objective To investigate the correlation between visceral adiposity index(VAI) and early morning hypertension.Methods A total of 539 patients with hypertension were selected. A 24-hour ambulatory blood pressure monitoring was performed, and the patients were divided into early morning hypertension group and non-early morning hypertension group according to the early morning blood pressure level, and the visceral adiposity index was measured using BIA, and the general data of the patients were recorded, and further analyzed correlation between VAI and early morning hypertension.Results The visceral fat index in early morning hypertension group was significantly higher than that in non-morning hypertension group(P < 0.05). Multivariate logistic regression analysis showed that VAI was an independent risk factor for hypertension in the early morning(OR=1.07, 95%CI1.00~1.15). In smooth curve fitting, VAI was linearly positively correlated with morning hypertension.Conclusion In the patients with essential hypertension, the incidence of hypertension in the early morning increase, and VAI is a risk factor for the occurrence of hypertension in the morning. There is a linear positive correlation between VAI and hypertension in the morning.
-
Key words:
- hypertension /
- early morning hypertension /
- visceral adiposity index
-

-
表 1 一般资料
Table 1. General data
例(%), X±S 项目 所有人群 非晨峰高血压组 晨峰高血压组 P 例数/例 539 197 342 年龄/岁 65.84±11.63 65.58±11.92 66.00±11.48 0.688 男性 284(52.69) 102(51.78) 182(53.22) 0.747 体重/kg 71.57±12.88 70.47±12.92 72.21±12.83 0.084 身高/cm 165.44±7.54 165.47±7.48 165.42±7.58 0.869 BMI/(kg·m-2) 26.08±3.88 25.67±3.97 26.31±3.82 0.020 吸烟 175(32.53) 61(31.12) 114(33.33) 0.598 饮酒 163(30.30) 57(29.08) 106(30.99) 0.642 糖尿病 178(33.15) 63(31.98) 115(33.82) 0.662 高血压用药 364(67.53) 132(67.01) 232(67.84) 0.843 空腹血糖/(mmol·L-1) 6.91±3.06 6.61±2.68 7.09±3.25 0.441 谷丙转氨酶/(U·L-1) 24.33±18.40 24.04±17.43 24.49±18.95 0.804 谷草转氨酶/(U·L-1) 27.07±30.68 24.76±10.59 28.37±37.49 0.923 甘油三酯/(mmol·L-1) 2.05±1.91 2.07±2.50 2.03±1.48 0.518 高密度脂蛋白/(mmol·L-1) 1.02±0.29 1.01±0.30 1.02±0.29 0.441 低密度脂蛋白/(mmol·L-1) 2.40±1.02 2.42±1.16 2.39±0.92 0.207 胆固醇/(mmol·L-1) 4.25±1.09 4.26±1.02 4.25±1.13 0.783 尿酸/(μmol·L-1) 325.88±88.32 325.96±86.66 325.84±89.37 0.932 VAI 10.89±3.04 10.53±2.97 11.10±3.07 0.043 入院时收缩压/mmHg 146.47±19.25 140.15±14.90 150.12±20.51 < 0.001 入院时舒张压/mmHg 86.42±12.11 83.58±10.07 88.06±12.88 < 0.001 24 h平均收缩压/mmHg 136.63±16.80 123.39±11.00 144.25±14.710 < 0.001 24 h平均舒张压/mmHg 77.16±9.85 71.19±7.56 80.60±9.37 < 0.001 收缩压变异系数 12.91±4.11 13.31±4.48 12.67±3.87 0.232 舒张压变异系数 14.95±5.72 14.76±5.87 15.06±5.64 0.290 日平均收缩压/mmHg 137.63±16.92 124.63±11.54 145.31±14.78 < 0.001 日平均舒张压/mmHg 78.11±10.37 72.36±8.70 81.51±9.77 < 0.001 日收缩压变异系数 12.48±4.46 12.81±4.91 12.29±4.17 0.489 日舒张压变异系数 14.49±5.87 14.43±6.52 14.53±5.46 0.372 夜平均收缩压/mmHg 132.81±19.81 120.41±14.02 140.22±19.06 < 0.001 夜平均舒张压/mmHg 73.84±11.46 68.29±10.31 77.15±10.83 < 0.001 夜收缩压变异系数 10.95±4.64 11.29±4.55 10.74±4.69 0.136 夜舒张压变异系数 12.78±5.69 12.78±5.75 12.78±5.66 0.945 表 2 不同模型下VAI与晨峰高血压的关系
Table 2. Correlation Between VAI and early morning hypertension
变量 模型1 模型2 模型3 OR(95%CI) P OR(95%CI) P OR(95%CI) P VAI 1.06(1.00~1.13) 0.0379 1.07(1.01~1.14) 0.0283 1.07(1.00~1.15) 0.0445 VAI分组 Q1 Reference Reference Reference Q2 1.06(0.65~1.74) 0.8028 1.11(0.67~1.82) 0.6871 1.29(0.75~2.24) 0.3576 Q3 1.13(0.69~1.84) 0.6357 1.18(0.72~1.93) 0.5233 1.32(0.75~2.30) 0.3341 Q4 1.92(1.15~3.21) 0.0120 2.01(1.20~3.37) 0.0084 2.10(1.15~3.83) 0.0151 P趋势性检验 P=0.0151 P=0.0105 P=0.0193 年龄分组 < 60岁 1.02(0.92~1.14) 0.6950 1.04(0.92~1.17) 0.5422 1.04(0.90~1.19) 0.6088 60~79岁 1.08(1.00~1.17) 0.0469 1.11(1.02~1.20) 0.0163 1.12(1.02~1.23) 0.0233 ≥80岁 1.07(0.92~1.24) 0.3854 1.05(0.89~1.23) 0.5583 1.10(0.83~1.46) 0.5077 性别 女性 1.09(0.99~1.19) 0.0722 1.09(1.00~1.20) 0.0572 1.10(0.99~1.22) 0.0782 男性 1.05(0.97~1.14) 0.2156 1.04(0.96~1.12) 0.3757 1.03(0.93~1.13) 0.5755 -
[1] Blüher M. Obesity: global epidemiology and pathogenesis[J]. Nat Rev Endocrinol, 2019, 15(5): 288-298. doi: 10.1038/s41574-019-0176-8
[2] Umemura S, Arima H, Arima S, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension(JSH 2019)[J]. Hypertensi Res, 2019, 42(9): 1235-1481. doi: 10.1038/s41440-019-0284-9
[3] Wang JG, Kario K, Chen CH, et al. Management of morning hypertension: a consensus statement of an Asian expert panel[J]. J Clin Hypertens(Greenwich), 2018, 20(1): 39-44. doi: 10.1111/jch.13140
[4] Fan Y, He D, Liu S, et al. Association between visceral adipose index and risk of hypertension in a middle-aged and elderly Chinese population[J]. Nutr Metab Cardiovasc Dis, 2021, 31(8): 2358-2365. doi: 10.1016/j.numecd.2021.04.024
[5] Zhang Z, Shi D, Zhang Q, et al. Visceral adiposity index(VAI), a powerful predictor of incident hypertension in prehypertensives[J]. Intern Emerg Med, 2018, 13(4): 509-516. doi: 10.1007/s11739-018-1836-8
[6] Lee Y, Lee Y, Chuang P, et al. The utility of visceral fat level measured by bioelectrical impedance analysis in predicting metabolic syndrome[J]. Obes Res Clin Pract, 2020, 14(6): 519-523. doi: 10.1016/j.orcp.2020.09.008
[7] 刘惠娟, 唐腾腾, 徐新娟, 等. 原发性高血压患者24 h尿钠钾比值与中心动脉压相关指标之间的关系[J]. 临床心血管病杂志, 2021, 37(3): 234-239. https://www.cnki.com.cn/Article/CJFDTOTAL-LCXB202103010.htm
[8] Xin M, Zhang S, Zhao L, et al. Circadian and seasonal variation in onset of acute myocardial infarction[J]. Medicine(Baltimore), 2022, 101(28): e29839.
[9] Smolensky MH, Hermida RC, Portaluppi F. Circadian mechanisms of 24-hour blood pressure regulation and patterning[J]. Sleep Med Rev, 2017, 33: 4-16. doi: 10.1016/j.smrv.2016.02.003
[10] Oh J, Lee CJ, Kim IC, et al. Association of morning hypertension subtype with vascular target organ damage and central hemodynamics[J]. J Am Heart Assoc, 2017, 6(2): 110.
[11] Geng X, Liu X, Li F, et al. Blood pressure variability at different time periods within first 24 hours after admission and outcomes of acute ischemic stroke[J]. J Clin Hypertens(Greenwich), 2020, 22(2): 194-204. doi: 10.1111/jch.13785
[12] Wanthong S, Kabutoya T, Hoshide S, et al. Early morning-Best time window of hourly 24-hour ambulatory blood pressure in relation to hypertensive organ damage: The Japan Morning Surge-Home Blood Pressure study[J]. J Clin Hypertens(Greenwich), 2019, 21(5): 579-586. doi: 10.1111/jch.13498
[13] 陈茂鹤, 林琳, 陈睿, 等. 晨峰高血压与靶器官损害及10年动脉粥样硬化性心血管病发病风险的关系[J]. 中华高血压杂志, 2022, 30(5): 483-487. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGGZ202205015.htm
[14] Wu Q, Qu J, Yin Y, et al. Morning hypertension is a risk factor of macrovascular events following cerebral infarction[J]. Medicine, 2018, 97(34): e12013. doi: 10.1097/MD.0000000000012013
[15] Kim HJ, Shin JH, Lee Y, et al. Clinical features and predictors of masked uncontrolled hypertension from the Korean Ambulatory Blood Pressure Monitoring Registry[J]. Korean J Intern Med, 2021, 36(5): 1102-1114. doi: 10.3904/kjim.2020.650
[16] Satoh M, Metoki H, Asayama K, et al. Prediction models for the 5-and 10-year incidence of home morning hypertension: The Ohasama Study[J]. Am J Hypertens, 2022, 35(4): 328-336. doi: 10.1093/ajh/hpab177
[17] Shimizu M, Ishikawa J, Eguchi K, et al. Association of an abnormal blood glucose level and morning blood pressure surge in elderly subjects with hypertension[J]. Am J Hypertens, 2009, 22(6): 611-616. doi: 10.1038/ajh.2009.61
[18] Huang JF, Li Y, Shin J, et al. Characteristics and control of the 24-hour ambulatory blood pressure in patients with metabolic syndrome[J]. J Clin Hypertens(Greenwich), 2021, 23(3): 450-456. doi: 10.1111/jch.14229
[19] Zhang M, Zheng L, Li P, et al. 4-Year trajectory of visceral adiposity index in the development of type 2 diabetes: A Prospective Cohort Study[J]. Ann Nut Met, 2016, 69(2): 142-149. doi: 10.1159/000450657
[20] Kouli GM, Panagiotakos DB, Kyrou I, et al. Visceral adiposity index and 10-year cardiovascular disease incidence: The ATTICA study[J]. Nut Met Cardiovasc Dis, 2017, 27(10): 881-889. doi: 10.1016/j.numecd.2017.06.015
[21] 李中根, 李凌, 李黎, 等. 心外膜脂肪厚度与射血分数保留性心衰风险的相关性[J]. 临床心血管病杂志, 2022, 38(5): 393-399. doi: 10.13201/j.issn.1001-1439.2022.05.012 https://lcxxg.whuhzzs.com/article/doi/10.13201/j.issn.1001-1439.2022.05.012
[22] Li J, Zhu J, Tan Z, et al. Visceral adiposity index is associated with arterial stiffness in hypertensive adults with normal-weight: the china H-type hypertension registry study[J]. Nutr Metab(Lond), 2021, 18(1): 90.
[23] Choi HS, Cho YH, Lee SY, et al. Association between new anthropometric parameters and arterial stiffness based on brachial-ankle pulse wave velocity[J]. Diabetes Metab Syndr Obes, 2019, 12: 1727-1733. doi: 10.2147/DMSO.S211542
[24] Huang X, Jiang X, Wang L, et al. Visceral adipose accumulation increased the risk of hyperuricemia among middle-aged and elderly adults: a population-based study[J]. J Transl Med, 2019, 17(1): 341. doi: 10.1186/s12967-019-2074-1
[25] Kuwabara J, Kuwahara K, Kuwabara Y, et al. Cross-sectional study of the association between day-to-day home blood pressure variability and visceral fat area measured using the dual impedance method[J]. PLoS One, 2018, 13(11): e206945.
[26] Minh HV, Tien HA, Sinh CT, et al. Assessment of preferred methods to measure insulin resistance in Asian patients with hypertension[J]. J Clin Hypertens(Greenwich), 2021, 23(3): 529-537. doi: 10.1111/jch.14155
[27] Kumarasamy S, Gopalakrishnan K, Kim DH, et al. Dysglycemia induces abnormal circadian blood pressure variability[J]. Cardiovasc Diabetol, 2011, 10: 104. doi: 10.1186/1475-2840-10-104
[28] Kadi H, Avci E, Usta A, et al. Morning blood pressure surge and its relation to insulin resistance in patients of reproductive age with polycystic ovary syndrome[J]. Reprod Biol Endocrinol, 2018, 16(1): 75. doi: 10.1186/s12958-018-0394-2
[29] Hall JE, Mouton AJ, Da SA, et al. Obesity, kidney dysfunction, and inflammation: interactions in hypertension[J]. Cardiovasc Res, 2021, 117(8): 1859-1876. doi: 10.1093/cvr/cvaa336
[30] Grassi G, Biffi A, Seravalle G, et al. Sympathetic neural overdrive in the obese and overweight state[J]. Hypertension, 2019, 74(2): 349-358. doi: 10.1161/HYPERTENSIONAHA.119.12885
[31] Li P, Liu B, Wu X, et al. Perirenal adipose afferent nerves sustain pathological high blood pressure in rats[J]. Nat Commun, 2022, 13(1): 3130. doi: 10.1038/s41467-022-30868-6
[32] Smolensky MH, Hermida RC, Portaluppi F. Circadian mechanisms of 24-hour blood pressure regulation and patterning[J]. Sleep Med Rev, 2017, 33: 4-16. doi: 10.1016/j.smrv.2016.02.003
-




 下载:
下载: