Predictors and prognosis of heart failure with improved ejection fraction after chronic total occlusion percutaneous coronary intervention
-
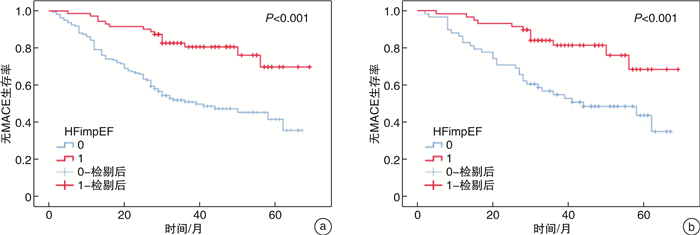
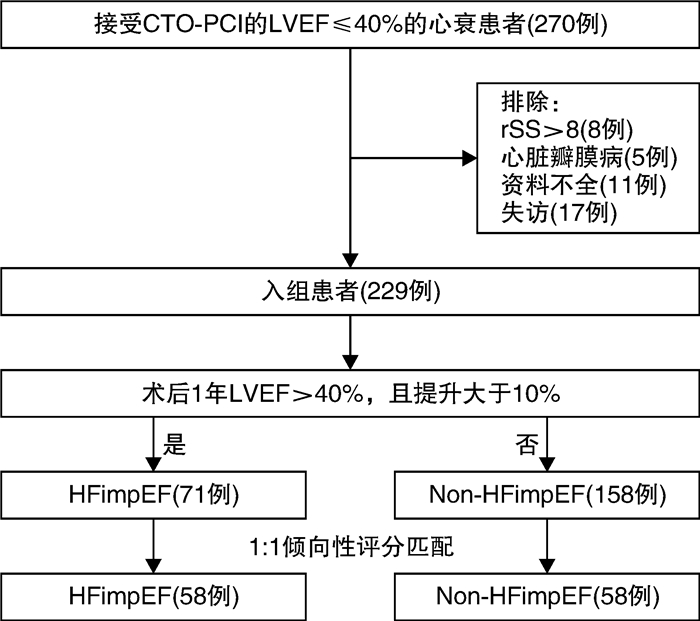
摘要: 目的 探究冠状动脉(冠脉)慢性完全闭塞病变经皮介入治疗(CTO-PCI)术后射血分数改善型心力衰竭(心衰)的影响因素及其长期预后。方法 回顾性入选CTO-PCI术前左室射血分数(LVEF)≤40%的心衰患者229例,根据术后1年LVEF的变化分为射血分数改善型心衰(HFimpEF)组(71例)和非射血分数改善型心衰(non-HFimpEF)组(158例)。采用logistic回归筛选CTO-PCI术后HFimpEF的影响因素;使用Cox回归探究主要不良心血管事件(MACE)的影响因素,并通过Kaplan-Meier生存分析比较两组的预后差异,同时基于倾向性评分匹配(PSM)进行敏感性分析。结果 Logistic回归结果示,年龄<60岁、左室舒张末期内径(LVEDD)<60 mm、J-CTO评分<3以及应用β受体阻滞剂和钠-葡萄糖共转运蛋白2抑制剂(SGLT2i)与CTO-PCI术后射血分数改善相关(P<0.05)。PSM前后的Cox回归结果均表明,HFimpEF是患者CTO-PCI术后发生MACE的独立保护因素(P<0.01)。PSM前后的Kaplan-Meier曲线显示HFimpEF组的无MACE生存率高于non-HFimpEF组(P<0.01)。结论 年龄<60岁、LVEDD<60 mm、J-CTO评分<3以及应用β受体阻滞剂和SGLT2i是CTO-PCI术后HFimpEF的独立影响因素,HFimpEF患者拥有更好的长期预后。
-
关键词:
- 射血分数改善型心力衰竭 /
- 慢性完全闭塞病变 /
- 经皮冠状动脉介入治疗 /
- 预后
Abstract: Objective To investigate the predictors and long-term prognosis of heart failure with improved ejection fraction(HFimpEF) after chronic total occlusion percutaneous coronary intervention(CTO-PCI).Methods A total of 229 heart failure patients with left ventricular ejection fraction(LVEF) ≤40% before CTO-PCI were retrospectively enrolled and divided into HFimpEF group(n=71) and non-HFimpEF group(n=158) according to the change in LVEF at 1 year after CTO-PCI. Binary logistic regression was used to screen the predictors of HFimpEF after CTO-PCI. Cox regression was used to explore the factors influencing major adverse cardiovascular events(MACE). Kaplan-Meier survival analysis was used to compare the prognostic differences between two groups, and sensitivity analysis was performed based on propensity score matching(PSM).Results Logistic regression analysis showed that age < 60 years, left ventricular end-diastolic diameter(LVEDD) < 60 mm, J-CTO score < 3, and the use of β-blockers and sodium-glucose cotransporter 2 inhibitors(SGLT2i) were associated with improved ejection fraction after CTO-PCI(P < 0.05). Cox regression analysis before and after PSM showed that HFimpEF was an independent protective factor for MACE after CTO-PCI(P < 0.01). Kaplan-Meier survival analysis showed higher MACE-free survival in the HFimpEF group than in the non-HFimpEF group(P < 0.01).Conclusion Age < 60 years, LVEDD < 60 mm, J-CTO score < 3, and the use of β-blockers and SGLT2i were predictors of HFimpEF after CTO-PCI, and this patient population had a better long-term prognosis. -

-
表 1 PSM前后基线人口统计学及临床特征对比
Table 1. Comparison of demographic and clinical characteristics before and after PSM
例(%), M(P25, P75) 指标 PSM前 P PSM后 P HFimpEF组(71例) non-HFimpEF组(158例) HFimpEF组(58例) non-HFimpEF组(58例) 男性 56(78.87) 119(75.32) 0.558 45(77.59) 44(75.86) 0.826 年龄/岁 59.00 (49.00,67.00) 64.00 (56.00,71.00) 0.003 62.50 (52.00,68.25) 60.50 (51.00,66.25) 0.466 高血压 30(42.25) 82(52.53) 0.177 25(43.10) 35(60.34) 0.063 糖尿病 24(33.80) 43(27.22) 0.311 17(29.31) 20(34.48) 0.550 慢性肾功能不全 11(15.49) 26(16.46) 0.855 11(18.97) 10(17.24) 0.809 吸烟 29(40.85) 66(41.77) 0.895 25(43.10) 25(43.10) 1.000 脑血管疾病 10(14.08) 33(20.89) 0.223 10(17.24) 13(22.41) 0.485 心房颤动 3(4.23) 3(1.90) 0.567 3(5.17) 1(1.72) 0.611 既往心肌梗死 39(54.93) 89(56.33) 0.844 33(56.90) 32(55.17) 0.852 NYHA分级>2 39(54.93) 87(55.06) 0.985 33(56.90) 31(53.45) 0.709 CRP/(mg/L) 2.80(0.80,7.70) 3.95(1.30,9.70) 0.052 2.90(0.90,7.75) 3.60(1.45,10.63) 0.183 LDL-C/(mmol/L) 1.78(1.61,2.51) 1.69(1.58,2.32) 0.201 1.78(1.61,2.38) 1.68(1.58,2.62) 0.384 NT-proBNP/(ng/L) 1502.00 (571.00,3478.00) 2201.00 (1220.50,4091.75) 0.020 1571.00 (564.75,3538.50) 2041.50 (901.00,3289.75) 0.476 LVEF/% 37.00 (33.00,38.00) 37.00 (34.00,39.00) 0.084 37.00 (34.00,38.00) 35.00 (31.00,37.00) 0.105 LVEDD/mm 59.00 (53.00,62.00) 60.00 (56.00,65.00) 0.019 59.00 (55.00,62.00) 59.00 (56.75,63.00) 0.636 J-CTO评分 1.00(0.00,2.00) 1.00(1.00,2.00) 0.022 1.00(0.00,2.00) 1.00(1.00,2.00) 0.089 CTO数量 1.00(1.00,1.00) 1.00(1.00,1.00) 0.370 1.00(1.00,1.00) 1.00(1.00,1.00) 0.328 LAD-CTO 41(57.75) 83(52.53) 0.464 33(56.90) 29(50.00) 0.457 LCX-CTO 13(18.31) 39(24.68) 0.287 10(17.24) 14(24.14) 0.359 RCA-CTO 27(38.03) 73(46.20) 0.249 22(37.93) 30(51.72) 0.135 侧支循环良好 65(91.55) 145(91.77) 0.955 53(91.38) 53(91.38) 1.000 ACEI/ARB/ARNI 64(90.14) 146(92.41) 0.566 52(89.66) 56(96.55) 0.272 β受体阻滞剂 67(94.37) 129(81.65) 0.011 54(93.10) 53(91.38) 1.000 呋塞米 67(94.37) 148(93.67) 1.000 54(93.10) 52(89.66) 0.508 螺内酯 70(98.59) 155(98.10) 1.000 57(98.28) 57(98.28) 1.000 洋地黄 23(32.39) 41(25.95) 0.315 20(34.48) 19(32.76) 0.844 SGLT2i 10(14.08) 7(4.43) 0.010 5(8.62) 6(10.34) 0.751 NYHA:纽约心功能分级;CRP:C反应蛋白;LDL-C:低密度脂蛋白胆固醇;LAD:前降支;LCX:回旋支;RCA:右冠脉;ACEI:血管紧张素转化酶抑制剂;ARB:血管紧张素受体拮抗剂;ARNI:血管紧张素受体脑啡肽酶抑制剂。 表 2 CTO-PCI术后HFimpEF的二分类logistic回归
Table 2. Binary logistic regression of HFimpEF after CTO-PCI
变量 单因素 P 多因素 P OR 95%CI OR 95%CI 年龄<60岁 1.873 1.062~3.306 0.030 2.024 1.104~3.709 0.023 NT-proBNP<2000 ng/L 1.675 0.951~2.948 0.074 LVEDD<60mm 2.121 1.193~3.771 0.010 2.127 1.157~3.912 0.015 J-CTO评分<3 3.148 1.053~9.417 0.040 3.257 1.047~10.130 0.041 β受体阻滞剂 3.766 1.271~11.158 0.017 4.129 1.343~12.697 0.013 SGLT2i 3.536 1.287~9.715 0.014 3.758 1.261~11.196 0.017 表 3 PSM前后两组结局事件的比较
Table 3. Outcome events in the HFimpEF and non-HFimpEF groups before and after PSM
例(%) 结局事件 PSM前 P PSM后 P HFimpEF组 non-HFimpEF组 HFimpEF组 non-HFimpEF组 MACE 15(21.13) 80(50.63) <0.001 12(20.69) 31(53.45) <0.001 心血管死亡 6(8.45) 49(31.01) <0.001 6(10.34) 16(27.59) 0.018 心衰再入院 9(12.68) 52(32.91) 0.001 7(12.07) 18(31.03) 0.013 非致死性心肌梗死 2(2.82) 7(4.43) 0.831 1(1.72) 6(10.34) 0.119 注:部分患者因心衰入院后继而出现心血管死亡,故子事件总和大于MACE事件数 表 4 PSM后MACE事件的Cox回归分析
Table 4. Cox regression analysis of MACE after PSM
指标 单因素 P 多因素 P HR 95%CI HR 95%CI 年龄 1.045 1.011~1.079 0.009 1.045 1.015~1.083 0.004 NT-proBNP 1.00013 1.00002~1.00023 0.016 1.00014 1.00003~1.00024 0.013 LVEF 0.914 0.859~0.973 0.005 0.914 0.850~0.982 0.015 β受体阻滞剂 0.357 0.150~0.851 0.020 0.169 0.064~0.442 <0.001 SGLT2i 0.132 0.018~0.974 0.047 0.078 0.010~0.591 0.014 HFimpEF 0.338 0.174~0.660 0.001 0.277 0.140~0.550 <0.001 -
[1] Fefer P, Knudtson ML, Cheema AN, et al. Current perspectives on coronary chronic total occlusions: the Canadian Multicenter Chronic Total Occlusions Registry[J]. J Am Coll Cardiol, 2012, 59(11): 991-997. doi: 10.1016/j.jacc.2011.12.007
[2] Tomasello SD, Boukhris M, Giubilato S, et al. Management strategies in patients affected by chronic total occlusions: results from the Italian Registry of Chronic Total Occlusions[J]. Eur Heart J, 2015, 36(45): 3189-3198. doi: 10.1093/eurheartj/ehv450
[3] Di Mario C, Mashayekhi KA, Garbo R, et al. Recanalisation of coronary chronic total occlusions[J]. Euro Intervention, 2022, 18(7): 535-561.
[4] 韩旭飞, 刘恒道, 邢军辉, 等. 单纯使用药物涂层球囊治疗冠状动脉慢性完全闭塞性病变的临床疗效分析[J]. 临床心血管病杂志, 2021, 37(7): 604-609. https://lcxxg.whuhzzs.com/article/doi/10.13201/j.issn.1001-1439.2021.07.004
[5] Galassi AR, Boukhris M, Toma A, et al. Percutaneous coronary intervention of chronic total occlusions in patients with low left ventricular ejection fraction[J]. JACC Cardiovasc Interv, 2017, 10(21): 2158-2170. doi: 10.1016/j.jcin.2017.06.058
[6] Gulati G, Udelson JE. Heart failure with improved ejection fraction: is it possible to escape one's past?[J]. JACC Heart Fail, 2018, 6(9): 725-733. doi: 10.1016/j.jchf.2018.05.004
[7] Wilcox JE, Fang JC, Margulies KB, et al. Heart failure with recovered left ventricular ejection fraction: JACC scientific expert panel[J]. J Am Coll Cardiol, 2020, 76(6): 719-734. doi: 10.1016/j.jacc.2020.05.075
[8] Ybarra LF, Rinfret S, Brilakis ES, et al. Definitions and clinical trial design principles for coronary artery chronic total occlusion therapies: CTO-ARC Consensus Recommendations[J]. Circulation, 2021, 143(5): 479-500. doi: 10.1161/CIRCULATIONAHA.120.046754
[9] Généreux P, Palmerini T, Caixeta A, et al. Quantification and impact of untreated coronary artery disease after percutaneous coronary intervention: the residual SYNTAX(Synergy Between PCI with Taxus and Cardiac Surgery)score[J]. J Am Coll Cardiol, 2012, 59(24): 2165-2174. doi: 10.1016/j.jacc.2012.03.010
[10] Bozkurt B, Coats A, Tsutsui H. Universal definition and classification of heart failure[J]. J Card Fail, 2021, 20: 110.
[11] Hoebers LP, Claessen BE, Elias J, et al. Meta-analysis on the impact of percutaneous coronary intervention of chronic total occlusions on left ventricular function and clinical outcome[J]. Int J Cardiol, 2015, 187: 90-96. doi: 10.1016/j.ijcard.2015.03.164
[12] Megaly M, Saad M, Tajti P, et al. Meta-analysis of the impact of successful chronic total occlusion percutaneous coronary intervention on left ventricular systolic function and reverse remodeling[J]. J Interv Cardiol, 2018, 31(5): 562-571. doi: 10.1111/joic.12538
[13] Werner GS, Martin-Yuste V, Hildick-Smith D, et al. A randomized multicentre trial to compare revascularization with optimal medical therapy for the treatment of chronic total coronary occlusions[J]. Eur Heart J, 2018, 39(26): 2484-2493. doi: 10.1093/eurheartj/ehy220
[14] Lee SW, Lee PH, Ahn JM, et al. Randomized trial evaluating percutaneous coronary intervention for the treatment of chronic total occlusion[J]. Circulation, 2019, 139(14): 1674-1683. doi: 10.1161/CIRCULATIONAHA.118.031313
[15] Mashayekhi K, Nührenberg TG, Toma A, et al. A randomized trial to assess regional left ventricular function after stent implantation in chronic total occlusion: The REVASC Trial[J]. JACC Cardiovasc Interv, 2018, 11(19): 1982-1991. doi: 10.1016/j.jcin.2018.05.041
[16] Abe M, Morimoto T, Morino Y, et al. Association between J-CTO score and long-term target lesion revascularization rate after successful chronic total coronary occlusion angioplasty(from the J-CTO Registry)[J]. Catheter Cardiovasc Interv, 2019, 93(6): 1025-1032. doi: 10.1002/ccd.28104
[17] Ye LF, Li XL, Wang SM, et al. Body mass index: an effective predictor of ejection fraction improvement in heart failure[J]. Front Cardiovasc Med, 2021, 8: 586240. doi: 10.3389/fcvm.2021.586240
[18] Y$\acute{a}$ñez-Bisbe L, Garcia-Elias A, Tajes M, et al. Aging impairs reverse remodeling and recovery of ventricular function after isoproterenol-induced cardiomyopathy[J]. Int J Mol Sci, 2021, 23(1): 110. doi: 10.3390/ijms23010110
[19] 孟利民, 谷国强. 慢性冠状动脉完全闭塞病变介入治疗并发症风险评估进展[J]. 临床心血管病杂志, 2021, 37(11): 979-982. https://lcxxg.whuhzzs.com/article/doi/10.13201/j.issn.1001-1439.2021.11.002
[20] Torii Y, Kusunose K, Hirata Y, et al. Left atrial strain associated with functional recovery in patients receiving optimal treatment for heart failure[J]. J Am Soc Echocardiogr, 2021, 34(9): 966-975.e962. doi: 10.1016/j.echo.2021.03.016
[21] Jia S, Li J, Zhang C, et al. Long-term prognosis of moderate to severe coronary artery calcification in patients undergoing percutaneous coronary intervention[J]. Circ J, 2020, 85(1): 50-58. doi: 10.1253/circj.CJ-20-0761
[22] Wang N, Fulcher J, Abeysuriya N, et al. Predictors of successful chronic total occlusion percutaneous coronary interventions: a systematic review and meta-analysis[J]. Heart, 2018, 104(6): 517-524. doi: 10.1136/heartjnl-2017-311986
[23] Ghimire A, Fine N, Ezekowitz JA, et al. Frequency, predictors, and prognosis of ejection fraction improvement in heart failure: an echocardiogram-based registry study[J]. Eur Heart J, 2019, 40(26): 2110-2117. doi: 10.1093/eurheartj/ehz233
[24] Li Q, Qiao Y, Tang J, et al. Frequency, predictors, and prognosis of heart failure with improved left ventricular ejection fraction: a single-centre retrospective observational cohort study[J]. ESC Heart Fail, 2021, 8(4): 2755-2764. doi: 10.1002/ehf2.13345
[25] Heidenreich PA, Bozkurt B, Aguilar D, et al. 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: Executive Summary: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines[J]. Circulation, 2022, 145(18): e876-e894.
[26] Park CS, Park JJ, Mebazaa A, et al. Characteristics, outcomes, and treatment of heart failure with improved ejection fraction[J]. J Am Heart Assoc, 2019, 8(6): e011077. doi: 10.1161/JAHA.118.011077
[27] McDonagh TA, Metra M, Adamo M, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure[J]. Eur Heart J, 2021, 42(36): 3599-3726. doi: 10.1093/eurheartj/ehab368
[28] McMurray JJV, Solomon SD, Inzucchi SE, et al. Dapagliflozin in patients with heart failure and reduced ejection fraction[J]. N Engl J Med, 2019, 381(21): 1995-2008. doi: 10.1056/NEJMoa1911303
[29] Packer M, Anker SD, Butler J, et al. Cardiovascular and renal outcomes with empagliflozin in heart failure[J]. N Engl J Med, 2020, 383(15): 1413-1424. doi: 10.1056/NEJMoa2022190
-




 下载:
下载: