Research progress of left bundle branch block associated with transcatheter aortic valve replacement
-
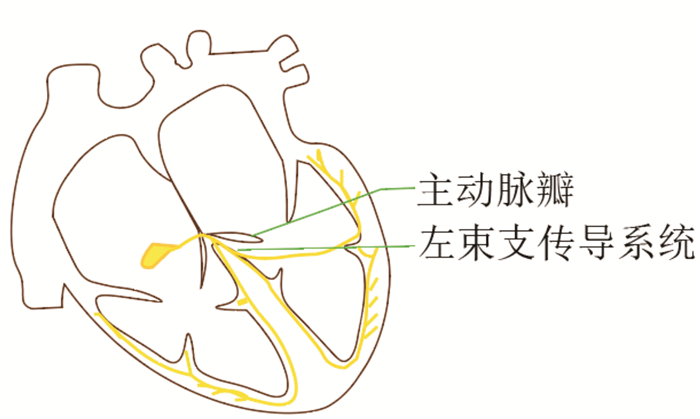
摘要: 左束支传导阻滞是经导管主动脉瓣置换术后最常见的传导障碍类型。术后新发持续性左束支传导阻滞可引起心室舒缩障碍,进展为高度房室传导阻滞时,常影响患者预后。永久起搏器植入术可作为经导管主动脉瓣置换术后新发持续性左束支传导阻滞的治疗方案,但其植入适应证尚需进一步临床论证。与左束支传导阻滞相关的传导系统起搏有望成为其主要治疗手段,但远期预后尚不明确。本文总结了经导管主动脉瓣置换术后左束支传导阻滞的相关因素、预后及治疗等方面的研究进展。
-
关键词:
- 经导管主动脉瓣置换术 /
- 左束支传导阻滞 /
- 治疗 /
- 预后
Abstract: Left bundle branch block is the most common type of conduction disorder after transcatheter aortic valve replacement. Postoperative persistent left bundle branch block can cause ventricular systolic and diastolic dysfunction, which often affects the prognosis of patients when it progresses to high atrioventricular block. Permanent pacemaker implantation is often used as a new treatment for persistent left bundle branch block after transcatheter aortic valve replacement, but its indication needs further clinical demonstration. The pacing of the conduction system related to the left bundle branch block is the fundamental treatment, but the long-term prognosis is still unclear. This article summarized the research progress in the related factors, prognosis, and treatment of left bundle branch block after transcatheter aortic valve replacement.-
Key words:
- transcatheter aortic valve replacement /
- left bundle branch block /
- treatment /
- prognosis
-

-
[1] Chamandi C, Barbanti M, Munoz-Garcia A, et al. Long-Term Outcomes in Patients With New-Onset Persistent Left Bundle Branch Block Following TAVR[J]. JACC Cardiovasc Interv, 2019, 12(12): 1175-1184. doi: 10.1016/j.jcin.2019.03.025
[2] 张文杰, 孟哲, 李黎, 等. 经导管主动脉瓣置入术后新发左束支传导阻滞危险因素分析及对左心室功能的影响[J]. 临床心血管病杂志, 2022, 38(6): 495-500. https://lcxxg.whuhzzs.com/article/doi/10.13201/j.issn.1001-1439.2022.06.013
[3] Sammour Y, Krishnaswamy A, Kumar A, et al. Incidence, Predictors, and Implications of Permanent Pacemaker Requirement After Transcatheter Aortic Valve Replacement[J]. JACC Cardiovasc Interv, 2021, 14(2): 115-134. doi: 10.1016/j.jcin.2020.09.063
[4] Faroux L, Chen S, Muntané-Carol G, et al. Clinical impact of conduction disturbances in transcatheter aortic valve replacement recipients: a systematic review and meta-analysis[J]. Eur Heart J, 2020, 41(29): 2771-2781. doi: 10.1093/eurheartj/ehz924
[5] 周达新, 潘文志, 吴永健, 等. 经导管主动脉瓣置换术中国专家共识(2020更新版)[J]. 中国介入心脏病学杂志, 2020, 28(6): 301-309. doi: 10.3969/j.issn.1004-8812.2020.06.001
[6] Nazif TM, Williams MR, Hahn RT, et al. Clinical implications of new-onset left bundle branch block after transcatheter aortic valve replacement: analysis of the PARTNER experience[J]. Eur Heart J, 2014, 35(24): 1599-1607. doi: 10.1093/eurheartj/eht376
[7] Isogai T, Dykun I, Agrawal A, et al. Early Resolution of New-Onset Left Bundle Branch Block After Transcatheter Aortic Valve Implantation With the SAPIEN 3 Valve[J]. Am J Cardiol, 2022, 168: 117-127. doi: 10.1016/j.amjcard.2021.12.032
[8] Auffret V, Puri R, Urena M, et al. Conduction Disturbances After Transcatheter Aortic Valve Replacement: Current Status and Future Perspectives[J]. Circulation, 2017, 136(11): 1049-1069. doi: 10.1161/CIRCULATIONAHA.117.028352
[9] Poels TT, Stassen R, Kats S, et al. Effective Distance between Aortic Valve and Conduction System Is an Independent Predictor of Persistent Left Bundle Branch Block during Transcatheter Aortic Valve Implantation[J]. Medicina(Kaunas), 2021, 57(5): 476.
[10] Syed FF, Hai JJ, Lachman N, et al. The infrahisian conduction system and endocavitary cardiac structures: relevance for the invasive electrophysiologist[J]. J Interv Card Electrophysiol, 2014, 39(1): 45-56. doi: 10.1007/s10840-013-9858-7
[11] Aktug Ö, Dohmen G, Brehmer K, et al. Incidence and predictors of left bundle branch block after transcatheter aortic valve implantation[J]. Int J Cardiol, 2012, 160(1): 26-30. doi: 10.1016/j.ijcard.2011.03.004
[12] Reiter C, Lambert T, Kellermair J, et al. Intraprocedural dynamics of cardiac conduction during transcatheter aortic valve implantation: Assessment by simultaneous electrophysiological testing[J]. Heart Rhythm, 2021, 18(3): 419-425. doi: 10.1016/j.hrthm.2020.10.018
[13] Keßler M, Gonska B, Seeger J, et al. Long-term clinical outcome of persistent left bundle branch block after transfemoral aortic valve implantation[J]. Catheter Cardiovasc Interv, 2019, 93(3): 538-544. doi: 10.1002/ccd.27850
[14] Regueiro A, Abdul-Jawad Altisent O, Del Trigo M, et al. Impact of New-Onset Left Bundle Branch Block and Periprocedural Permanent Pacemaker Implantation on Clinical Outcomes in Patients Undergoing Transcatheter Aortic Valve Replacement: A Systematic Review and Meta-Analysis[J]. Circ Cardiovasc Interv, 2016, 9(5): e003635. doi: 10.1161/CIRCINTERVENTIONS.115.003635
[15] Shiyovich A, Kornowski R, Plakht Y, et al. Increased Rate of New-onset Left Bundle Branch Block in Patients With Bicuspid Aortic Stenosis Undergoing Transcatheter Aortic Valve Implantation(From a National Registry)[J]. Am J Cardiol, 2021, 156: 101-107. doi: 10.1016/j.amjcard.2021.06.046
[16] Hamdan A, Nassar M, Schwammenthal E, et al. Short membranous septum length in bicuspid aortic valve stenosis increases the risk of conduction disturbances[J]. J Cardiovasc Comput Tomogr, 2021, 15(4): 339-347. doi: 10.1016/j.jcct.2020.10.002
[17] Singh A, Musa TA, Treibel TA, et al. Sex differences in left ventricular remodelling, myocardial fibrosis and mortality after aortic valve replacement[J]. Heart, 2019, 105(23): 1818-1824. doi: 10.1136/heartjnl-2019-314987
[18] Ponnusamy SS, Vijayaraman P. Left Bundle Branch Block-Induced Cardiomyopathy: Insights From Left Bundle Branch Pacing[J]. JACC Clin Electrophysiol, 2021, 7(9): 1155-1165. doi: 10.1016/j.jacep.2021.02.004
[19] Chamandi C, Barbanti M, Munoz-Garcia A, et al. Long-Term Outcomes in Patients With New-Onset Persistent Left Bundle Branch Block Following TAVR[J]. JACC Cardiovasc Interv, 2019, 12(12): 1175-1184. doi: 10.1016/j.jcin.2019.03.025
[20] Wang J, Liu S, Han X, et al. Prognostic Outcome of New-Onset Left Bundle Branch Block After Transcatheter Aortic Valve Replacement in Patients With Aortic Stenosis: A Systematic Review and Meta-Analysis[J]. Front Cardiovasc Med, 2022, 9: 842929. doi: 10.3389/fcvm.2022.842929
[21] Akdemir B, Roukoz H. A single-centre cohort and short-term follow-up of patients who developed persistent new onset left bundle branch block after transcatheter aortic valve replacement[J]. Acta Cardiol, 2020, 75(4): 360-365. doi: 10.1080/00015385.2020.1713520
[22] Schlömicher M, Useini D, Haldenwang PL, et al. Outcomes in Patients with Left Bundle Branch Block after Rapid Deployment Aortic Valve Replacement[J]. Thorac Cardiovasc Surg, 2023, 71(7): 528-534. doi: 10.1055/s-0042-1742361
[23] Glikson M, Nielsen JC, Kronborg MB, et al. 2021 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy[J]. Eur Heart J, 2021, 42(35): 3427-3520.
[24] Viskin D, Halkin A, Sherez J, et al. Heart Failure Due to High-Degree Atrioventricular Block: How Frequent Is It and What Is the Cause?[J]. Can J Cardiol, 2021, 37(10): 1562-1568. doi: 10.1016/j.cjca.2021.05.007
[25] El-Sabawi B, Welle GA, Cha YM, et al. Temporal Incidence and Predictors of High-Grade Atrioventricular Block After Transcatheter Aortic Valve Replacement[J]. J Am Heart Assoc, 2021, 10(10): e020033. doi: 10.1161/JAHA.120.020033
[26] Urena M, Mok M, Serra V, et al. Predictive factors and long-term clinical consequences of persistent left bundle branch block following transcatheter aortic valve implantation with a balloon-expandable valve[J]. J Am Coll Cardiol, 2012, 60(18): 1743-1752. doi: 10.1016/j.jacc.2012.07.035
[27] Auberson C, Badertscher P, Madaffari A, et al. Non-invasive predictors for infranodal conduction delay in patients with left bundle branch block after TAVR[J]. Clin Res Cardiol, 2021, 110(12): 1967-1976. doi: 10.1007/s00392-021-01924-w
[28] Jørgensen TH, Thyregod H, Ihlemann N, et al. Eight-year outcomes for patients with aortic valve stenosis at low surgical risk randomized to transcatheter vs. surgical aortic valve replacement[J]. Eur Heart J, 2021, 42(30): 2912-2919. doi: 10.1093/eurheartj/ehab375
[29] Moat NE, Ludman P, de Belder MA, et al. Long-term outcomes after transcatheter aortic valve implantation in high-risk patients with severe aortic stenosis: the U. K. TAVI(United Kingdom Transcatheter Aortic Valve Implantation)Registry[J]. J Am Coll Cardiol, 2011, 58(20): 2130-2138. doi: 10.1016/j.jacc.2011.08.050
[30] Khan MZ, Gupta A, Franklin S, et al. Predictors of Early and Late Atrioventricular Block Requiring Permanent Pacemaker Implantation After Transcatheter Aortic Valve Replacement: A Single-Center Experience[J]. Cardiovasc Revasc Med, 2022, 42: 67-71. doi: 10.1016/j.carrev.2022.02.002
[31] Elchinova E, Nozica N, Bartkowiak J, et al. Permanent pacemaker implantation late after transcatheter aortic valve implantation[J]. Heart Rhythm, 2021, 18(12): 2033-2039. doi: 10.1016/j.hrthm.2021.08.010
[32] Mirolo A, Viart G, Durand E, et al. Pacemaker memory in post-TAVI patients: Who should benefit from permanent pacemaker implantation?[J]. Pacing Clin Electrophysiol, 2018, 41(9): 1178-1184. doi: 10.1111/pace.13422
[33] Glikson M, Nielsen JC, Kronborg MB, et al. 2021 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy[J]. Europace, 2022, 24(1): 71-164.
[34] Poels TT, Engels EB, Kats S, et al. Occurrence and Persistency of Conduction Disturbances during Transcatheter Aortic Valve Implantation[J]. Medicina(Kaunas), 2021, 57(7): 695.
[35] Wu S, Chen X, Wang S, et al. Evaluation of the Criteria to Distinguish Left Bundle Branch Pacing From Left Ventricular Septal Pacing[J]. JACC Clin Electrophysiol, 2021, 7(9): 1166-1177. doi: 10.1016/j.jacep.2021.02.018
[36] Zhang S, Zhou X, Gold M R. Left Bundle Branch Pacing: JACC Review Topic of the Week[J]. J Am Coll Cardiol, 2019, 74(24): 3039-3049. doi: 10.1016/j.jacc.2019.10.039
[37] 马博斐, 谢瑞芹. 希氏束及其束支起搏治疗进展[J]. 中华心律失常学杂志, 2019, 23(2): 115-119. doi: 10.3760/cma.j.issn.1007-6638.2019.02.005
[38] 严霜霜, 熊峰, 张丽娟, 等. 二维斑点追踪技术评价左束支区域起搏早期右心室收缩功能及同步性[J]. 临床心血管病杂志, 2022, 38(7): 561-565. https://lcxxg.whuhzzs.com/article/doi/10.13201/j.issn.1001-1439.2022.07.009
[39] Hua J, Chen Y, Yu J, et al. Long-term outcomes of left bundle branch area pacing versus biventricular pacing in patients with heart failure and complete left bundle branch block[J]. Heart Vessels, 2022, 37(7): 1162-1174. doi: 10.1007/s00380-021-02016-5
[40] Liu W, Hu C, Wang Y, et al. Mechanical Synchrony and Myocardial Work in Heart Failure Patients With Left Bundle Branch Area Pacing and Comparison With Biventricular Pacing[J]. Front Cardiovasc Med, 2021, 8: 727611.
[41] Zhang J, Li F, Zhang ZY, et al. Conduction system pacing is superior to biventricular pacing in patients with heart failure: Insights from the pooled clinical studies[J]. Front Physiol, 2023, 14: 1125340. doi: 10.3389/fphys.2023.1125340
[42] Gui Y, Ye L, Wu L, et al. Clinical Outcomes Associated With His-Purkinje System Pacing vs. Biventricular Pacing, in Cardiac Resynchronization Therapy: A Meta-Analysis[J]. Front Cardiovasc Med, 2022, 9: 707148. doi: 10.3389/fcvm.2022.707148
[43] Guo J, Li L, Xiao G, et al. Feasibility and stability of left bundle branch pacing in patients after prosthetic valve implantation[J]. Clin Cardiol, 2020, 43(10): 1110-1118.
[44] Su L, Wang S, Wu S, et al. Long-Term Safety and Feasibility of Left Bundle Branch Pacing in a Large Single-Center Study[J]. Circ Arrhythm Electrophysiol, 2021, 14(2): e009261. doi: 10.1161/CIRCEP.120.009261
[45] Fan L, Choy JS, Raissi F, et al. Optimization of cardiac resynchronization therapy based on a cardiac electromechanics-perfusion computational model[J]. Comput Biol Med, 2022, 141: 105050.
[46] McDonagh TA, Metra M, Adamo M, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure[J]. Eur Heart J, 2021, 42(36): 3599-3726.
[47] Jastrzebski M, Baranchuk A, Fijorek K, et al. Cardiac resynchronization therapy-induced acute shortening of QRS duration predicts long-term mortality only in patients with left bundle branch block[J]. Europace, 2019, 21(2): 281-289.
[48] Zhang S, Shan Q. Discussion of LBBP synchronization effects in HF patients with LBBB and comparison with BiV-CRT[J]. Heart Fail Rev, 2022, 27(6): 2181-2186.
-




 下载:
下载: