Effect factors of the death in heart failure with mildly reduced ejection fraction and establishment of predictive model
-
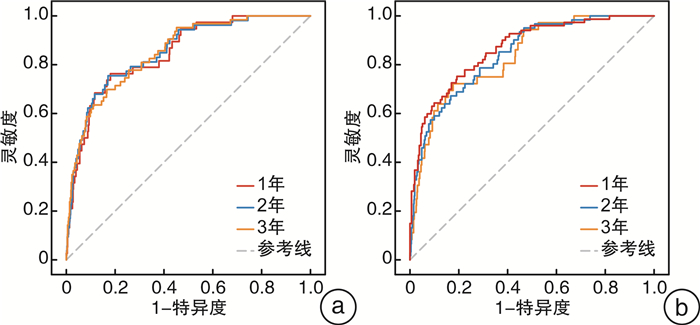
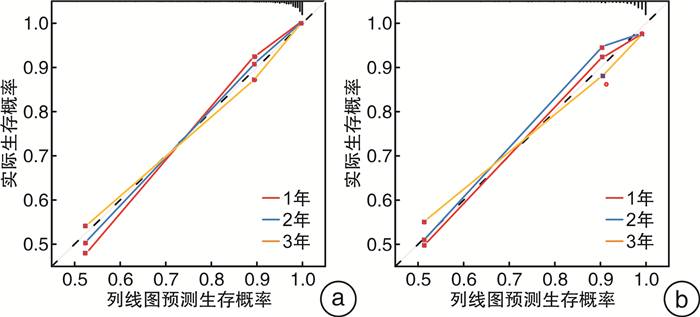
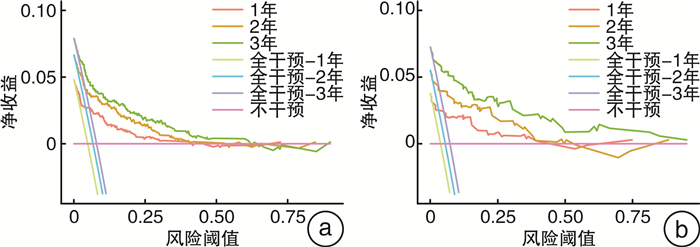
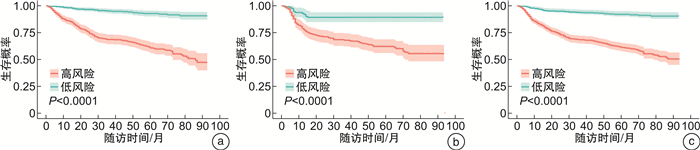
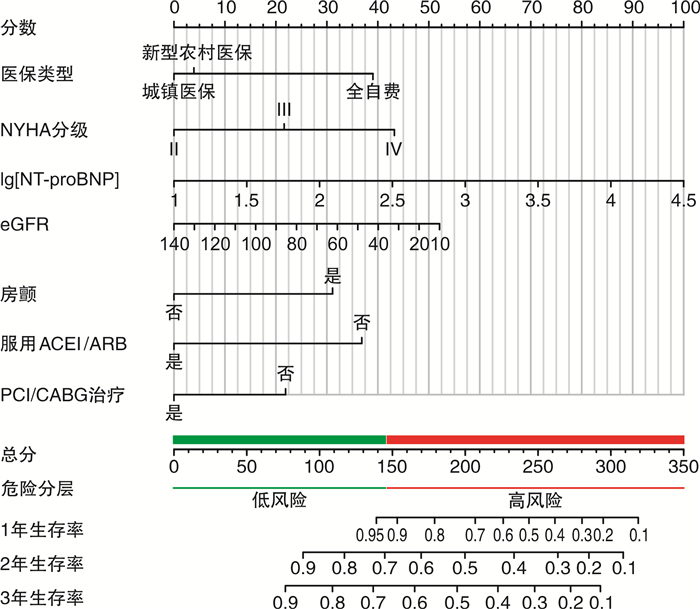
摘要: 目的 探讨射血分数轻度降低的心力衰竭(HFmrEF)全因死亡的影响因素,通过长期随访数据构建列线图模型,用于预测患者1年、2年、3年期的全因死亡率。方法 顺序入选2014年4月—2019年3月山西省3所三级甲等医院诊治的慢性心力衰竭且射血分数为41%~49%的患者1 148例进行随访,以全因死亡为终点事件,随访截止日期为2022年4月1日。将所有研究对象按7:3比例随机分为训练集和验证集,训练集用于模型的构建,验证集用于模型性能的评估。利用Cox回归分析患者全因死亡的影响因素,R 4.3.1用于构建列线图预测模型。采用一致性指数(C-index)、受试者工作特征曲线下面积(AUC)和校正曲线评价模型的区分度和预测性能,通过临床决策曲线(DCA)评估模型的临床潜在应用价值。根据ROC曲线确定的最佳截断阈值对患者进行死亡风险分层,并采用Kaplan-Meier曲线比较高风险组和低风险组患者之间的生存差异。结果 多因素Cox回归分析显示,住院费用全自付(HR=4.722,95%CI:2.544~8.765)、入院NYHA心功能Ⅳ级(HR=2.982,95%CI:1.507~5.898)、N末端脑钠肽前体(对数值)[lg(NT-proBNP)]水平升高(HR=2.360,95%CI:1.414~3.938)、合并心房颤动(HR=2.321,95%CI:1.419~3.797)增加患者全因死亡风险;高估算肾小球滤过率(eGFR)水平(HR=0.984,95%CI:0.973~0.995)、服用血管紧张素转换酶抑制剂/血管紧张素Ⅱ受体拮抗剂(ACEI/ARB)药物(HR=0.320,95%CI:0.191~0.535)及接受经皮冠状动脉介入治疗/冠状动脉旁路移植术(PCI/CABG)治疗(HR=0.503,95%CI:0.264~0.958)降低患者全因死亡风险。依此构建的列线图模型经测试集验证,C-index为0.839,1年、2年、3年生存期预测模型的AUC分别为0.864、0.860、0.857。校正曲线和DCA曲线结果显示,模型预测效果和实际生存情况拟合度较好,具有较好的临床适用性。风险分层能够有效区分高、低危患者的预后。结论 基于医保类型、NYHA心功能分级、NT-proBNP、eGFR、心房颤动、ACEI/ARB类药物及PCI/CABG治疗7个因素构建的列线图预测模型有助于高风险HFmrEF患者早期识别与治疗决策指导。
-
关键词:
- 射血分数轻度降低的心力衰竭 /
- 全因死亡 /
- 影响因素 /
- 列线图 /
- 预测模型
Abstract: Objective To explore the effect factors of the death of heart failure with mildly reduced ejection fraction(HFmrEF), and to construct a nomogram model based on long-term follow-up data to predict the all-cause mortality of patients at 1 year, 2 years and 3 years.Methods A total of 1148 patients with chronic heart failure and ejection fraction of 41%-49% who were diagnosed and treated in three tertiary-level A hospitals in Shanxi Province from April 2014 to March 2019 were sequentially enrolled for follow-up, with all-cause death as the endpoint event, and the deadline for follow-up was April 1, 2022. All study subjects were randomly divided into a training set and a validation set in a 7: 3 ratio; the training set was used for model construction, and the validation set was used for model performance evaluation. Cox regression was used to analyze the factors influencing all-cause mortality in patients, and R 4.3. 1 was used to construct the column-line graph prediction model. The consistency index(C-index), the area under the working curve(AUC) of subjects, and calibration curves were used to evaluate the discriminatory and predictive performance of the model, and the clinical potential application value of the model was assessed by the clinical decision curve(DCA). Based on the optimal cut-off threshold determined by the ROC curve, the patients were stratified by death risk, and the Kaplan-Meier curves were used to compare the survival differences between the patients in the high-risk and low-risk groups.Results Multifactorial Cox regression analysis showed that self-paying(HR=4.722, 95%CI: 2.544 to 8.765), admission the New York Heart Association class Ⅳ(HR=2.982, 95%CI: 1.507 to 5.898), elevated of N-terminal brain natriuretic peptide precursor(Logarithmic value) [lg(NT-proBNP)]levels(HR=2.360 with 95%CI: 1.414 to 3.938), and combined atrial fibrillation(HR=2.321, 95%CI: 1.419 to 3.797) increased the risk of all-cause mortality in patients; high estimated glomerular filtration rate(eGFR) levels(HR=0.984, 95%CI: 0.973 to 0.995), and the use of angiotensin-converting enzyme inhibitors or angiotensin receptor antagonist(ACEI/ARB) medications(HR=0.320, 95%CI: 0.191~0.535) and receiving percutaneous coronary intervention or coronary artery bypass grafting(PCI/CABG) treatments(HR=0.503, 95%CI: 0.264~0.958) reduced the risk of all-cause mortality in patients. The C-index of the column-line graph model constructed accordingly was 0.839, and the AUCs of the 1-, 2-, and 3-year survival prediction models were 0.864, 0.860, and 0.857, respectively, and the calibration curves suggested that the model prediction effect was basically in line with the actual survival situation, and the DCA curves indicated that the model had good clinical applicability. Risk stratification can effectively distinguish the prognosis of high-and low-risk patients.Conclusion Based on these 7 factors(medical insurance type, NYHA classification, NT-proBNP, eGFR, atrial fibrillation, ACEI/ARB drugs, and PCI/CABG treatment), the nomogram is helpful for the early identification and treatment decision-making guidance of high-risk HFmrEF patients. -

-
表 1 两组患者基线资料的比较
Table 1. basic data between two groups
例(%), M(P25, P75) 项目 存活组(1 037例) 死亡组(111例) χ2/Z P值 一般资料 年龄/岁 67(59,76) 76(69,81) -7.526 < 0.001 男性 747(72.03) 68(61.26) 5.651 0.017 职业 12.413 < 0.001 体力劳动 369(35.58) 21(18.92) 非体力劳动 668(64.42) 90(81.08) 医保类型 13.954 < 0.001 城镇医保 636(61.33) 70(63.06) 新型农村合作医保 298(28.74) 19(17.12) 全自费 103(9.93) 22(19.82) 吸烟史 11.851 < 0.001 未吸烟 385(37.13) 23(20.72) 戒烟 148(14.27) 21(18.92) 吸烟 504(48.60) 67(60.36) 饮酒史 270(26.04) 18(16.22) 5.145 0.023 NYHA心功能分级 63.941 < 0.001 Ⅱ 453(43.68) 22(19.82) Ⅲ 394(38.00) 33(29.73) Ⅳ 190(18.32) 56(50.45) 心率/(次/min) 73(66,81) 73(68,80) -0.493 0.622 收缩压/mmHg△ 130(116,140) 130(112,149) -0.798 0.425 舒张压/mmHg 80(70,85) 78(68,85) -0.822 0.411 体重指数/(kg/m2) 24.28(22.23,26.93) 23.59(20.93,25.59) -2.982 0.073 合并症 糖尿病 337(32.50) 41(36.94) 0.895 0.344 高血压 601(57.96) 77(69.37) 5.402 0.020 心脏瓣膜病 83(8.00) 15(13.51) 3.898 0.048 冠状动脉粥样硬化性心脏病 831(80.14) 87(78.38) 0.193 0.660 COPD 180(17.36) 33(29.73) 10.156 < 0.001 脑卒中 210(20.26) 47(42.34) 28.164 < 0.001 肾功能不全 105(10.13) 25(22.52) 15.346 < 0.001 房颤 229(22.08) 56(50.45) 43.235 < 0.001 实验室指标 lg(NT-proBNP)/(pg/mL) 3.03(2.67,3.43) 3.51(3.25,3.81) -9.328 < 0.001 胱抑素C/(mg/L) 1.11(0.98,1.40) 1.30(1.08,1.79) -4.743 < 0.001 eGFR/[mL/min/(1.73m2)] 90.70(72.87,109.29) 67.17(51.43,84.91) -8.012 < 0.001 尿酸/(μmol/L) 370(314,435) 393(329,474) -2.070 0.038 血清总胆固醇/(mmol/L) 4.04(3.38,4.81) 4.04(3.36,4.79) -0.158 0.875 甘油三酯/(mmol/L) 1.41(1.04,1.85) 1.33(1.01,1.76) -1.184 0.236 HDL-C/(mmol/L) 0.99(0.84,1.14) 0.99(0.84,1.15) -0.282 0.778 LDL-C/(mmol/L) 2.43(1.93,3.05) 2.44(1.88,3.09) -0.115 0.908 红细胞分布宽度/% 13.94(13.40,14.70) 14.50(13.90,15.45) -5.122 < 0.001 血红蛋白/(g/L) 137(125,149) 132(118,142) -3.815 < 0.001 ALT/(U/L) 20.80(14.00,33.00) 18.00(12.00,25.00) -3.055 0.052 AST/(U/L) 27.00(21.00,41.00) 24.87(20.00,35.79) -1.839 0.066 白蛋白/(g/L) 43.00(40.00,46.00) 40.30(37.15,43.20) -5.147 < 0.001 血清总胆红素/(mmol/L) 14.70(11.20,19.36) 15.95(11.40,20.48) -1.046 0.295 血钾/(mmol/L) 4.07(3.82,4.34) 4.11(3.79,4.42) -0.694 0.487 血钠/(mmol/L) 139.00(138.00,141.00) 139.00(137.50,141.50) -0.078 0.938 心电图 QRS间期/ms 98(90,112) 98(90,115) -0.960 0.337 QTC间期/ms 440(418,468) 448(422,477) -1.721 0.085 心脏彩超 室间隔厚度/mm 9(8,11) 10(9,11) -1.801 0.072 左室舒张末期内径/mm 56(52,59) 55(51,59) -0.345 0.730 左室后壁厚度/mm 9(9,10) 9(8,11) -0.750 0.453 左室射血分数/% 45(43,47) 44(42,46) -1.424 0.155 治疗情况 抗血小板药物 957(92.29) 94(84.68) 7.488 0.006 硝酸酯类药物 705(67.98) 77(69.37) 0.089 0.766 β受体阻滞剂 246(23.72) 22(19.82) 0.853 0.356 ACEI/ARB 609(58.73) 27(24.32) 48.029 < 0.001 他汀类药物 961(92.67) 96(86.49) 5.255 0.022 利尿剂 833(80.33) 91(81.98) 0.175 0.676 正性肌力药物 120(11.57) 17(15.32) 1.337 0.248 PCI/CABG 376(36.26) 14(12.61) 24.993 < 0.001 注:△1 mmHg=0.133 kPa。COPD:慢性阻塞性肺疾病;HDL-C:高密度脂蛋白胆固醇;LDL-C:低密度脂蛋白胆固醇;ALT:丙氨酸氨基转移酶;AST:门冬氨酸氨基转移酶。 表 2 HFmrEF患者全因死亡影响因素的单因素和多因素Cox回归分析
Table 2. Univariate and multivariate Cox regression analysis of influencing factors of all-cause mortality in patients with HFmrEF
变量 单因素Cox回归分析 多因素Cox回归分析 HR 95%CI P HR 95%CI P 年龄 1.059 1.035~1.083 < 0.001 男性 0.649 0.442~0.953 0.027 职业:体力劳动 1.796 1.058~3.048 0.003 医保类型 城镇医保 参考值 参考值 新型农村医疗合作医保 0.672 0.374~1.208 0.184 1.519 0.690~3.345 0.299 全自费 2.137 1.200~3.714 0.008 4.722 2.544~8.765 < 0.001 吸烟史 未吸烟 参考值 戒烟 1.090 0.493~2.408 0.832 吸烟 1.167 0.980~2.835 0.059 饮酒史 0.551 0.291~1.043 0.067 NYHA心功能分级 Ⅱ 参考值 Ⅲ 1.716 0.911~3.230 0.094 1.569 0.816~3.015 0.177 Ⅳ 5.294 2.935~9.550 < 0.001 2.982 1.507~5.898 0.002 lg(NT-proBNP) 4.924 3.258~7.441 < 0.001 2.360 1.414~3.938 0.001 eGFR 0.976 0.968~0.985 < 0.001 0.984 0.973~0.995 0.006 胱抑素C 1.164 1.008~1.344 0.039 血红蛋白 0.985 0.975~0.995 0.002 红细胞分布宽度 1.089 1.015~1.167 0.017 白蛋白 0.958 0.932~0.985 0.003 高血压 1.313 0.313~2.118 0.265 心脏瓣膜病 1.571 0.755~3.270 0.227 房颤 3.609 2.300~5.663 < 0.001 2.321 1.419~3.797 0.001 COPD 2.526 1.729~3.690 < 0.001 脑卒中 2.015 1.337~3.038 0.001 肾功能不全 2.535 1.620~3.967 < 0.001 抗血小板药物 0.426 0.230~0.790 0.007 ACEI/ARB 0.304 0.187~0.497 < 0.001 0.320 0.191~0.535 < 0.001 他汀类药物 0.513 0.264~0.997 0.049 PCI/CABG 0.345 0.186~0.639 0.001 0.503 0.264~0.958 0.037 -
[1] Mcdonagh TA, Metra M, Adamo M, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure[J]. Euro Heart J, 2021, 42(36): 3599-3726. doi: 10.1093/eurheartj/ehab368
[2] Zhang Y, Zhang J, Butler J, et al. Contemporary epidemiology, management, and outcomes of patients hospitalized for heart failure in China: Results From the China Heart Failure(China-HF)Registry[J]. J Cardiac fail, 2017, 23(12): 868-875. doi: 10.1016/j.cardfail.2017.09.014
[3] 王华, 刘宇佳, 杨杰孚. 心力衰竭流行病学[J]. 临床心血管病杂志, 2023, 39(4): 243-247. https://lcxxg.whuhzzs.com/article/doi/10.13201/j.issn.1001-1439.2023.04.001
[4] Taylor CJ, Ordonez-mena JM, Roalfe AK, et al. Trends in survival after a diagnosis of heart failure in the United Kingdom 2000-2017: population based cohort study[J]. BMJ, 2019, 364: 1223.
[5] Metra M, Teerlink JR. Heart failure[J]. The Lancet, 2017, 390(10106): 1981-1995. doi: 10.1016/S0140-6736(17)31071-1
[6] Wang Z, Yao L, Li D, et al. Mortality prediction system for heart failure with orthogonal relief and dynamic radius means[J]. Int J Med Info, 2018, 115: 10-17. doi: 10.1016/j.ijmedinf.2018.04.003
[7] Gao Y, Bai X, Lu J, et al. Prognostic value of multiple circulating biomarkers for 2-year death in acute heart failure with preserved ejection fraction[J]. Front Cardiovasc Med, 2021, 8: 779282. doi: 10.3389/fcvm.2021.779282
[8] Kasahara S, Sakata Y, Nochioka K, et al. The 3A3B score: The simple risk score for heart failure with preserved ejection fraction-A report from the CHART-2 Study[J]. Inter J Cardiol, 2019, 284: 42-49. doi: 10.1016/j.ijcard.2018.10.076
[9] 周浩斌, 安冬琪, 詹琼, 等. 不同射血分数心力衰竭患者临床特征和预后回顾性分析[J]. 中华内科杂志, 2017, 56(4): 253-257. doi: 10.3760/cma.j.issn.0578-1426.2017.04.003
[10] Abdul-Rahim AH, Shen L, Rush CJ, et al. Effect of digoxin in patients with heart failure and mid-range(borderline)left ventricular ejection fraction[J]. Euro J Heart fail, 2018, 20(7): 1139-1145. doi: 10.1002/ejhf.1160
[11] Hsu JJ, Ziaeian B, Fonarow GC. Heart failure with mid-range(Borderline)ejection fraction: clinical implications and future directions[J]. JACC Heart Fail, 2017, 5(11): 763-771. doi: 10.1016/j.jchf.2017.06.013
[12] Savarese G, Stolfo D, Sinagra G, et al. Heart failure with mid-range or mildly reduced ejection fraction[J]. Nat Rev Cardiol, 2022, 19(2): 100-116. doi: 10.1038/s41569-021-00605-5
[13] 贾盈盈, 崔念奇, 胡欢婷, 等. 中国心力衰竭患者死亡风险预测模型的系统评价[J]. 中国循环杂志, 2023, 38(10): 1036-1041. doi: 10.3969/j.issn.1000-3614.2023.10.006
[14] Dunlay SM, Roger VL, Redfield MM. Epidemiology of heart failure with preserved ejection fraction[J]. Nat Rev Cardiol, 2017, 14(10): 591-602. doi: 10.1038/nrcardio.2017.65
[15] 国家心血管病中心, 国家心血管病专家委员会心力衰竭专业委员会, 中国医师协会心力衰竭专业委员会, 等. 国家心力衰竭指南2023(精简版)[J]. 中华心力衰竭和心肌病杂志, 2023, 7(3): 139-172. https://www.cnki.com.cn/Article/CJFDTOTAL-ZGXH202312011.htm
[16] Angraal S, Mortazavi BJ, Gupta A, et al. Machine Learning Prediction of Mortality and Hospitalization in Heart Failure With Preserved Ejection Fraction[J]. JACC Heart Fail, 2020, 8(1): 12-21. doi: 10.1016/j.jchf.2019.06.013
[17] Nahm FS. Receiver operating characteristic curve: overview and practical use for clinicians[J]. Korean J Anesthesiol, 2022, 75(1): 25-36. doi: 10.4097/kja.21209
[18] 陈红珍, 刘幸娟, 郝琦等. 急性ST段抬高型心肌梗死介入治疗前并发心室颤动的预测模型构建[J]. 临床心血管病杂志, 2023, 39(11): 870-875. https://lcxxg.whuhzzs.com/article/doi/10.13201/j.issn.1001-1439.2023.11.010
[19] Bonsu KO, Owusu IK, Buabeng KO, et al. Clinical characteristics and prognosis of patients admitted for heart failure: A 5-year retrospective study of African patients[J]. Int J Cardiol, 2017, 238: 128-135. doi: 10.1016/j.ijcard.2017.03.014
[20] Rickenbacher P, Kaufmann BA, Maeder MT, et al. Heart failure with mid-range ejection fraction: a distinct clinical entity? Insights from the Trial of Intensified versus standard Medical therapy in Elderly patients with Congestive Heart Failure(TIME-CHF)[J]. Eur J Heart Fail, 2017, 19(12): 1586-1596. doi: 10.1002/ejhf.798
[21] Spinar J, Spinarova L, Malek F, et al. Prognostic value of NT-proBNP added to clinical parameters to predict two-year prognosis of chronic heart failure patients with mid-range and reduced ejection fraction-A report from FAR NHL prospective registry[J]. Plos One, 2019, 14(3): e0214363. doi: 10.1371/journal.pone.0214363
[22] Han Q, Ren J, Tian J, et al. A nomogram based on a patient-reported outcomes measure: predicting the risk of readmission for patients with chronic heart failure[J]. Health Qual Life Outcomes, 2020, 18(1): 290. doi: 10.1186/s12955-020-01534-6
[23] Tian J, Yan J, Zhang Q, et al. Analysis of re-hospitalizations for patients with heart failure caused by coronary heart disease: data of first event and recurrent event[J]. Therap Clin Risk Man, 2019, 15: 1333-1341. doi: 10.2147/TCRM.S218694
[24] Guisado-Espartero ME, Salamanca B, Aramburu-Bodas ó, et al. Heart failure with mid-range ejection fraction in patients admitted to internal medicine departments: Findings from the RICA Registry[J]. Int J Cardiol, 2018, 255: 124-128. doi: 10.1016/j.ijcard.2017.07.101
[25] Santner V, Riepl HS, Posch F, et al. Non-eligibility for pivotal HFpEF/HFmrEF outcome trials and mortality in a contemporary heart failure cohort[J]. Euro J Int Med, 2023, 118: 73-81. doi: 10.1016/j.ejim.2023.07.027
[26] Ostrominski JW, Vaduganathan M, Selvaraj S, et al. Dapagliflozin and apparent treatment-resistant hypertension in heart failure with mildly reduced or preserved ejection fraction: The DELIVER Trial[J]. Circulation, 2023, 148(24): 1945-1957. doi: 10.1161/CIRCULATIONAHA.123.065254
[27] Schupp T, Abumayyaleh M, Weidner K, et al. Prognostic implications of Type 2 diabetes mellitus in heart failure with mildly reduced ejection fraction[J]. J Clin Med, 2024, 13(3): 742. doi: 10.3390/jcm13030742
[28] Ostrominski JW, Thierer J, Claggett BL, et al. Cardio-renal-metabolic overlap, outcomes, and dapagliflozin in heart failure with mildly reduced or preserved ejection fraction[J]. JACC Heart Fail, 2023, 11(11): 1491-1503. doi: 10.1016/j.jchf.2023.05.015
[29] Wang Z, Jin L, Zhou W, et al. A single-center observational study on the efficacy of percutaneous coronary intervention for ischemic heart failure: A cohort study[J]. Medicine, 2018, 97(13): e0238. doi: 10.1097/MD.0000000000010238
[30] 王星, 高路, 史慧婷, 等. 经皮冠状动脉介入治疗和左室射血分数恢复对慢性完全闭塞合并射血分数轻度降低的心力衰竭患者预后的影响[J]. 临床心血管病杂志, 2023, 39(4): 276-281. https://lcxxg.whuhzzs.com/article/doi/10.13201/j.issn.1001-1439.2023.04.009
[31] Ybarra LF, Rinfret S. Why and how should we treat chronic total occlusion? evolution of state-of-the-art methods and future directions[J]. Can J Cardiol, 2022, 38(10): S42-S53. doi: 10.1016/j.cjca.2020.10.005
[32] Pocock SJ, Wang D, Pfeffer MA, et al. Predictors of mortality and morbidity in patients with chronic heart failure[J]. Eur Heart J, 2006, 27(1): 65-75. doi: 10.1093/eurheartj/ehi555
[33] Meta-analysis Global Group in Chronic Heart Failure(MAGGIC). The survival of patients with heart failure with preserved or reduced left ventricular ejection fraction: an individual patient data meta-analysis[J]. Eur Heart J, 2012, 33(14): 1750-1757. doi: 10.1093/eurheartj/ehr254
[34] Zhao H, Li P, Zhong G, et al. Machine learning models in heart failure with mildly reduced ejection fraction patients[J]. Front Cardiovasc Med, 2022, 9: 1042139. doi: 10.3389/fcvm.2022.1042139
[35] Han Q, Ren J, Tian J, et al. A nomogram based on a patient-reported outcomes measure: predicting the risk of readmission for patients with chronic heart failure[J]. Health Qual Life Outcomes, 2020, 18(1): 290. doi: 10.1186/s12955-020-01534-6
-

计量
- 文章访问数: 329
- 施引文献: 0



 下载:
下载: